26 Cardiomyopathy
I. CASE
A. Fetal echocardiography findings
a. Fetal echocardiography reveals situs solitus of the atria, levocardia, left aortic arch, and heart rate of 150 bpm.
b. The four-chamber view is abnormal with equal-sized ventricles, both being hypertrophic and dilated, and a normal cardiac axis and position. Cardiac size is increased (cardiothoracic ratio = 0.6).
c. There is no evidence of structural congenital heart disease. Specifically, the aortic valve is normal, with no evidence of valvar or subvalvar stenosis.
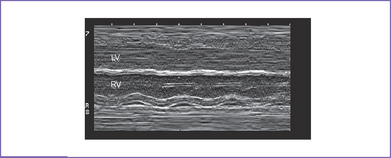
d. There is severely reduced shortening of the ventricles, with left worse than right (Fig. 26-1).
e. The aortic and ductal arches are normal. The aortic arch is leftward and the ductal and aortic arches are of similar size.
f. The aortic annulus is of normal size, and there is normal Doppler velocity through it at 0.6 m/s.
g. Pulmonary outflow is normal, suggesting no evidence of increased cardiac output.
h. Inflow velocity at the atrioventricular (AV) valves is abnormal, with nearly absent E wave suggesting diastolic dysfunction.
i. The pulmonary venous flow pattern is normal.
j. A small pericardial effusion is present, and there are no other hydropic signs.
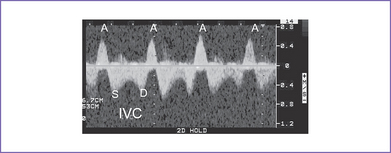
k. There is increased A wave reversal in the inferior vena cava (IVC) and hepatic veins and a wave reversal in the ductus venosus.
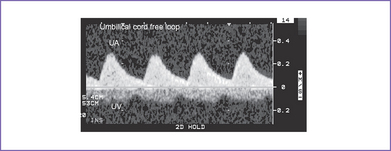
l. The umbilical artery Doppler is normal, but there are umbilical venous pulsations in the free loop of the umbilical cord (Fig. 26-2).
D. Fetal management and counseling
1. Amniocentesis was offered but declined.
a. Evaluation for fetal infection is performed including viral titers for Coxsackievirus, adenovirus, TORCH (toxoplasmosis, other infections, rubella, cytomegalovirus, herpes simplex virus) infections, and parvovirus screen.
b. The mother is assessed for anti-Ro and anti-La autoantibodies.
c. Every week she is evaluated for:
a. Digoxin 0.2 mg PO twice per day was started, and the mother tolerated it without complication (e.g., nausea, ECG changes, or arrhythmia).
b. The mother’s trough level, checked 1 week later, was 1.2 ng/mL.
E. Delivery
a. Delivery near term is most desired.
b. Prenatal listing for cardiac transplantation beyond 34 to 35 weeks may be feasible in some centers, particularly if this is the most likely course for the infant after birth. It would require a commitment for delivery if a heart became available before spontaneous delivery. Depending upon the transplant center strategy, transplantation can require knowledge of both fetal and maternal blood type at the time of listing.
F. Neonatal management
a. The severity of the infant’s heart failure and hemodynamic instability determines the intensity and level of resuscitation.
b. Assessment for a potentially treatable cause of myocardial disease is important.
a. Cardiac transplantation is the only true option for the majority of severely affected neonates and infants.
b. Early consideration for transplantation, even before birth in some centers, is important because the baby can die before a donor heart becomes available.
G. Follow-up
1. Transplantation in the neonate has a small risk at the time of the operation, but heart failure and death can occur while the patient is on the waiting list.
2. Rejection of the transplanted heart can occur, medications can cause malignancy, and side effects of the rejection medications can cause morbidity or mortality.
3. The child’s growth can be altered if steroids are required to prevent rejection.
4. Immune suppression makes the child more susceptible to infections.
5. The parents must pass an evaluation of their psychological profile to assess their coping skills to care for a child with a heart transplant.
6. Average outcomes are center-dependent but average 75% survival at 5 years.
I. Outcome of this case
1. The baby was born at 37 weeks weighing 3.5 kg (appropriate for gestation) with Apgar scores of 7 at 1 minute and 8 at 5 minutes.
2. Venous and arterial lines were placed and the baby was taken immediately to the neonatal intensive care unit (ICU).
4. On admission, the neonate was active and had no obvious malformation and vital signs were normal.
5. There was decreased perfusion in the extremities.
6. Milrinone IV infusion, 0.5 μg/kg per minute, was used to improve the distal perfusion.
7. Blood gas analysis showed mild metabolic acidosis that was corrected.
8. Lactate assay was monitored daily.
9. The echocardiogram confirmed the diagnosis of biventricular dilated or hypertrophied cardiomyopathy with fractional shortening of the LV of 10%.
10. LV ejection fraction was 12%.
11. There was severe hypertrophy of both ventricles.
12. RV function was also severely decreased.
13. Cardiac transplant was performed at 6 weeks of age without complication.
14. Discharge medications included digoxin, furosemide, cyclosporine, and steroids.
15. He is thriving 5 years later under the care of the cardiac transplant team on no cardiac medications.
16. Examination of the explanted heart showed findings compatible with a mitochondrial myopathy without evidence of skeletal muscle involvement.