In the United States, approximately 15 million adults have clinically diagnosed diabetes mellitus, with 1.5 million new cases each year. Almost 35 million Americans and 35% of elderly Americans have some degree of glucose intolerance. As many as 5.7 million people may have unrecognized diabetes. At least 65% of people with diabetes mellitus die of some form of heart disease or stroke. After adjusting for population, age, and sex differences, average medical expenditures among people with diagnosed diabetes were 2.3 times higher than expenditures among those without diabetes. The direct costs related to treatment of these patients were U.S. $116 billion with an additional indirect cost of U.S. $58 billion (disability, work loss, and premature mortality).
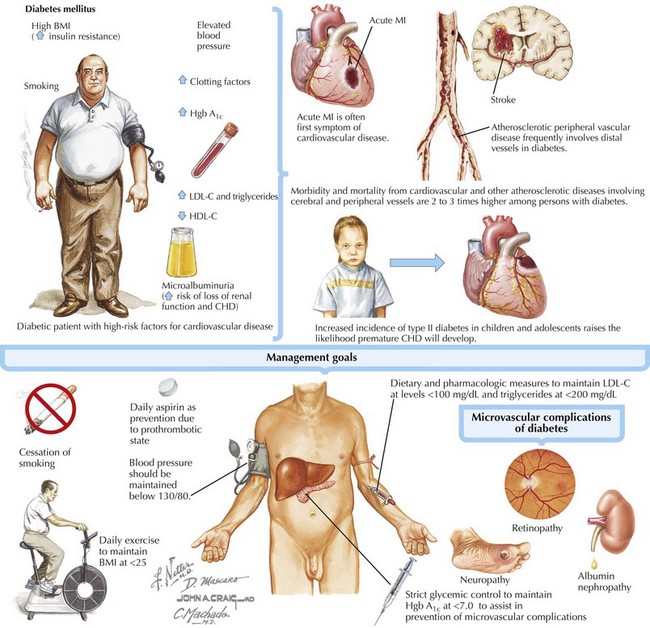
The rates of morbidity and mortality from CVD and from atherosclerotic disease involving the cerebral and peripheral vessels are two to eight times higher among individuals with diabetes (Fig. 71-1). Diabetes was the seventh leading cause of death on U.S. death certificates in 2006. Among ethnic minorities older than 18 years of age, diabetes is present in 13.6% of Native Americans, 6.5% of Asians, and 9.8% of Hispanics. The increase in type 2 diabetes among children and adolescents is likely to result in further increases in the incidence of premature coronary heart disease (CHD). The National Cholesterol Education Program Adult Treatment Panel (ATP) III identifies diabetes as a CHD equivalent and recommends the same intensive risk factor modification and preventive therapy for patients with diabetes as for patients with known CHD.
Evaluation of the patient with diabetes begins with a careful medical history (see also Chapter 1). Symptoms of atherosclerotic vascular disease, such as claudication and angina, deserve special attention, although diabetic individuals often have atypical symptoms or no symptoms at all in the presence of significant CHD. Patients with diabetes should also be evaluated for signs and symptoms of congestive heart failure. The resting ECG should be evaluated for evidence of left ventricular hypertrophy as well as new left bundle branch block, both being markers for increased cardiovascular risk. The use of medical therapies such as lipid-lowering treatment should be based on the presence of diabetes, a CHD equivalent, rather than on symptoms or the identification of an abnormality on noninvasive testing. The updated ATP III recommends a target low-density lipoprotein cholesterol (LDL-C) below 100 mg/dL, with an optional goal of less than 70 mg/dL for patients with diabetes. The American Heart Association (AHA)/American College of Cardiology (ACC) secondary prevention statement recommends that blood pressure be kept below 130/80 mm Hg and hemoglobin A1c below 7.0 as treatment goals for patients with diabetes. For patients who have triglyceride levels above 200 mg/dL despite appropriate diet and exercise and who have received statin therapy, treatment with a fibrate is recommended. Because a prothrombotic state accompanies diabetes, patients with diabetes should be considered high risk, and treatment with daily aspirin even in the absence of clinical CHD may be considered. Physical activity and maintenance of body mass index below 25 improve control of diabetes and reduce the risk of CHD-related events.
The hospitalization and long-term mortality rates following acute myocardial infarction (MI) are two to four times as high in individuals with diabetes. Diabetes is a major risk factor for adverse outcomes in patients with unstable angina. Often acute MI is the first symptom of CVD in a patient with diabetes. Because symptoms may be atypical, late recognition by the patient may delay implementation of reperfusion therapies, thus leading to a poorer prognosis. The ventricle in patients with diabetes has a higher likelihood of undergoing maladaptive remodeling, which may contribute to heart failure and cardiogenic shock. Among diabetic individuals presenting with acute MI who are undergoing primary coronary intervention, the use of a glycoprotein (GP) IIb/IIIa receptor antagonist results in better outcomes. Similar benefits have been observed with GP IIb/IIIa receptor antagonists in patients with diabetes who have unstable angina or non–ST-segment elevation MI. For patients with diabetes, the use of β-blockers results in early and late survival benefits. The admission glucose level is an independent predictor of early and late mortality in diabetic patients admitted with MI. In several studies among patients hospitalized with MI, strict glycemic control improved cardiovascular outcomes. Studies of MI survivors with diabetes show a significant survival benefit among those with optimal glycemic control for up to 3 years following their MI.
The control of cardiovascular risk factors in patients with diabetes must be a high priority. In patients with diabetes who smoke cigarettes, cardiovascular risk is doubled. The benefit of glycemic control coupled with treatment of high blood pressure and lipid abnormalities significantly reduces microvascular complications of diabetes (nephropathy, neuropathy, and retinopathy). Diabetes is the leading cause of end-stage renal disease in the United States (accounting for 44% of the new cases of renal failure in 2005), with a 5-year survival of only 20%. Microalbuminuria is a major predictor of impaired renal function as well as for the development of CHD. The early use of angiotensin-converting enzyme inhibitors among patients with diabetes, even in the absence of hypertension, reduces the rates of cardiovascular morbidity and mortality.
Of the nearly 1.5 million percutaneous and surgical revascularization procedures carried out annually in the United States, roughly 25% are performed on patients with diabetes. In this group, comorbidities such as hypertension, dyslipidemia, systolic and diastolic heart failure, nephropathy, and peripheral vascular, cerebrovascular, and microvascular diseases contribute to poorer outcomes as compared with patients without diabetes. In addition to the extent of coronary artery disease (CAD), the presence of diabetes alone may govern the revascularization approach chosen. For instance, significant differences in survival, favoring surgical revascularization, exist for patients with diabetes and two- or three-vessel CAD who are randomized to coronary artery bypass graft surgery compared with percutaneous coronary intervention. The benefits of coronary artery bypass graft surgery are seen only when at least one arterial conduit is used. The increased use of stents and GP IIb/IIIa receptor antagonists in percutaneous revascularization procedures has improved outcomes from percutaneous revascularization. Further studies that will help define the relative benefits of coronary artery stenting using drug-eluting stents versus surgical revascularization among patients with diabetes are continuing.