Cardiac Testing
4.1 Exercise Stress Testing
Circ 2002;106:1883; J Am Coll Cardiol 2002;40:1531
Indications
Pts with intermediate pretest probability of CAD with normal EKG, RBBB, <1 mm resting ST depression but not pre-excitation (Wolff-Parkinson-White) syndrome, paced ventricular rhythm or complete LBBB
Pts with suspected vasospastic angina
Risk assessment inpts with CAD undergoing initial evaluation or who have significant change in clinical status
Pts post-MI: submaximal at 4-7 d, symptom-limited at 14-21 d or at 3-6 wk if early exercise test was submaximal
Pts with multiple risk factors or who are at high risk for CAD due to other diseases; men > 40 yr and women > 50 yr who plan to start vigorous exercise, who are in occupations in which impairment might affect public safety, or who are at high risk for CAD due to other diseases
Evaluation of asymptomatic adultpts with diabetes mellitus who have additional CAD risk factors or microvascular disease
Pts with chronic aortic regurgitation who require evaluation of functional capacity
Pts with recurrent sx suggesting ischemia after revascularization
Evaluation of exercise-induced arrhythmias and of ablative therapy in suchpts
Evaluation of patients with congenital complete heart block
Identification of appropriate settings inpts with rate-adaptive pacemakers
Contraindications
Absolute Contraindications
High-risk, unstable angina
Uncontrolled cardiac arrhythmias causing symptoms or hemodynamic compromise
Symptomatic severe aortic stenosis
Uncontrolled symptomatic CHF
Acute pulmonary embolus or pulmonary infarction
Acute myocarditis or pericarditis
Acute aortic dissection
Relative Contraindications
Left main coronary stenosis
Moderate stenotic valvular heart disease
Electrolyte abnormalities
Tachyarrhythmias or bradyarrhythmias
Hypertrophic cardiomyopathy and other forms of outflow tract obstruction
Mental or physical impairment leading to inability to exercise adequately
High-degree AV block
Procedure
Exercise Protocols: Bruce protocol is the most widely used
Preparation
Pt assessment; informed consent
No eating or smoking for 3 hr before test
Loose clothing; appropriate footwear
Examine for murmur, gallop, wheezing, rales
Consider withdrawal of medication such as β-blockers that could interfere with test
Absolute Indications for Cessation of Stress Test
Drop in systolic BP (persistently below baseline) despite an increase in workload
Increasing anginal pain
CNS symptoms (eg, ataxia, dizziness, or near-syncope)
Signs of poor perfusion (cyanosis or pallor)
Serious arrhythmias (ie, high-grade ventricular arrhythmias such as multiform complexes, triplets, and runs of VT)
Subject’s request to stop
Relative Indications for Cessation of Stress Test
ST or QRS changes such as excessive ST displacement, extreme junctional depression, or marked axis shift
Fatigue, shortness of breath, wheezing, leg cramps, or claudication
Less serious arrhythmias, including supraventricular tachycardias
Interpretation & Findings
Sensitivity/Specificity: Sensitivity of stress testing without imaging reported in meta-analyses to be 67-72%, sensitivity 69-77%, predictive accuracy 68-74%
ST-segment depression: Represents subendocardial ischemia; abnormal response ≥ 1 mm (0.1 mV) horizontal/downsloping ST-segment depression 0.08 sec past J point; exercise-induced ST-segment depression less specific in presence of baseline EKG abnormalities; amount, time of appearance, duration, and number of leads with ST-segment depression all correlate with probability/severity of CAD; ST depression at lower workload or double product worsens prognosis and increases likelihood of multivessel disease
Downsloping ST-segment depression is a stronger predictor of CAD than horizontal depression. Both are more predictive than upsloping depression. Ischemic ST-segment changes developing during recovery from treadmill exercise in apparently healthy individuals have adverse prognostic significance similar to those appearing during exercise (Circ 1998;97:2117).
Lead V5 outperforms the inferior leads or combination of lead V5 with II, because lead II has a high false-positive rate. Inpts without prior MI and normal resting EKG, precordial leads alone are a reliable marker for CAD and monitoring of inferior limb leads adds little additional diagnostic information. Inpts with normal resting EKG, exercise-induced ST-segment depression confined to inferior leads is of little value for identification of CAD.
ST elevation in leads without Q waves occurs in only 1 of 1000pts. ST elevation on a normal EKG (other than in aVR or V1) represents transmural ischemia caused by spasm or a critical lesion, is very rare (0.1% in a clinical lab), and is very arrhythmogenic and localizes ischemia. If resting EKG shows old MI, ST elevation may indicate wall motion abnormalities or residual viability in the infarcted area.
R-Wave Changes: Many factors affect the R-wave amplitude response to exercise; response does not have diagnostic significance.
LBBB: Exercise-induced ST depression usually occurs with LBBB and has no association with ischemia; ˜0.5% ofpts develop new LBBB during exercise; exercise-induced LBBB associated with adjusted relative risk of 2.78 for death and major cardiac events (Jama 1998;279:153).
RBBB: Exercise-induced ST depression usually occurs with RBBB in leads V1-V3 and is not associated with ischemia; ST depression in lead V5-V6 or in inferior leads has same significance as in normal EKG.
LVH with Repolarization Abnormalities: Associated with decreased specificity of exercise testing, but sensitivity is unaffected
Resting ST-Segment Depression: Identified as marker for adverse cardiac events inpts with and without known CAD; 2-mm additional exercise-induced ST-segment depression or downsloping depression of 1 mm or more in recovery useful markers for dx of CAD
Attenuated heart rate response to exercise is predictive of increased mortality and CAD incidence (Framingham). Inpts having a stress test, chronotropic incompetence is an independent predictor of all-cause mortality (Circ 1996;93:1520; Jama 1999;281:524).
PVC: Frequent ventricular ectopy (> 7 PVC/min) during exercise predicted an increased 5-yr risk of death, and frequent ectopy in recovery period was an even stronger predictor (Nejm 2003;348:781).
Women: Exercise-induced ST depression less sensitive in women than men; exercise EKG commonly viewed as less specific in women than men; significant gender differences are modest and do not preclude use of treadmill exercise testing in women; possible explanations offered include greater prevalence of mitral valve prolapse and syndrome X in women, differences in microvascular function (leading perhaps to coronary spasm), and possibly hormonal differences
Digoxin: Produces abnormal exercise-induced ST depression in 25-40% of apparently healthy normal subjects; prevalence of abnormal responses directly related to age; repolarization effects alleviated 2 wk post cessation of administration
β-Blockers: Exercise testing may have reduced diagnostic value due to inadequate heart rate response; β-blockers should not be stopped inpts exhibiting possible sx of ischemia.
Flecainide: Associated with exercise-induced ventricular tachycardia
Scoring of Results: Pretest likelihood of CAD can be estimated (Table 4.1) on basis of pt’s age, sex, and description of chest pain (typical angina: substernal chest discomfort with characteristic quality and duration, provoked by exertion/emotional stress, relieved by rest/TNG; atypical angina pain meeting 2 of above characteristics; noncardiac chest pain meets ≤ 1 of the typical angina characteristics) (J Am Coll Cardiol 1983;1:574)
Duke treadmill score formula: Exercise time − (5 × ST deviation) − (4 × exercise angina) with 0 = none, 1 = nonlimiting, and 2 = exercise-limiting
Typical score is −25 to +15. Pts can be stratified to low risk (score + 5 or above), moderate risk (score −10 to +4), and high risk (score −11 or below) categories. In the Duke study, 60% of low-riskpts had no coronary stenosis > 75%, 16% had only
single-vessel > 75% stenosis, 74% of high-riskpts had 3-vessel or left main CAD, and 5-yr mortality was 3%, 10%, and 35% for low-, moderate-, and high-risk groups, respectively (Circ 1998; 98:1622). Prognosis can be formulated using the nomogram in Figure 4.2. Score may have reduced prognostic accuracy in subjects > age 65 (Ann IM 2000;132:862).
single-vessel > 75% stenosis, 74% of high-riskpts had 3-vessel or left main CAD, and 5-yr mortality was 3%, 10%, and 35% for low-, moderate-, and high-risk groups, respectively (Circ 1998; 98:1622). Prognosis can be formulated using the nomogram in Figure 4.2. Score may have reduced prognostic accuracy in subjects > age 65 (Ann IM 2000;132:862).
Table 4.1 Pretest Probability of CAD Based on Age, Sex, and Pain Description | |||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||
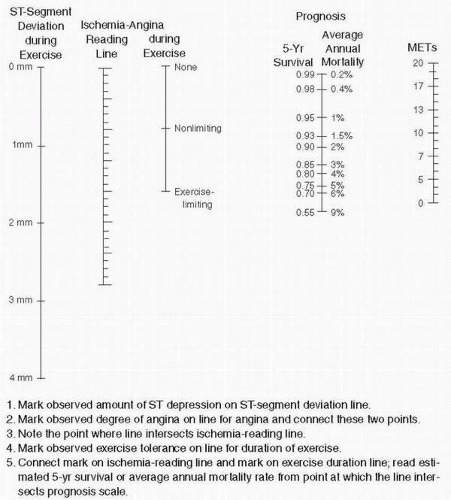 Figure 4.1 Duke Treadmill Score Nomogram (J Am Coll Cardiol 1999;33:1756) |
4.2 Radionuclide Imaging
Circ 2003;108:1404; J Am Coll Cardiol 2003;42:1318
Indications
Uses of Radionuclide Testing after Acute MI: Assessment of RV/LV function with rest radionuclide angiography; detection of stress-induced ischemia by stress myocardial perfusion imaging, measurement of infarct size by rest myocardial perfusion imaging
Uses of Radionuclide Testing in Pts with Unstable Angina: Identification of ischemia in the distribution of the “culprit” lesion or in remote areas with stress myocardial perfusion imaging; assessment of severity/extent of disease inpts with ischemia with rest and stress myocardial perfusion imaging; measurement of baseline LV function with radionuclide angiography
Uses of Radionuclide Testing in Detection and Assessment of Chronic Ischemic Heart Disease: Dx of ischemia with exercise or with pharmacologic myocardial perfusion imaging (for subjects with pacemakers or those unable to exercise); assessment of ventricular performance (rest or exercise) by radionuclide angiography or gated sestamibi imaging; assessment of myocardial viability in patients with LV dysfunction in planning revascularization [restredistribution Tl-201 imaging, stress-redistribution-reinjection Tl-201 imaging (J Am Coll Cardiol 2002;39:1151), or PET F18 fluorodeoxyglucose imaging]; identifying lesions causing myocardial ischemia, if not otherwise known with exercise or pharmacologic myocardial perfusion imaging; risk stratification before noncardiac surgery with pharmacologic or exercise perfusion imaging; assessment of LV performance with rest or exercise radionuclide angiography or gated sestamibi perfusion imaging; assessment of possible restenosis after PTCA or CABG with exercise or pharmacologic perfusion imaging
Uses of Radionuclide Imaging in Myocarditis and Cardiomyopathies: Determination of initial and serial LV and RV performance in myocarditis or dilated, hypertrophic, and restrictive cardiomyopathy with rest radionuclide angiography; initial and serial evaluation of LV function inpts receiving chemotherapy with doxorubicin with rest radionuclide angiography; differentiation of ischemic and dilated cardiomyopathy with exercise or pharmacologic perfusion imaging; assessment of myocardial ischemia in hypertrophic cardiomyopathy
In general, thepts who benefit most from a stress test with SPECT perfusion scan at the outset are those with an intermediate (15-90%) pretest likelihood of CAD. Exercise EKG stress testing alone is the first test of choice inpts with a likelihood of CAD < 15% (based on age, gender, type of chest pain presentation, number of CAD risk factors, EKG findings at rest). If suchpts demonstrate an ischemic ST-segment response that might represent a false-positive test outcome or fail to reach 85% of maximal predicted heart rate, repeat testing with SPECT perfusion imaging indicated (J Am Coll Cardiol 1998;31:1286).
Contraindications
For ischemic disease, same as those under stress testing
Procedure
Nuclear cardiology applications utilize a gamma camera for either planar or SPECT imaging (tomographic reconstructions derived from gamma camera that rotates aroundpt). Tomographic imaging allows for better separation of myocardial and other nonmyocardial structures and individual coronary artery beds and is inherently quantitative.
Equilibrium or gated blood pool radionuclide angiography most commonly utilizes technetium-99m (Tc-99m) pertechnetate bound to red blood cells. Acquisition of images is synchronized with the EKG QRS complex, with the cardiac cycle divided temporally into frames and corresponding frames from all cycles added together for an acquisition
time ranging from 2 to 10 min. This approach generates reliable LV and RV ejection fraction values and offers a means for assessing regional wall motion. Studies can be acquired by both planar and SPECT approaches.
time ranging from 2 to 10 min. This approach generates reliable LV and RV ejection fraction values and offers a means for assessing regional wall motion. Studies can be acquired by both planar and SPECT approaches.
Myocardial perfusion imaging can employ thallium-201 (Tl-201), Tc-99m sestamibi, or Tc-99m tetrofosmin. Tl-201 is very efficiently extracted by viable myocardial cells and distributes in proportion to regional blood flow. Retention is an active process that is a function of cell viability and cell membrane integrity. “Redistribution” of the isotope generally occurs in previously ischemic zones, while defects related to infarcted or scarred myocardium typically do not “redistribute” and remain fixed. Imaging at 24 hr or after reinjection of Tl-201 may show viable but hypoperfused segments not identified by a standard redistribution study at 3-4 hr after isotope injection. Studies can be performed at rest, with exercise or dobutamine stress, or after the myocardial hyperemia induced by iv dipyridamole or adenosine.
Tc-99m sestamibi has a shorter half-life than Tl-201 (6 hr vs 73 hr) and has more favorable imaging characteristics (higher emission energy, less scattered radiation). Like Tl-201, Tc-99m requires intact cell membrane processes for retention.
PET employs radiotracers such as fluorine-18 (F-18, half-life 110 min), nitrogen 13 (N-13, half-life 10 min), or rubidium-82 (Rb-82, half-life 75 sec) coupled to physiologically active molecules to assess myocardial perfusion or metabolism.
Myocardial perfusion imaging is most commonly used in conjunction with exercise stress, with Tl-201 administered iv at peak exercise. The pt then exercises for an additional 30-60 sec. Images are acquired immediately after and again 3-4 hr after Tl administration. Because sestamibi undergoes only a small amount of washout after initial myocardial uptake, distinguishing between transient, stress-induced perfusion defects and fixed perfusion defects requires administration of 2 separate injections, one during stress and one at rest.
Adenosine/Dipyridamole Stress Test Protocol
Contraindications: Unstable angina or acute MI; asthma; systolic BP < 100 mm Hg; hemodynamically severe aortic stenosis; high-degree AV block; pregnancy
Pretest Instructions: No aminophylline for 48 hr prior to study; no coffee, tea, cola, chocolate, or other caffeinated beverages for 24 hr prior to study; npo 3 hr prior to study
Protocol: Adenosine, 0.84 mg/kg in 40 mL NS, infused over 6 min; inject radionuclide at 3 min or dipyridamole, 0.57 mg/kg (maximum dose 60 mg) in 25-50 mL NS, infused over 4 min; inject radionuclide with 5 min of infusion; monitor vital signs and EKG q 1 min; image 45 min after completion of infusion and preferably after pt has eaten; ambulation (1 mph) during infusion increases image quality (J Nucl Cardiol 2000;7:439)
Side Effects: Headache, nausea/vomiting, dizziness, hypotension, chest pain
Termination Criteria: Same as for exercise stress test
Dobutamine Stress Test Protocol
Contraindications: Unstable angina or acute MI; obstructive hypertrophic cardiomyopathy; hemodynamically severe aortic stenosis; any symptomatic tachyarrhythmia; systolic BP > 180 mm Hg and/or diastolic BP > 110 mm Hg; pregnancy
Protocol: Dobutamine continuous iv infusion at 5 μgm/kg/min for 3 min; increase to 10, 20, 30, 40 μgm/kg/min at 3-min intervals; monitor VS and EKG q 3 min; inject radionuclide after 1 min at maximal infusion rate; continue infusion an additional 2 min; if target heart rate not obtained, administer atropine 0.5-1 mg iv; image 5-10 min after completion of infusion
Side Effects: Palpitations, dizziness, chest pain
Termination Criteria: Same as for exercise stress test
Interpretation & Findings
Comparison with Stress Echo: Advantages of stress radionuclide imaging include higher technical success rate, higher sensitivity (1-vessel CAD), better accuracy in evaluating ischemia if rest wall motion abnormalities are present, and a more extensive published database. Advantages of stress echo include higher specificity, more extensive evaluation of cardiac anatomy, greater convenience/availability, and lower cost (Circ 1999;99:2829). In a meta-analysis, exercise echo had a sensitivity of 85% and specificity of 77%; exercise SPECT had a sensitivity of 87% and specificity of 64-73%; vasodilator SPECT had a sensitivity of 89% and specificity of 75%. Unlike exercise stress testing, ST depression ≥ 2 mm inpts undergoing adenosine SPECT is not specific for CAD (Am Hrt J 2000;140:937). Vasodilator SPECT has better sensitivity, especially inpts on β-blockers; echo stress has better specificity (Am Hrt J 2001;142:934; Cardiol 2001;95:112). Both echo and SPECT performed significantly better than exercise testing without imaging (Jama 1998;280:913).
Chest pain may occur during adenosine administration in the absence of ischemia (May Clin Proc 1995;70:331).
The diagnostic sensitivity/specificity of SPECT imaging is not diminished inpts with LVH and repolarization abnormalities.
Pts with LBBB have an increased prevalence of false-positive septal perfusion defects. Pharmacologic stress is preferred for such subjects.
Normal-stress SPECT sestamibi images are associated with a 0.6% average annual event rate (death or nonfatal MI). Pts with abnormal images had an annual event rate of 7.4% (J Am Coll Cardiol 1998;32:57).
In a retrospective study, 4649pts with intermediate-risk Duke treadmill scores and normal/near-normal exercise SPECT perfusion images had cardiovascular survival rates of 99.8% at
1 yr, 99.0% at 5 yr, and 98.5% at 7 yr; cardiac survival free of MI was 96.6% at 7 yr; survival free of MI or revascularization was 87.1% at 7 yr (Circ 1999;100:2140).
1 yr, 99.0% at 5 yr, and 98.5% at 7 yr; cardiac survival free of MI was 96.6% at 7 yr; survival free of MI or revascularization was 87.1% at 7 yr (Circ 1999;100:2140).
Results predicting high risk for adverse outcomes inpts with known or suspected CAD include severe resting or exercise LV dysfunction (LVEF < 35%), high-risk treadmill score (score ≤ −11), stress-induced large perfusion defect (particularly if anterior) or multiple moderate perfusion defects, and large, fixed perfusion defect or moderate stress-induced perfusion defect with LV dilatation or increased lung uptake. Conversely, in men with and without diabetes and in nondiabetic women with no known CAD and a negative test, predicted time to 1% risk was > 1 yr even at age 80 (J Am Coll Cardiol 2003;41:1329).
4.3 Echocardiography
J Am Coll Cardiol 2003;42:954; Circ 2003;108:1146
Indications
Two-dimensional echocardiography provides images of the heart, paracardiac structures, and great vessels. Interposition of an air-filled lung between the body surface and heart limits examination inpts with COPD. Pts on ventilators,pts who cannot be rotated into a lateral position, andpts with incisions may not have satisfactory precordial or apical windows. TEE may avoid most of these limitations.
Valvular Heart Disease
Evaluation of Heart Murmurs: Indicated for murmur inpts with cardiorespiratory sx, murmur in asymptomaticpts if clinical features
indicate a moderate probability that the murmur is reflective of structural heart disease, murmur in asymptomaticpts in whom dx of heart disease cannot be reasonably excluded
indicate a moderate probability that the murmur is reflective of structural heart disease, murmur in asymptomaticpts in whom dx of heart disease cannot be reasonably excluded
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


