Cardiac Masses
Suzanne V. Arnold
High-Yield Findings
Thrombi usually occur in areas of low flow—for example, alongside an akinetic left ventricular (LV) wall
Vegetations are typically on the low-pressure side of the valve
Assess tumors for size, shape, and physiologic significance (i.e., disruption of flow, displacement of normal structures)
Describe what you see to help develop a differential diagnosis
Common Pitfalls
Beware of normal variants and pathologic variations of normal structures
All masses should ideally be seen in more than one plane
Use color flow and/or intravenous (IV) contrast to ensure mass is not artifactual
Normal Variants and Pathologic Variations of Normal Structures
Normal Variants
LV false tendons: Fibromuscular bands that extend across the LV from the septum to the free wall (Fig. 18-1A).
Moderator band: A muscular band that extends across the right ventricle (RV) from the septum to the base of the papillary muscles of the RV.
Prominent or calcified papillary muscles of the mitral valve (MV) or tricuspid valve (TV).
Crista terminalis: A vertical ridge of smooth myocardium that extends between the right side of the orifice of the superior vena cava (SVC) to the right side of the valve of the inferior vena cava (IVC).
Eustachian valve: A valve flap at the distal end of the IVC that directs blood into the right atrium (RA) and toward the interatrial septum. When prominent and filamentous, it is called a Chiari network (Fig. 18-1B).
“Coumadin ridge”: Artifact from a prominent fold of tissue that separates the left superior pulmonary vein and the left atrial appendage can be confused on TEE with a thrombus.
Pathologic Variations of Normal Structures
Dense mitral annular calcification
Lipomatous infiltration of the atrial septum (Fig. 18-2)
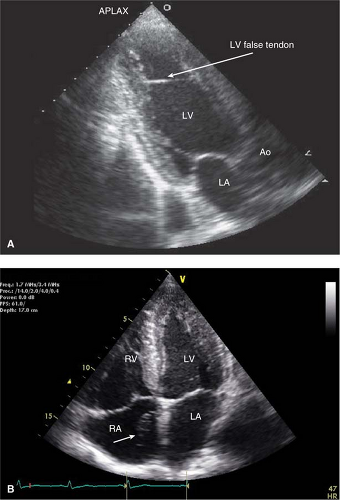
Figure 18-1. A: APLAX with bright linear echodensity seen in distal LV consistent with false tendon. B: A4C with bright linear echodensity seen in RA consistent with a Chiari network (arrow).
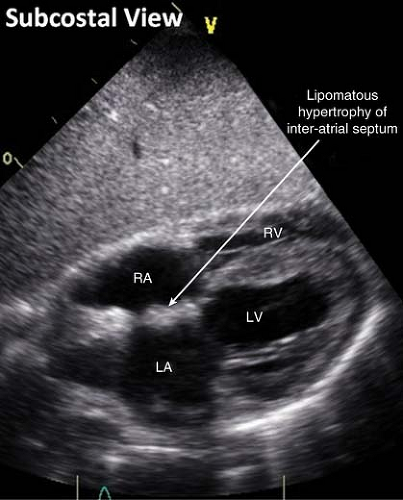
Figure 18-2. Subcostal view showing the typical “dumb-bell” appearance of interatrial septal hypertrophy.
Epicardial fat
LV trabeculations (e.g., non-compaction, chest wall deformities)
Lambl’s excrescences: Filiform strands (typically small mobile homogeneous echo-dense structures <1 cm) that originate at valve closure sites. They are usually thought of as a normal variant (found in 70% to 80% of adults), but embolism has been reported (most likely due to superimposed thrombus)
Artifacts
The use of ultrasound may produce artifacts that give the appearance of masses within the heart. The use of imaging from multiple planes, color Doppler interrogation, and contrast administration will reduce misinterpretation; however, use of alternative imaging modalities may be needed to exclude important pathology. Examples of common ultrasound artifacts are listed below (Fig. 18-3).
Side-lobe artifact—secondary, oblique “lobes” of ultrasound energy occur off the main beam axis. In general, because of the lower energy of the side-lobes, this does
not commonly affect the image that is displayed. However, occasionally when there is a bright specular reflector (e.g., catheter, wire) detected by the side-lobe, this may be mis-assigned to the main beam and noticeable in the echo-free spaces of the heart or its surroundings.
not commonly affect the image that is displayed. However, occasionally when there is a bright specular reflector (e.g., catheter, wire) detected by the side-lobe, this may be mis-assigned to the main beam and noticeable in the echo-free spaces of the heart or its surroundings.
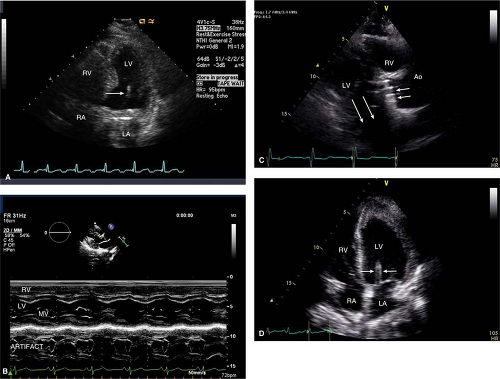 Figure 18-3. Ultrasound artifacts: (A) Side-lobe artifact places the image of the RV pacing wire in the LV (arrow). Note reverberation artifact below mechanical MV, (B) PLAX M-mode shows duplication artifact of MV in the echo-free space behind the LV. (C) PLAX in patient with mechanical bi-leaflet valve in the aortic position exhibiting shadowing or attenuation artifact (long arrows) as well as reverberation (short arrows), (D) Comet-tail artifact (arrows) in patient with pleural effusions and pulmonary edema (note apical thrombus secondary to hypereosinophilic syndrome).
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|