After reading this chapter, you will be able to: 1. Describe the causes and common characteristics of the following symptoms: Symptoms are subjective clinical findings generally reported by the patient during or shortly after the initial interview (described in Chapter 2). Clinical signs, on the other hand, are objective and measurable, such as the vital signs and laboratory studies detailed in subsequent chapters of this text. Respiratory therapists (RTs) will encounter patients with a variety of symptoms. The primary symptoms associated with cardiopulmonary disorders are cough, sputum production, hemoptysis, shortness of breath (dyspnea), and chest pain. Other less specific complaints include dizziness and fainting; ankle swelling (peripheral edema); fever, chills, and night sweats; snoring; personality changes; daytime somnolence (sleepiness); and gastric reflux. This chapter defines the terms associated with these symptoms, briefly discusses their causes (etiology), and describes how these symptoms relate to commonly associated diseases. The more familiar RTs are with these symptoms and their characteristics, the better they can ask relevant questions, assist the patient care team in making a correct diagnosis, and help design an appropriate interdisciplinary treatment plan. Cough is one of the most common, though nonspecific, symptoms seen in patients with pulmonary disease. It is the powerful protective reflex arising from stimulation of receptors located in the pharynx, larynx, trachea, large bronchi, and even the lung and the visceral pleura. Coughing can be caused by inflammatory, mechanical, chemical, or thermal stimulation of cough receptors found anywhere from the oropharynx to the terminal bronchioles or simply by tactile pressure in the ear canal. There are many conditions that can make a patient cough. The key to determining the cause in many cases can be found in a careful review of the history, physical examination, and chest radiograph (Table 3-1). TABLE 3-1 Possible Causes of Cough Receptor Stimulation 1. Inspiratory phase: reflex opening of the glottis and contraction of the diaphragm, thoracic, and abdominal muscles cause a deep inspiration with a concomitant increase in lung volume accompanied by an increase in the caliber and length of the bronchi. 2. Compression phase: closure of the glottis and relaxation of the diaphragm while the expiratory muscles contract against the closed glottis can generate very high intrathoracic pressures and narrowing of the trachea and bronchi. 3. Expiratory phase: opening of the glottis, explosive release of trapped intrathoracic air, and vibration of the vocal cords and mucosal lining of the posterior laryngeal wall shake secretions loose from the larynx and move undesired material out of the respiratory tract. 1. Weakness of either the inspiratory or expiratory muscles 2. Inability of the glottis to open or close correctly 3. Obstruction, collapsibility, or alteration in shape or contours of the airways 4. Decrease in lung recoil as occurs with emphysema 5. Abnormal quantity or quality of mucus production (e.g., thick sputum) Most patients will have a single cause for their cough; however, in some patients, two or three simultaneous causes (comorbidities) may be present. Cough may be acute (sudden onset, usually severe with a short course, self-limited), chronic (persistent and troublesome for more than 3 weeks), or paroxysmal (periodic, prolonged, and forceful episodes). An acute self-limited cough is usually due to a viral infection involving the upper airway, which usually resolves in a few days. A chronic persistent cough is most commonly caused by postnasal drip syndrome, followed by acute asthma, acute exacerbation of chronic obstructive pulmonary disease (COPD), allergic rhinitis, gastroesophageal reflux disease (GERD), chronic bronchitis, bronchiectasis, and other conditions such as left heart failure, bronchogenic cancer, and sarcoidosis. In smokers, chronic cough is usually due to chronic bronchitis (“smoker’s cough”). Still other chronic coughs may result from certain medications, such as angiotensin-converting enzyme (ACE) inhibitors commonly prescribed for congestive heart failure and other cardiac conditions. Though not fully understood, patients taking ACE inhibitors may develop a chronic dry cough, possibly as a result of an increase in cough mediators that accumulate in the upper airway. Hence, the medication history described in Chapter 2 can provide vital clues to the underlying cause. Aggravating, painful, or persistent cough or cough equivalent, such as throat clearing, is not normal and warrants further clinical investigation. The quality, time, and setting in which a cough occurs may also provide some clues to the location and type of disorder (Table 3-2). Barking (like a seal), brassy (harsh, dry), and hoarse coughs, as well as those associated with inspiratory stridor, are usually heard when there is a problem with the larynx (e.g., infection or tumor). Wheezy coughs (accompanied by whistling or sighing sounds) suggest bronchial disorders. Acute, productive coughs are most often seen with allergic asthma as well as bacterial or viral respiratory infections, and chronic productive coughs are generally indicative of significant bronchopulmonary disease (e.g., chronic bronchitis). Hacking (frequent brief periods of coughing or clearing the throat) may be dry and the result of smoking, a viral infection, a nervous habit, or difficult-to-move secretions, which may occur with postnasal drip. TABLE 3-2 ACE, angiotensin-converting enzyme; AIDS, acquired immunodeficiency syndrome; COPD, chronic obstructive pulmonary disease; TB, tuberculosis; URI, upper respiratory infection (common cold). Sputum should be described as to the color, consistency, odor, quantity, time of day, and presence of blood or other distinguishing matter. The amount may vary from scanty (a few teaspoons) to copious (as much as a pint or more), as seen in certain chronic bronchial infections and bronchiectasis. These characteristics of the sputum may be highly indicative of the underlying disorder (Table 3-3). Though sputum culture and sensitivity tests described in Chapter 7 provide for a more in depth microbiologic examination of sputum, bedside examination can be helpful as an initial screening tool. TABLE 3-3 Differential diagnosis is complex and includes bronchopulmonary, cardiovascular, hematologic, and other systemic disorders (Box 3-1). A history of pulmonary or cardiovascular disease; cigarette smoking and tobacco use; trauma; aspiration of a foreign body; repeated and severe lung infections; bleeding disorder; use of anticoagulant agents (warfarin or heparin), aspirin, nonsteroidal anti-inflammatory agents, or chemotherapeutic agents; or inhaling crack cocaine suggests the possible cause of hemoptysis. A history of travel to places where tuberculosis or fungal infections, such as coccidioidomycosis or histoplasmosis, are prevalent, including central Africa (tuberculosis) and the San Joaquin Valley of California (coccidioidomycosis), may also help identify the underlying disorder. “Spitting up blood,” as patients frequently call it, may be confused with blood originating in the oropharynx, esophagus, or stomach. The patient with a nosebleed at night could cough up blood in the morning. The presence of symptoms, such as nausea and vomiting, especially with a history of alcoholism or cirrhosis of the liver, may suggest the esophagus or stomach as the source. Conversely, vomiting of blood may sometimes manifest from bronchopulmonary bleeding. When bleeding occurs during the night and the blood reaches the oropharynx, it may be swallowed without the patient waking. The swallowed blood may act as an irritant, and the patient may vomit early in the morning. Careful questioning and often examination of the bloody sputum are required to distinguish hemoptysis from hematemesis (vomited blood) (Table 3-4). It is important to obtain a detailed sequence of events to determine whether the blood originated in the respiratory tract and was swallowed and then vomited, or the blood was vomited, aspirated, and later expectorated. TABLE 3-4 Distinguishing Characteristics of Hemoptysis and Hematemesis 1. Sensory input to the cerebral cortex. Multiple sources of sensory information from mechanoreceptors in the upper airway, thorax, and muscles are integrated in the central nervous system and sent to the sensorimotor cortex in the brain. In general, the sensation of dyspnea is related to the intensity of the input from the thoracic structures and from chemoreceptors. It varies directly with ventilatory demand such as exercise and inversely with ventilatory capacity (ability to move gas in and out of the lung). The more stimulation of the drive to breathe when ventilatory abnormalities exist, the greater the dyspnea. 2. Perception of the sensation. Perception relies on interpretation of the information arriving at the sensorimotor cortex, and interpretation is highly dependent on the psychological makeup of the person. The emotional state, distraction, and belief of significance can influence the perception of dyspnea. A Modified Borg Scale, such as shown in Table 3-5, also uses a 0 to 10 scoring system with descriptive terms to depict the perceived intensity of a symptom such as dyspnea after a specified task. Tools like the frequently used American Thoracic Society Shortness of Breath Scale (Table 3-6) specify the degree of dyspnea (slight, moderate, severe, or very severe) using descriptive terms as well as a numerical grading system. In addition, there are also questionnaires that attempt to quantify the severity of dyspnea by asking patients to rate their shortness of breath while performing a variety of activities of daily living. TABLE 3-5 Modified Borg Scale for Estimation of Subjective Symptoms TABLE 3-6 American Thoracic Society Shortness of Breath Scale (From Muza SR, Silverman MY, Gilmore GC et al: Comparison of scales used to quantitate the sense of effort to breath in patients with chronic obstructive pulmonary disease, Am Rev Respir Dis 141:909, 1990.) Dyspnea is most often related to pulmonary or cardiac disease, but it is also seen with hematologic, metabolic, chemical, neurologic, psychogenic, and mechanical disorders. Dyspnea may be described by clinical type as shown in Table 3-7, or the causes of dyspnea may be grouped by body system as listed in Table 3-8. TABLE 3-7
Cardiopulmonary Symptoms
 Fever, chills, and night sweats
Fever, chills, and night sweats
 Headache, altered mental status, and personality changes
Headache, altered mental status, and personality changes
Cough
Types of Stimulation
Possible Causes
Inflammatory
Infection, lung abscess, drug reaction, allergy, edema, hyperemia, collagen vascular disease, radiotherapy, pneumoconiosis, tuberculosis
Mechanical
Inhaled dusts, suction catheter, food
Obstructive
Foreign bodies, aspirations of nasal secretions, tumor or granulomas within or around the lung, aortic aneurysm
Airway wall tension
Pulmonary edema, atelectasis, fibrosis, chronic interstitial pneumonitis
Chemical
Inhaled irritant gases, fumes, smoke
Temperature
Inhaled hot or cold air
Ear
Tactile pressure in the ear canal (Arnold nerve response) or from otitis media
Causes and Clinical Presentation
Descriptions
Description
Possible Causes
Acute (<3 wk) or recurrent (adults) productive
Postnasal drip, allergies, infections, especially viral URI, bronchitis
Acute or recurrent (adults) and nonproductive
Laryngitis, inhalation of irritant gases
Chronic productive
Bronchiectasis, chronic bronchitis, lung abscess, asthma, fungal infections, bacterial pneumonias, tuberculosis
Chronic (>3 wk) or recurrent (adults) and nonproductive
Postnasal drip, asthma, gastroesophageal reflux, bronchiectasis, COPD, lung tumor, sarcoidosis, ACE inhibitors, left heart failure
Recurrent (children)
Viral bronchitis, asthma, allergies
Dry
Viral infections, inhalation of irritant gases, interstitial lung diseases, pleural effusion, cardiac condition, nervous habit, tumor, radiation therapy, chemotherapy
Dry, progressing to productive
Atypical and mycoplasmal pneumonia, AIDS, legionnaires disease, asthma, silicosis, pulmonary embolus and edema, lung abscess, emphysema (late in disease), smoking
Inadequate, weak
Debility, weakness, oversedation, pain, poor motivation, emphysema
Paroxysmal (especially night)
Aspiration, asthma, left heart failure
Barking
Epiglottal disease, croup, influenza, laryngotracheal bronchitis
Brassy or hoarse
Laryngitis, laryngotracheal bronchitis, laryngeal paralysis, pressure on recurrent laryngeal nerve: mediastinal tumor, aortic aneurysm, left atrial enlargement
Inspiratory stridor
Tracheal or mainstem bronchial obstruction, croup, epiglottitis
Wheezy
Bronchospasm, asthma, bronchitis, cystic fibrosis
Morning
Chronic bronchitis, smoking
Associated with position change or lying down
Bronchiectasis, left heart failure, chronic postnasal drip or sinusitis, gastroesophageal reflux with aspiration
Associated with eating or drinking
Neuromuscular disease of the upper airway, esophageal problems, aspiration
Sputum Production
Causes and Descriptions
Appearance of Sputum
Possible Cause
Clear, colorless, like egg white
Normal
Black
Smoke or coal dust inhalation
Brownish
Cigarette smoker
Frothy white or pink
Pulmonary edema
Sand or small stone
Aspiration of foreign material, broncholithiasis
Purulent (contains pus)
Infection, pneumonia caused by:
Apple-green, thick
Haemophilus influenzae
Pink, thin, blood-streaked
Streptococci or staphylococci
Red currant jelly
Klebsiella species
Rusty
Pneumococci
Yellow or green, copious
Pseudomonas species pneumonia, advanced chronic bronchitis, bronchiectasis (separates into layers)
Foul odor (fetid)
Lung abscess, aspiration, anaerobic infections, bronchiectasis
Mucoid (white-gray and thick)
Emphysema, pulmonary tuberculosis, early chronic bronchitis, neoplasms, asthma
Grayish
Legionnaires disease
Silicone-like casts
Bronchial asthma
Mucopurulent
As above with infection, pneumonia, cystic fibrosis
Blood-streaked or hemoptysis (frankly bloody)
Bronchogenic carcinoma, tuberculosis, chronic bronchitis, coagulopathy, pulmonary contusion or abscess (see discussion of causes of hemoptysis)
Hemoptysis
Definition
Causes
Hemoptysis versus Hematemesis
Characteristic
Hemoptysis
Hematemesis
History
Cardiopulmonary disease
Gastrointestinal disease
As stated by the patient
Coughed up from lungs/chest
Vomited from stomach
Associated symptoms
Dyspnea, pain or tickling sensation in chest
Nausea, pain referred to stomach
Blood: pH
Alkaline
Acid
Mixed with
Sputum
Food
Froth
May be present
Absent
Color
Bright red
Dark, clotted, “coffee grounds”
Shortness of Breath (Dyspnea)
Subjectiveness of Dyspnea
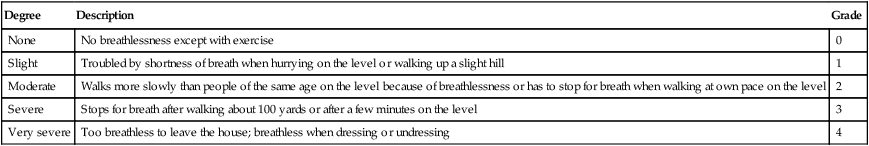
Dyspnea Scoring Systems
Rating
Intensity of Sensation
0
Nothing at all
0.5
Very, very mild/weak
1
Very mild/weak
2
Mild/weak
3
Moderate
4
Somewhat severe/strong
5
6
7
Very severe/strong
8
9
Very, very severe/strong
10
MAXIMAL
Degree
Description
Grade
None
No breathlessness except with exercise
0
Slight
Troubled by shortness of breath when hurrying on the level or walking up a slight hill
1
Moderate
Walks more slowly than people of the same age on the level because of breathlessness or has to stop for breath when walking at own pace on the level
2
Severe
Stops for breath after walking about 100 yards or after a few minutes on the level
3
Very severe
Too breathless to leave the house; breathless when dressing or undressing
4
Causes, Types, and Clinical Presentation of Dyspnea
Dyspnea
Associated with
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access










