Cardiomyopathies
Christopher L. Holley
High-Yield Findings
HCM is characterized by LV hypertrophy in the absence of pressure overload; 35% of cases do not have any outflow obstruction
Hypertrophic obstructive cardiomyopathy (HOCM) is a variant of HCM with outflow obstruction >30 mmHg; often with asymmetric septal hypertrophy (ASH), systolic anterior motion (SAM), and eccentric MR
DCM is accompanied by both increased LV mass and volume; EF <55%; diastolic dysfunction is always present and central (functional) MR is common
RCM involves restrictive filling without hypertrophy or dilation; it should prompt a thorough search for an underlying etiology, such as amyloid or other systemic illnesses
Arrhythmogenic right ventricular dysplasia (ARVD) echocardiographic findings include RVOT diameter >30 mm and RV dysfunction in the presence of a normal LV. RV trabecular derangement is common
Takotsubo cardiomyopathy is transient LV dysfunction with apical hypokinesis and basal hyperkinesis; requires angiography to exclude significant CAD
Non-compaction is a developmental disorder with echocardiographic findings of abnormal LV trabeculation and cardiomyopathy
Key Views
HCM: PLAX to show abnormal septal or inferolateral wall thickness
HOCM: PLAX (2D and M-mode) to look for ASH and SAM; A4C Doppler to demonstrate and localize LVOT gradient
DCM: PLAX and A4C to show increased LV cavity diameter and volume; A4C Doppler to demonstrate diastolic dysfunction and look for MR
RCM: A4C to assess restrictive filling by transmitral PW Doppler and low mitral annular tissue Doppler velocities
ARVD: PLAX or PSAX to demonstrate RVOT enlargement; off-axis A4C to evaluate RV function and search for structural abnormalities
Takotsubo: PLAX and A4C to show apical ballooning and hypercontractile basal segments
Non-compaction: Apical and PSAX views with contrast enhancement to demonstrate abnormal LV trabeculation
The European Society of Cardiology uses this definition for cardiomyopathy: “A myocardial disorder in which the heart muscle is structurally and functionally abnormal, in the absence of coronary artery disease, hypertension, valvular disease, and congenital heart disease sufficient to cause the observed myocardial abnormality.” (Elliott, P, et al. Classification of the cardiomyopathies: a position statement from the European Society Of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J. 2008;29:270–276.) The five broad categories of cardiomyopathy are:
Hypertrophic cardiomyopathy (HCM, including obstructive forms)
Dilated cardiomyopathy (DCM)
Arrhythmogenic right ventricular dysplasia (ARVD)
Restrictive cardiomyopathy (RCM—see also Chapter 19)
Other (including takotsubo and non-compaction cardiomyopathy)
Hypertrophic Cardiomyopathy (HCM)
HCM is defined by the presence of increased ventricular wall thickness or mass in the absence of pressure overload. Such conditions that would otherwise lead to hypertrophy, such as hypertension and valvular heart disease (especially AS), must be excluded.
Background
Around 1:500 adults in the general population, men = women
Important cause of sudden cardiac deaths in young adults
Majority of patients do not have an outflow obstruction at rest
35% of patients are not obstructed at rest or with provocation
Echocardiographic Findings
Left ventricular (LV) hypertrophy (increased mass), concentric or eccentric
Septal or inferolateral wall thickness >1.5 cm (PLAX or PSAX)
No LV dilatation
HOCM: HCM with obstructive physiology
LVOT obstruction is dynamic, that is, increases with time during systole
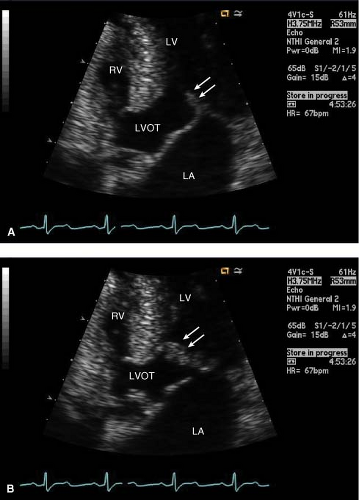
ASH of the basal ventricular septum (see Fig. 8-1A)
SAM of the anterior mitral leaflet toward the septum
SAM:
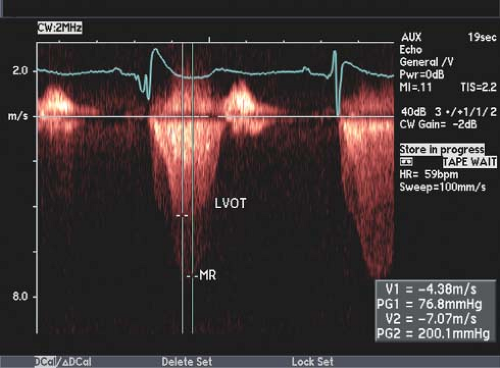
Eccentric posteriorly directed, MR jet secondary to SAM causing incomplete leaflet apposition (Fig. 8-3B)
As MR is mid to late peaking, it may be confused with the LVOT gradient.
A central or anterior jet should raise concern for intrinsic mitral valve pathology.
The MR jet peak velocity and systolic blood pressure (SBP) can be used to verify what the expected LVOT gradient should be and can be used as a “reality
check.” In Figure 8-4, CW Doppler shows both the broader MR jet superimposed on the LVOT jet with measured gradients fitting with measured SBP.
MR peak gradient = LVSP – LAP
 LVSP = MR peak gradient + LAP
LVSP = MR peak gradient + LAP
SBP = LVSP – LVOT gradient
 LVOT gradient = LVSP – SBP
LVOT gradient = LVSP – SBP
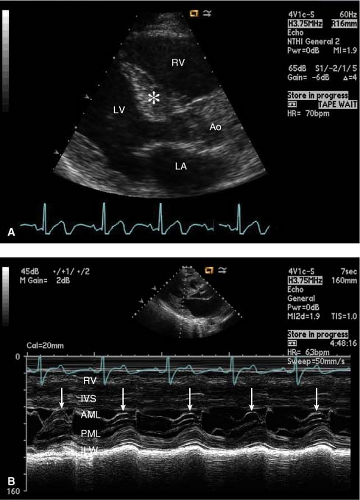
Figure 8-1. (A) Typical PLAX view for HOCM, with eccentric hypertrophy of the basal septum (*). (B) M-mode from the same view, demonstrates SAM of the MV anterior leaflet in systole (arrows).
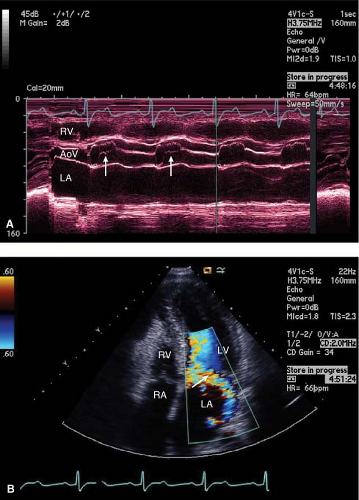
Figure 8-3. (A) Mid-systolic closure of the AoV due to dynamic LVOT obstruction (arrows). (B) Mid-systolic MR (arrow) with posteriorly directed jet due to SAM of the MV.
Subaortic gradient: ≥30 mmHg (velocity ≥2.7 m/s)
CW Doppler will show late-peaking Doppler envelope (“broad-blade dagger” shape) due to dynamic nature of obstruction (Fig. 8-5A). Intracavitary LV gradients due to hyperdynamic LV function and small LV cavity are distinguished from LVOT gradients by having a “narrow-blade” and “pointy” late-peaking gradient (Fig. 8-5B). These both are in contrast to the early to mid-peaking Doppler envelope of fixed outflow obstruction (e.g., valvular AS, subaortic membrane) (Fig. 8-5C).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree