Implantable cardioverter-defibrillators (ICDs) are similarly designed, though the pulse generator tends to be larger owing to the need for the increased size of the power source. Most often, the pulse generator produces a noticeable and easily palpable protrusion on the chest wall. These devices may be single-chamber, dual chamber, or part of a biventricular pacing system. They can be identified radiographically by the presence of one or more coils on the lead which extends into the right ventricle. The coiled appears as a “notched” or “rippled” portion of the lead which is thicker and more radiodense than the remaining portion of the lead (Figure 22.2).
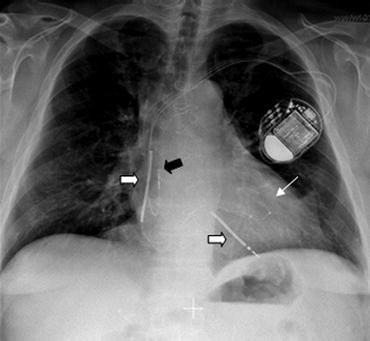
Biventricular devices also tend to have larger pulse generators. The additional size is necessary to accommodate the power source as well as a requisite increase in the amount of circuitry. These devices are designed not only to defibrillate a patient if necessary but also to deliver pacing stimuli as frequently as possible. The additional lead tends to be of smaller diameter, and achieves its location preferably on the lateral wall of the left ventricle by exiting the right atrium through the coronary sinus, extending posteriorly around the left ventricle (Figure 22.3) and then into a lateral venous branch where it is held in place by the shape of the lead tip and the tortuosity of the venous branch.
All of these devices are capable of transcutaneous transmission of data. This is done in the hospital or cardiology/electrophysiology clinic with a device analyzer. These computers are manufacturer-specific, and can provide information about battery status, pacemaker/ICD parameters, and lead diagnostic information, as well as events programmed to be monitored or treated by the device.
Figure 22.2 PA chest film showing the usual appearance of a dual-chamber ICD system. Note the pulse generator in the left chest wall, with leads entering the vasculature and coursing to a position overlying the right atrium and right ventricle. Note that the atrial (pacing) lead is of smaller diameter than the ventricular (ICD) lead (black arrow). Note also the appearance of the coils (white arrows) on the ventricular lead (superior vena cava and right ventricle).
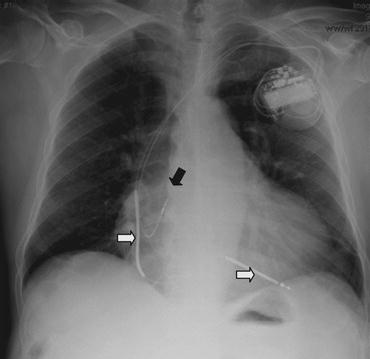
Figure 22.3 PA chest film showing the appearance of a biventricular pacemaker system. Note the pulse generator with three leads exiting the header. The right ventricular (ICD) lead can be identified by the presence of the coils on the lead and the slightly larger diameter (block white arrows). The right atrial lead has an intermediate diameter (block black arrow). The coronary sinus lead has the smallest diameter, and can be seen coursing through the coronary sinus to a location in a lateral branch on the left ventricular free wall (thin white arrow).
22.3 INDICATIONS FOR THE IMPLANTATION OF PACEMAKERS AND ICDS
This section addresses the indications for the various forms of cardiac device therapy. It is intended to provide a brief overview rather than a detailed discussion, so that the hospitalist may begin to formulate a plan of care even before a cardiologist or electrophysiologist become involved. A much more detailed description of the indications for and contraindications to pacemaker or ICD implantation can be found in the most recent guidelines.
In general, pacemakers are designed to supply a pacing stimulus to a chamber of the heart where the native conduction system has failed to supply a sufficient pacing stimulus of its own. As such, they are implanted for acquired or congenital disorders affecting the cardiac conduction system producing a heart rate that is not sufficient. This can result from disorders of the SA node (Table 22.1), the AV node (Table 22.2), or a combination thereof.
Despite the effects of carotid sinus syndrome and neurocardiogenic syncope on both the sinus and AV node, pacemaker implantation is often not helpful. Pacemaker implantation is indicated for recurrent syncope due to spontaneously occurring carotid sinus stimulation that induces ventricular asystole of more than three seconds. Pacemaker implantation is not indicated for hypersensitive cardioinhibitory response to carotid sinus stimulation without symptoms or with vague symptoms, or for situational vasovagal syncope in which avoidance behavior is effective and preferred.
Implantable cardioverter-defibrillators (ICDs) are designed primarily to treat ventricular tachyarrhythmias, though all ICDs do possess pacing capabilities. As such, they are indicated in patients who have a history of ventricular tachycardia or ventricular fibrillation, or who are at high risk for developing these potentially lethal rhythm disturbances. Common indications and contraindications for ICD implantation are listed in Table 22.3. Those patients who meet criteria for ICD implantation and have a QRS duration >120 ms may obtain benefit from an implantable defibrillator with cardiac resynchronization therapy, i.e. placement of a biventricular ICD with a coronary sinus lead (Table 22.4). These devices have been studied and shown to be of benefit in the treatment of New York Heart Class II, III or IV heart failure in a patient on optimal medical therapy due to either ischemic and non-ischemic processes. Benefits of cardiac resynchronization provided by these devices include improved exercise tolerance, improvement in NYHA functional class, improved quality of life, and survival benefit.
Table 22.1 Pacing Indications and Contraindications for Sinus Node Dysfunction.
| Pacing indications for sinus node dysfunction | |
| Indications | Symptomatic sinus node dysfunction, including sinus pauses of more than 3 seconds in the awake patient |
| Symptomatic chronotropic incompetence | |
| Symptomatic bradycardia resulting from essential pharmacotherapy (beta blockers post-MI) | |
| Contraindications | Asymptomatic sinus node dysfunction |
| Sinus node dysfunction when symptoms suggestive of bradycardia are documented in the absence of bradycardia | |
| Sinus node dysfunction due to non-essential pharmacotherapy |
Table 22.2 Pacing Indications and Contraindications for AV Node Dysfunction.
| Pacing indications for AV node dysfunction | |
| Indications | Third-degree and advanced second-degree block associated with bradycardia resulting in symptoms |
| Third-degree and advanced second-degree block associated with arrhythmias requiring medications producing symptomatic bradycardia | |
| Third-degree and advanced second-degree block in a patient who is asymptomatic in sinus rhythm who has a period of asystole greater than 3 seconds, or a ventricular escape rate less than 40 beats per minute | |
| Third-degree and advanced second-degree block in a patient who is asymptomatic in atrial fibrillation with bradycardia with a pause of greater than 5 seconds | |
| Second-degree block with associated symptomatic bradycardia | |
| Advanced second-degree or third-degree block associated with neuromuscular disease (myotonic dystrophy, Erb dystrophy, peroneal muscular atrophy, etc.) | |
| Contraindications | Asymptomatic first-degree AV block |
| Asymptomatic Type I second-degree (Wenkebach) AV block | |
| Any AV block which is transient and not likely to recur (Lyme disease, drug toxicity, transient increases in vagal tone) |
Table 22.3 Implantable Defibrillator Indications and Contraindications.
| Indications for ICD implantation | |
| Indications | Patients who are survivors of cardiac arrest (VT or VF) after evaluation and treatment of reversible cause |



