75 Cardiovascular Effects of Air Pollutants
Risk factors for atherosclerotic coronary artery disease—including hypertension, lipid abnormalities, diabetes mellitus, obesity, physical inactivity, and tobacco use—provide targets for the prevention or progression of heart disease (see Chapters 46, 61, 65, 70, 73, and 74). Yet these risk factors account for only approximately 50% to 75% of cases of ischemic heart disease and cardiac events. For this reason it is logical to assume that other factors contribute independently or modify the known risk factors to produce vascular disease and trigger cardiac events. Air pollution is the best-studied environmental factor known to impact hospitalizations and deaths from heart disease. Of the various air pollutants, the evidence for a causative role in cardiovascular diseases is strongest for particles derived from combustion. Indeed, the World Health Organization estimates that more than 2 million premature deaths each year are attributed to urban outdoor air pollution and indoor air pollution from the burning of solid fuels. However, the effects of air pollutants on the cardiovascular system are generally not appreciated by patients or their health care providers. The major air pollutants include particulate matter (PM), ozone (O3), nitrogen oxides, carbon monoxide (CO), and sulfur dioxide (SO2). This chapter reviews the links between air pollution and cardiovascular disease, describes plausible physiologic mechanisms accounting for these effects, and provides an educational resource for physicians and patients to decrease exposure and risk.
Particulate Matter
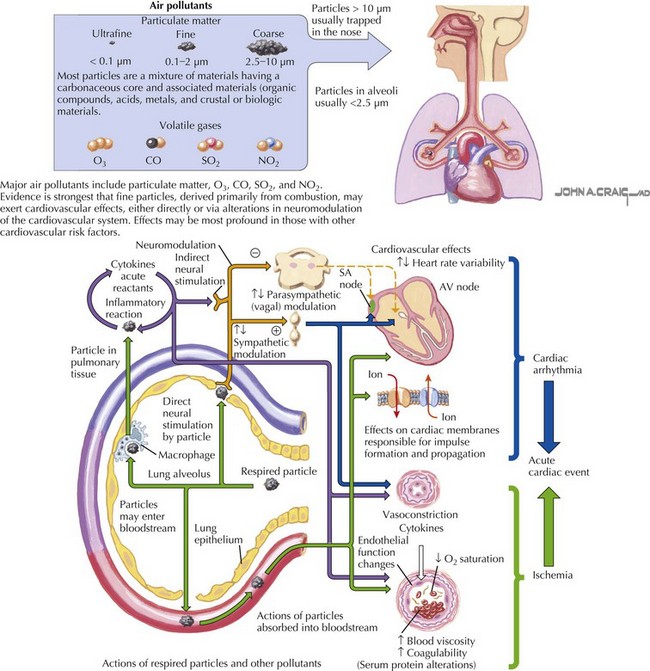
Airborne PM is not a single compound but a mixture of materials having a carbonaceous core and associated constituents such as organic compounds, acids, metals, crustal components, and biologic materials, including pollen, spores, and endotoxins. Combustion processes, such as those in vehicles and power plants, account for most human-generated PM. Importantly, particles generated by mechanical processes, windblown dust, and wildfires also contribute to the mass of PM. Particles are classified as “ultrafine,” “fine” or “coarse” based on their size. Ultrafine particles have an equivalent aerodynamic diameter smaller than 0.1 µm (about one one-thousandth the diameter of a human hair). Fine particles (PM2.5) have a diameter of 2.5 µm or less. Coarse particles (PM2.5–10) have a diameter between 2.5 and 10 µm. Only particles smaller than 10 µm in diameter are respirable (Fig. 75-1, upper). Ultrafine and fine fractions are more likely to be produced by combustion, whereas the coarse fraction is more likely to contain crustal and biologic material. Outdoor PM readily penetrates into homes and buildings depending on building stock and use of air conditioning and heating, and thus increases in outdoor PM can result in increased indoor levels of PM. Cooking, smoking, dusting, and vacuuming also contribute to indoor PM, although not much is known about cardiovascular effects induced by exposure to indoor sources of air pollution in the United States. The national air quality standard for the allowable level of PM2.5 averaged over 24 hours is 35 µg/m3, and the annual average is 15 µg/m3. The standard for PM10 averaged over 24 hours is 150 µg/m3.
The causal link between inhaled particles depositing on respiratory surfaces and cardiovascular health effects remains poorly understood. PM air pollution is associated with acute coronary syndrome (unstable angina and myocardial infarction), deep venous thrombosis, rhythm disturbances, stroke, and worsening of heart failure. Biochemical and physiologic responses of exposure to ambient air PM include changes in blood proteins, including acute-phase reactants, coagulation proteins, and proinflammatory cytokines; endothelial function; and neural modulation of the heart. Such changes would be expected to increase the risk of cardiovascular events secondary to thrombosis and arrhythmia (Fig. 75-1).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree