Chapter 3 Cardiac output
FACTORS THAT DETERMINE CARDIAC OUTPUT
If you consider the sequence of events reviewed in Chapter 2 you will see that the volume of blood that can be pumped by the heart will be determined by a number of factors including the frequency of pumping, the efficiency of ventricular filling and the efficiency of ventricular emptying.
Heart rate
The usual resting heart rate of 65–75 beats/min reflects a substantial degree of bradycardic vagal tone, so heart rate can be increased moderately either by reducing that vagal influence or by increasing sympathetic tachycardic drive, or both. Any increase above the intrinsic pacemaker frequency of 100 beats/min, however, relies entirely on sympathetic activation. The sympathetic nerves act through activation of β-adrenoceptors and drugs that antagonize this action (the so-called β-blockers) are frequently used in patients for whom exercise is prescribed as a rehabilitative aid after heart attacks. The reduced capacity to produce normal tachycardia is an important factor in determining the absolute intensities of exercise that these individuals are able to undertake and must also be borne in mind if absolute heart rate is being used to quantify their exercise workload (see Chapter 11, p. 131).
The standard equation to calculate maximum heart rate (HRmax) for an adult of a known age is:
but it is important to bear in mind that this can be applied only to adult subjects. In children, maximum heart rate appears to vary little or not at all with age and remains around a little more than 200 beats/min until approximately 18 years (see Chapter 9, p. 113). In addition, the generalization of HRmax falling by 1 beat/min per year has been derived from population studies, and absolute maxima vary by up to 10 beats/min between people of any given age. For this reason, if heart rate is to be used for quantifying workload during exercise then it is preferable to determine each individual’s HRmax directly.
appears to be more accurate than the standard one (Miller et al 1993).
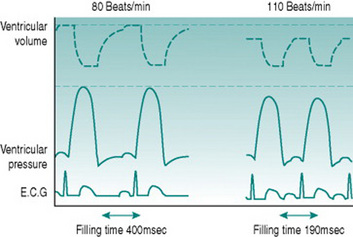
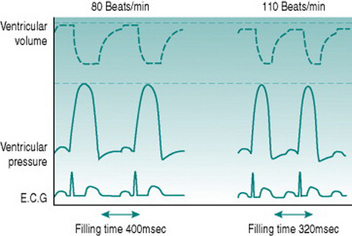
Ventricular filling time
Simple calculation would indicate that a threefold elevation of heart rate should increase cardiac output by the same amount, but it is clear from looking at the pressure–flow relationships during the cardiac cycle (Fig. 3.1) that the situation is not as straightforward as this. As heart rate increases, the interval between successive ventricular contractions decreases so that the absolute time available for refilling falls. With moderate tachycardia this is not a major problem, since most filling occurs during the first 100 ms of diastole when the atrioventricular pressure gradient is greatest. As heart rate increases further, however, filling efficiency falls dramatically. With typical ventricular action potential durations of 300–350 ms it can be calculated that a heart rate of 180 beats/min (1 beat every 330 ms) would actually allow no time for filling at all. Moreover, if there was no diastolic relaxation period then there could be virtually no coronary perfusion to the left ventricle, so myocardial metabolism could not be sustained. Since maximal exercise capacity involves heart rates in young adults of 200 beats/min and cardiac outputs in excess of 20 L/min, this scenario is clearly too simplistic.
The answer is that, in fact, ventricular action potential duration does not remain constant as heart rate increases, because the sympathetically released catecholamines that produce tachycardia also reduce the cycle time of the voltage-gated calcium channels (Fig. 3.2). In consequence, the normal HRmax for a 20-year-old of 200 beats/min is associated with an endocardial ventricular action potential plateau phase of about 200 ms rather than the 350 ms seen at rest, allowing around 100 ms for ventricular filling. In consequence, stroke volume falls only slightly even at maximal work capacity.
Atrial function
For any finite diastolic period available for ventricular filling, the efficiency of the filling process depends on the pressure gradient between atria and ventricles. This is itself determined by the efficiency of atrial filling, which reflects the pressure gradient from the peripheral veins to the heart. During exercise, two factors facilitate venous return. One is the increased negative pressure inside the thorax during inspiration that results from larger tidal volume. The other is external compression of veins in the moving limbs by muscle contraction (muscle pumping) and in the abdomen by abdominal wall muscle activity during expiration. The importance of the leg muscle pump for efficient cardiac filling is illustrated by comparing circulatory responses to arm and leg exercise. During arm exercise, heart rate rises more with given work increments, because the absence of muscle pumping limits stroke volume (see Chapter 7, p. 89).