Chapter 14 Cardiac rehabilitation and secondary prevention
INTRODUCTION
Cardiac rehabilitation is an accepted form of management for people with cardiac disease. Initially rehabilitation was offered mainly to people recovering from a myocardial infarction (MI), but now encompasses a wide range of cardiac problems. More than 275 000 people have a MI each year in England and, while more than 40% of these are fatal, the survival rate is improving (Department of Health 2006). With more people surviving the peri-infarct period, the incidence of people with chronic heart failure (CHF) is increasing. These changes in mortality and morbidity present challenges for health professionals involved in organizing and delivering rehabilitation programmes. The aim of cardiac rehabilitation is to enable people to regain full physical, psychological and social status and, in order to optimize long-term prognosis, to promote and implement coronary heart disease (CHD) secondary prevention measures. Cardiac rehabilitation should be an integral part of both acute care and long-term follow-up, but provision and uptake remains inconsistent (Beswick et al 2004, Bittner & Sanderson 2006, Brodie et al 2006). In the United Kingdom (UK), the National Service Framework for CHD (Department of Health 2000) was written to provide guidance on the management of people with coronary heart disease. One of the standards of recommended care is the provision of a multidisciplinary programme of cardiac rehabilitation and secondary prevention. There is large variation in the format and organization of rehabilitation programmes, both within and between countries, but traditionally most encompass a period of exercise training, education sessions, psychosocial support and advice/counselling for both the patient and their family. In addition to people with a MI or CHF, participants may include those with an implanted cardioverter defibrillator (ICD), pacemaker and following coronary artery bypass graft surgery (CABG) and transplantation. Demographic changes mean there is greater involvement of elderly people, which is both a reflection of an ageing population and expansion of health care, and there is also a gradual increase in the uptake of cardiac rehabilitation amongst women. The secondary prevention aspect of the programmes has an important place in the reduction of risk factors. Physically inactive people have approximately double the risk of CHD compared with active people and the implementation of regular exercise is considered to decrease their risk factor profile by the same magnitude as smoking cessation (Albu et al 2006, Department of Health 2004).
EVIDENCE BASE FOR CARDIAC REHABILITATION
With the increased evidence base for the benefits of cardiac rehabilitation, and particularly exercise training, many clinical guidelines for the management of people with cardiac problems recommend participation in a rehabilitation programme (National Institute for Clinical Excellence 2001, 2003, Scottish Intercollegiate Guidelines Network 2002). While there is a plethora of research supporting the benefits of cardiac rehabilitation programmes, the era in which the information was obtained has to be taken into consideration. Early studies concentrated on the benefits of exercise for post-MI patients in whom traditional management had restricted early activity – which differs from the early resumption of activity practised today. Early studies did not include the benefits of revascularization, thrombolysis and protective drug therapy (Franklin 2004, Kovoor et al 2006, Zwisler et al 2005). The restriction of studies to exercise training also limits their applicability to comprehensive cardiac rehabilitation programmes, as the sum of a programme may be greater than its individual parts. Additionally, women and the elderly were often excluded from research (Witt et al 2004). Consequently, most of the research findings in the 1960s and 1970s are no longer directly applicable to the management of people following a MI. The meta-analyses of Oldridge et al (1988) and O’Connor et al (1989) which have been used extensively to promote cardiac rehabilitation are now of limited usefulness and have been superseded by more recent studies (Jolliffe et al 2000, Rees et al 2004, Taylor et al 2004).
Current research continues to suggest that rehabilitation programmes confer benefit to participants in all domains of their lives, with a focus on patient selection and organization of the programme. Unfortunately the methodology of some research studies is of low quality (i.e. small sample number, restricted age/gender, lack of randomization), which limits extrapolation of their findings to clinical practice. Another problematic area for interpreting research findings is the choice of outcome measures (Sanderson et al 2004). The importance of improvement in health-related quality of life is recognized in many studies, but there is lack of consensus as to the most appropriate measuring tool (Shephard & Franklin 2001, Taylor et al 1998). The SF-36 and SF-12 Health Status Questionnaires have been widely used, but concern has been expressed as to their ability to detect change when used for serial measurements (Ni et al 2000, Smith et al 2000). Some studies suggest anxiety and depression improve after a period of rehabilitation and have been commonly measured by the Hospital and Depression Scale (Zigmond & Snaith 1983), but this is thought to be relatively insensitive to change in this group of patients (McGee et al 1999). With the difficulties in selecting robust and appropriate outcome measures for quality of life issues, studies frequently use physiological or exercise endurance indices to measure responses to exercise training. However, these also have methodological issues concerning the influence of motivation and relevance of results (Ingle et al 2005). It has been suggested that a suitable measure for people with ICDs is the confidence to exert themselves physically (Sears et al 2004). Measurements of general activity, using pedometers, are considered to demonstrate a close relationship with changes in functional status (Evangelista et al 2005) and may be a more appropriate outcome for determining the response to rehabilitation programmes.
The organization of cardiac rehabilitation programmes is varied, with some focusing primarily on education and psychosocial intervention (Mendes de Leon et al 2006) and others offering only exercise training. The World Health Organization (WHO) (Frye 1993) definition of cardiac rehabilitation encompasses the concept of comprehensive cardiac rehabilitation programmes. Research suggests the inclusion of exercise training is a key element in eliciting benefits both in facilitating return to function and secondary prevention (Leon et al 1991, National Institute for Clinical Excellence 2003, Taylor et al 2004). There is considerable variation across and between patient groups in the type and setting of exercise training (Hansen et al 2005). Many studies have concentrated on aerobic exercise owing to concerns regarding the effects of resistance training on cardiac function, but there is growing evidence that a mix of endurance and strength exercises are both safe and optimize the benefits (Adams et al 2006, Delagardelle et al 2002, Jonsdottir et al 2005, Levinger et al 2005). Concern that some patients may develop myocardial remodelling, as a result of participating in early activity (Jugdutt et al 1988, Kloner & Kloner 1983), has been alleviated by other work indicating that exercise does not contribute to the onset of remodelling (Cannistra et al 1999, DuBach et al 1997, Giannuzzi et al 1993, Myers et al 2000). The benefits of low- intensity exercise in the early stages of a programme are thought be similar to those of higher intensity (Blumenthal et al 1988, Goble et al 1991, Worcester et al 1993) and adoption of low-intensity exercise would facilitate both adherence and safety. Women have previously been under-represented in cardiac rehabilitation and may require specific programmes, based in the community or at home, to improve their uptake and adherence (Sanderson & Bittner 2005, Todaro et al 2004, Witt et al 2004). Some studies recommend inspiratory muscle training in people with chronic heart failure (Dall’Ago et al 2006).
The duration of the period of exercise training is influenced by many factors, such as physiological and psychological state (Kovoor et al 2006), objectives and adherence. Secondary prevention requires a prolonged period of training (Brubaker et al 2000) and adherence and uptake to a programme may be influenced by social support (Husak et al 2004) age, gender (Todaro et al 2004) and location of training (Grace et al 2005). The lack of consensus on an optimal period of exercise training for different groups of patients and an absence of a robust prediction model to determine the magnitude of benefit each patient may receive from a rehabilitation programme (Pierson et al 2004, Shen et al 2006) places an emphasis on assessment, joint goal setting and regular re-evaluation of response. Few studies have included a prolonged follow-up period, but any benefits appear to be quickly lost on cessation of regular exercise training.
The diversity of programmes and client groups makes it difficult to determine the cost-effectiveness of cardiac rehabilitation and this is compounded by differences in health provision among countries where this has been investigated. A survey within the UK calculated the cost per patient to be of the order of £490 (Beswick et al 2004) while an American review had higher average costs of $2054 and determined that participation prolonged survival by an additional 1.82 years at a cost of $1773 per/life-year saved (Georgiou et al 2001). It has been suggested that cardiac rehabilitation is more cost-effective than thrombolytic therapy and coronary bypass surgery (Ades et al 1997).
There has not been any reported increase in adverse events during either supervised or unsupervised exercise training following the inclusion of people who were previously considered a high risk: i.e. CHF and ICDs (Davids et al 2005, Fitchet et al 2003, Pashkow et al 1997) However, there is a paucity of information on the occurrence of adverse events outside research studies, which usually include highly selected patients who undergo formal exercise tests.
PROVISION OF CARDIAC REHABILITATION
Goals
Rehabilitation should combine exercise with patient education and counselling, which provide:
Patients should be offered an individually tailored package from this menu of care, according to their needs and preferences (Scottish Intercollegiate Guidelines Network 2002). Individual packages are usually described as spanning four phases of care (Coats et al 1995):
Phase I in-hospital period (average 3–5 days)
Phase II immediate post-discharge/convalescence stage (2–6 weeks)
Phase III supervised outpatient programme (6–12 weeks)
Phase IV long-term maintenance programme in the community.
Considerable variation exists in the model, timing, content and delivery of outpatient cardiac rehabilitation. Rehabilitation may be offered in supervised groups, within a hospital or community setting, or as part of a home-based package. Some programmes include education, psychosocial and exercise components while others provide only exercise training; some programmes are confined to 4–6 weeks’ duration while others last for up to a year. In order to maximize benefit and adherence, the rehabilitation professional must match the appropriate model of care to each patient’s individual needs. Increasing use of national clinical guidelines and audit tools have led to increased standardization, quality and effectiveness of cardiac rehabilitation services (American Association of Cardiovascular and Pulmonary Rehabilitation 2004, American College of Sports Medicine 2006, Fletcher et al 2001, Leon et al 2005, Scottish Intercollegiate Guidelines Network 2002).
By whom should cardiac rehabilitation be delivered?
Exercise rehabilitation should be delivered by a team of clinical and exercise specialists who are skilled in cardiovascular assessment, risk stratification, patient monitoring, exercise prescription, goal setting and behavioural management. The team needs to be able to deal with concurrent medical and psychosocial issues and combine the art and science of exercise prescription and delivery, i.e. the art of integrating strategies for behaviour change in order to enhance exercise compliance and long-term adherence, with the science of exercise prescription (American College of Sports Medicine 2006). There should also be joint working and close liaison with British Association of Cardiac Rehabilitation (BACR) Phase IV instructors (or their equivalent) who accept patients for long-term exercise in the community. Physiotherapists are key members of the team as they have specialist skills in the assessment, exercise prescription and rehabilitation management of multi-pathology patients, as well as being health educators and exercise advisors (Association of Chartered Physiotherapists in Cardiac Rehabilitation 2006, Jolliffe et al 2000). The Association of Chartered Physiotherapists Interested in Cardiac Rehabilitation (ACPICR) in the UK has developed guidelines for practice (Association of Chartered Physiotherapists in Cardiac Rehabilitation 2006) and a competency document outlining the physiotherapist’s role and required knowledge, skills and standard of performance in cardiac rehabilitation.
BENEFITS OF EXERCISE TRAINING
Improved exercise capacity
The development of cardiovascular endurance is the primary objective for CHD patients. Endurance training, defined as any activity which uses large muscle groups, can be sustained for a prolonged period and is rhythmic and aerobic in nature, results in an increase in maximal oxygen uptake (VO2max), i.e. the highest rate of oxygen consumption attainable during maximal exercise. Maximal oxygen uptake is limited:
 peripherally, in particular by the capacity of skeletal muscle to extract oxygen from the blood. This is represented as the difference between the oxygen content of arterial blood and mixed venous blood (arteriovenous oxygen difference
peripherally, in particular by the capacity of skeletal muscle to extract oxygen from the blood. This is represented as the difference between the oxygen content of arterial blood and mixed venous blood (arteriovenous oxygen difference  Consequently an increase in
Consequently an increase in  O2max depends on the potential for inducing central and/or peripheral adaptations.
O2max depends on the potential for inducing central and/or peripheral adaptations.Peripheral changes
In cardiac patients, the increase in VO2max is attributed predominantly to peripheral adaptation. Central changes are associated with prolonged periods of high-intensity training and although in selected patients central changes have been provoked (Ehsani et al 1986, Schuler et al 1992), the high intensity of the training regimen would be inappropriate for the heterogene- ous group of patients eligible for cardiac rehabilitation programmes.
EXERCISE PRESCRIPTION
Principles of exercise prescription
The principles of exercise training are:
Specificity – the adaptations conferred by training are highly specific to:
Intensity of exercise
The intensity of exercise is a critical issue because vigorous activity carries a greatly increased risk of precipitating adverse events such as myocardial infarction or arrhythmias (Willich et al 1993). Frequent, moderate-intensity exercise is recommended for CHD patients since it will optimize benefits without increasing the risk of adverse events (Dafoe & Huston 1997). For individuals with greatly diminished functional capacity, several short bouts (as little as 5–10 minutes) throughout the day may be advisable. There are a number of established methods for prescribing and monitoring intensity, which may be used separately or in combination with one another.
Use of heart rate
Ideally, training heart rate is based on information derived from a maximal or symptom-limited exercise electrocardiogram test (ETT) (Box 14.1). Where a maximal test has been achieved, training heart rate should be set at 60–75% of maximal heart rate (HRmax). If the test was symptom limited, training intensity should be set at 10–20 beats per minute (bpm) below the heart rate at which symptoms were apparent and the patient’s heart rate should be monitored throughout each exercise session. ECG test information is, however, not always available to health professionals. In the absence of test data or if, for diagnostic purposes, a patient performs the exercise test ‘off-medication’, other methods for establishing appropriate training intensity have to be used.
Box 14.1 Exercise tolerance testing
 measurement of functional capacity – on which advice about activities of daily living and a formal exercise prescription may be based
measurement of functional capacity – on which advice about activities of daily living and a formal exercise prescription may be based measurement of acute exercise responses including blood pressure, heart rate, ventilatory responses and detection of exercise-induced arrhythmias.
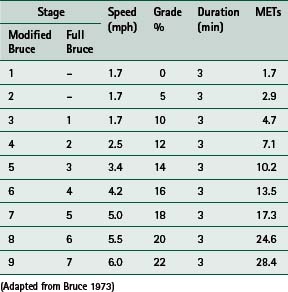
measurement of acute exercise responses including blood pressure, heart rate, ventilatory responses and detection of exercise-induced arrhythmias.Numerous exercise protocols have been developed which utilize a variety of different exercise modes, but in the United Kingdom an incremental treadmill protocol is the traditional test mode. Before acceptance into a Phase III programme, usually 2–6 weeks post MI, a symptom-limited test (i.e. the patient continues until signs or symptoms, which necessitate test termination, are evident) is customary; the Bruce protocol is the most common. Submaximal tests that use a predetermined endpoint such as an age-predicted maximum heart rate are usual before discharge. The modified Bruce protocol is the most commonly used since it introduces two preliminary, less strenuous stages (Table 14.1).
Criteria for terminating an exercise test include:
 marked drop in systolic blood pressure (>20 mmHg) indicating poor left ventricular function or severe coronary disease
marked drop in systolic blood pressure (>20 mmHg) indicating poor left ventricular function or severe coronary disease patient fatigue and/or excessive breathlessness at low workloads, which may simply indicate poor functional capacity but may also be suggestive of serious problems such as heart failure.
patient fatigue and/or excessive breathlessness at low workloads, which may simply indicate poor functional capacity but may also be suggestive of serious problems such as heart failure.Age-adjusted predicted maximal rates can be used (220 bpm minus age in years is one formula) and the training heart rate set at 60–75% of the predicted maximum; this is equivalent to 40–65% VO2max. However, the standard deviation (SD) for maximal heart rate during exercise is ± 10 bpm and some individuals will, therefore, have an actual maximum heart rate 20 bpm higher or lower (2 SD above or below the population mean) than predicted. An alternative approach is to prescribe training at 40–65% of heart rate reserve (HRR – the difference between resting and maximal heart rate). This HRR approach (also known as the Karvonen method) is convenient since it is known that 40–65% of heart rate reserve is equivalent to about 40–65% of VO2max (60–75% of maximal heart rate) although, across the entire range of fitness levels, it is more closely linked to the percentage of oxygen uptake reserve (VO2R): i.e. the difference between resting oxygen consumption and maximal oxygen consumption (American College of Sports Medicine 2006). An example of the HRR method for calculating training heart rate is shown below for an individual with a resting heart rate of 60 bpm and maximal heart rate of 150 bpm.
150 − 60 = 90 (heart rate reserve, HRR)
Training heart rate = 40−65% of heart rate reserve + resting heart rate (RHR)
90 × 0.40 = 36 + 60 (RHR) = 96 bpm (40%)
90 × 0.65 = 59 + 60 (RHR) = 119 bpm (65%)
Use of rating of perceived exertion
Cardiorespiratory and metabolic variables are strongly related to perceived exertion, which is accepted as a valid and reproducible indicator of the intensity of steady-state exercise. Physiotherapists and exercise specialists working in a cardiac rehabilitation setting are recommended to familiarize themselves with the scales of perceived exertion developed by Borg (1998). The Borg 15-point scale and the Borg CR10 scale of perceived exertion, together with patient instructions, are published in the Appendix of Borg’s Perceived Exertion and Pain Scales (Borg 1998). In order to preserve the validity and reproducibility of these scales, their format should not be altered and the patient instructions should be closely followed.
Use of metabolic equivalent values (METs)
Exercise may also be regulated by choice of activities according to their known MET (metabolic equivalent) values (for which tables are available in most exercise physiology texts). If an individual assesses walking at 3 miles per hour (mph) as 12–13 on the Borg RPE scale (corresponding to 60% of VO2max), then activities of comparable MET value can be prescribed in the knowledge that they will present an appropriate training stimulus. Knowledge of MET values is also important in terms of excluding those activities that might pose a risk to certain individuals. Skipping (8–12 METs) or freestyle swimming (9–10 METs), for example, would be entirely inappropriate for someone with a peak capacity of 7 METs.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree