Chapter 5 Cardiac Testing
Patients presenting for heart surgery have usually undergone a number of cardiac investigations preoperatively. In this chapter, the indications, principles, and interpretations of common preoperative cardiac investigations are discussed. Chest radiography and echocardiography are discussed in Chapters 6 and Chapter 7, respectively.
ANGIOGRAPHY OF THE CORONARY ARTERIES AND LEFT VENTRICLE
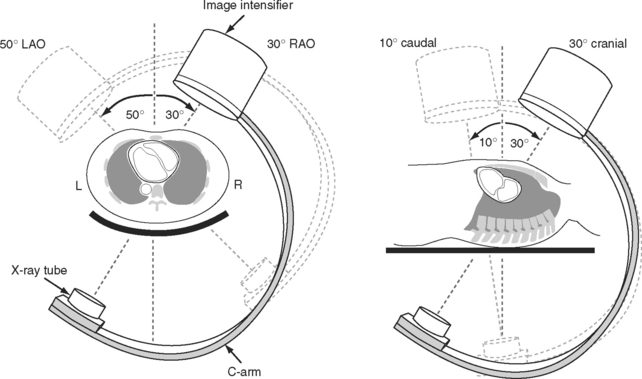
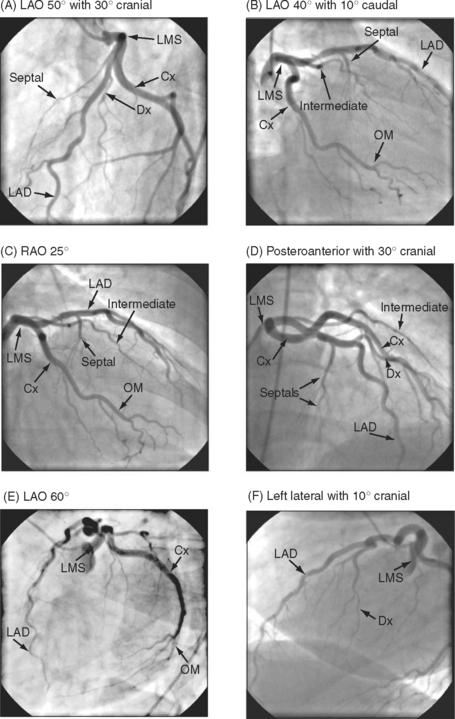
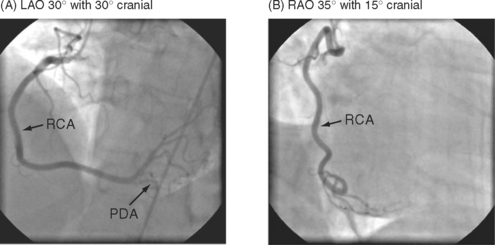
The complex and overlapping nature of the coronary anatomy necessitates image acquisition from a variety of angles to ensure complete visualization. The relationship between the patient, the x-ray tube, and the image intensifier during coronary angiography is shown in Figure 5-1. Images of normal coronary arteries obtained from some of the standard angiographic projections are shown in Figures 5-2 and 5-3.
Coronary Anatomy
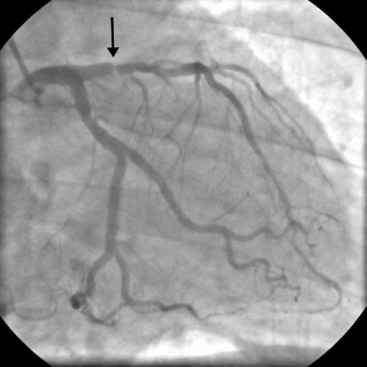
The anatomy of the coronary circulation varies among individuals but most patients have similar distributions of the major epicardial vessels. The left main-stem coronary artery arises from the left coronary sinus and divides after a short distance into the left anterior descending (LAD) and the left circumflex coronary arteries. Occasionally, the circumflex coronary artery arises directly from the right coronary sinus, adjacent to the right coronary artery (RCA). The LAD coronary artery (see Fig. 5-2) runs along the surface of the interventricular septum, passing anteriorly, inferiorly, and to the left in the anterior interventricular groove. It usually terminates a short distance beyond the apex, having turned onto the inferior surface of the heart in the posterior interventricular groove. The LAD coronary artery gives rise to septal branches that pass into the substance of the anterior interventricular septum, supplying the majority of this structure. The LAD coronary artery also gives rise to branches to the anterior (or diagonal) surface of the left ventricle, known as diagonal branches (see Fig. 5-2A, 5-2F). The number, size, and point of origin from the LAD coronary artery of the septal and diagonal branches are highly variable.
The circumflex coronary artery passes to the left and inferiorly in the left atrioventricular groove, usually terminating close to the junction of the lateral and the inferior surfaces of the left ventricle. The circumflex artery gives rise to a series of branches to the lateral surface of the left ventricle known as obtuse marginal (OM) branches (see Fig. 5-2 B, 5-2C, 5-2E). The number, size, and point of origin of the OM vessels vary greatly. A large branch, known as the intermediate coronary artery (see Fig. 5-2 B, 5-2C, 5-2D), may arise directly from the left main bifurcation or from the very proximal course of either the LAD or circumflex arteries to supply a portion of the diagonal (anterior) and OM (lateral) surfaces of the heart. Intermediate arteries can supply a substantial amount of the left ventricle and may be much larger than the circumflex artery.
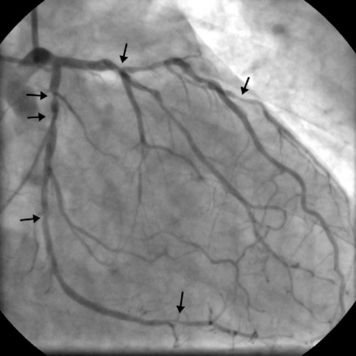
The RCA (see Fig. 5-3) arises from the right coronary sinus and passes inferiorly and to the right in the right atrioventricular groove before passing around the acute margin onto the inferior surface of the heart to reach the crux, the point at which the atrioventricular and interventricular grooves meet. The major branch to the posterior septum is the posterior descending coronary artery (PDA) (Fig. 5-3 A). The PDA normally arises from the RCA proximal to or at the crux, and passes anteriorly in the posterior interventricular groove, giving off a number of septal branches that enter the posterior portion of the interventricular septum. In some individuals, the RCA is so small it supplies none of the left ventricle, and the PDA arises from the circumflex coronary artery. The origin of the PDA determines the dominance of the coronary circulation. In more than 90% of the population the PDA arises from the RCA (right dominance); in about 6% of the population the PDA arises from the circumflex coronary artery (left dominance); and in less than 2% of individuals the supply to the posterior septum is shared (indeterminate dominance). Distal to the crux, the RCA continues along the posterior atrioventricular groove and gives rise to a number of branches which pass anteriorly on to the inferior surface of the left ventricle. The supply to the sinoatrial node arises from the proximal RCA. The supply to the atrioventricular node is a small artery that arises in the region of the crux, usually from the RCA.
Coronary Stenoses
Stenoses due to chronic atherosclerotic disease cause angina and exercise-induced myocardial ischemia. In contrast, unstable angina or acute coronary syndromes are usually associated with thrombus formation on a ruptured plaque, which prior to thrombus formation may have been causing only minor narrowing. Patients with acute coronary syndrome should have urgent coronary angiography with a view to revascularization. However, if a thrombolytic drug such as streptokinase has been administered, the thrombus may have resolved by the time of angiography.
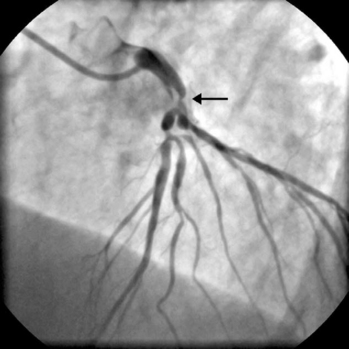
The presence of significant stenosis (>50%) of the left main stem coronary artery (Fig. 5-4) or of severe disease in the proximal course of both LAD and circumflex coronary arteries (left main equivalent disease) represents a situation of special concern because of the large proportion of the left ventricular myocardium whose vascular supply is in jeopardy. This is particularly the case in patients with left-dominant circulations. Urgent revascularization is indicated. Patients with severe stenoses of the proximal LAD coronary artery (Fig. 5-5) or extensive coronary artery disease (Fig. 5-6) also have a survival benefit from revascularization (Chapter 9).
Left Ventriculography and Pressure Recordings
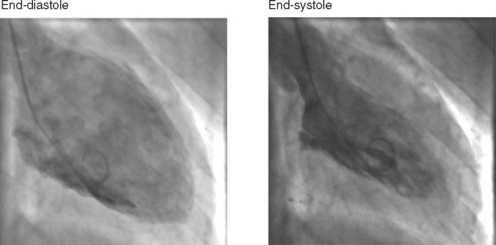
A left ventriculogram (Fig. 5-7) is commonly performed at the time of coronary angiography. Left ventriculography allows measurement of ventricular volumes and ejection fraction (Table 5-1) and provides some assessment of regional wall motion. The degree of mitral regurgitation, if any, may also be assessed. Care should be taken in the interpretation of measurements made of postectopic beats, as the measured ejection fraction will be greater than that obtained from a normal sinus beat (due to increased end-diastolic and reduced end-systolic volumes). The left ventriculogram is often omitted in patients with diabetes or left main-stem disease in order to reduce the dose of radiographic contrast medium. Radiographic contrast medium is nephrotoxic, especially in diabetics, and also has vasodilator and myocardial depressant effects, which may critically reduce myocardial perfusion in patients with left main-stem disease.
Table 5-1 Normal Values for Left Ventricular Volumes and Ejection Fraction
| End-diastolic volume index | < 90 ml/m2 |
| End-systolic volume index | < 30 ml/m2 |
| Ejection fraction | 55% to 75% |
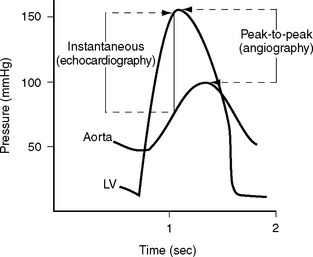
A pressure recording is made across the aortic valve as the catheter is withdrawn after the left ventricular study to check for aortic valve stenosis. Comparison of angiographic and echocardiographic transvalvular pressure gradients may reveal surprising discrepancies for a variety of reasons. Aortic valve gradients obtained from echocardiography are instantaneous measurements, whereas those from a cardiac catheter study are peak-to-peak pressure measurements (Fig. 5-8). Underestimation of transvalvular gradients in echocardiography may occur if imaging windows are poor or if the Doppler signal has not been lined up accurately with the jet of stenotic flow. Cardiac output may appear to be different on the angiogram and the echocardiogram. Cardiac catheterization is typically performed under mild benzodiazepine sedation, which may result in reduced gradients.
RIGHT HEART CATHETERIZATION
Right heart catheterization is performed for the evaluation of right ventricular function, pulmonary vascular disease, and intracardiac shunting. Common clinical scenarios in which right heart catheterization is indicated include the assessment of pulmonary vascular resistance prior to heart transplantation (Chapter 14), in patients with suspected Eisenmenger syndrome (Chapter 15), and in the diagnosis of idiopathic (or primary) pulmonary hypertension. Patients with pulmonary hypertension secondary to valvular heart disease are usually assessed with echocardiography but may occasionally undergo right heart catheterization.
The procedure may be performed using a standard balloon-tipped flow-directed pulmonary artery catheter (Chapter 8) or a catheter without a balloon (e.g., a Cournand catheter). It is often carried out in conjunction with left heart catheterization. Measurements that may be made during a right heart catheter study include right atrial pressure, pulmonary arterial pressure, pulmonary artery wedge pressure, cardiac output, and oxygen saturations from the vena cavae, right atrium, and pulmonary artery. In most catheter laboratories, cardiac output is routinely measured by using the thermodilution technique (Chapter 8). If thermodilution is likely to be inaccurate (e.g., due to the presence of severe tricuspid regurgitation) the Fick method may be used (see Equation 1-15). The Fick method necessitates obtaining pulmonary arterial and systemic arterial oxygen saturations and measuring oxygen consumption. From the measured variables (cardiac output, pulmonary artery wedge pressure, mean pulmonary artery pressure), transpulmonary gradient (Chapter 24) and pulmonary vascular resistance are calculated (see Equation 1-6).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree