Cardiac Manifestations of Systemic Illness
Mohammed K. Saghir
Thomas K. Kurian
Daniel H. Cooper
Amyloidosis
Classifications
Primary—most common, results from plasma cell dyscrasia and accumulated light chain protein. Cardiac involvement is common with mean survival of 4 months following development of heart failure.
Secondary—amyloid fibrils result from accumulation of acute phase reactant, serum amyloid A. This is often secondary to underlying chronic inflammatory conditions.
Hereditary—secondary to mutations in apolipoprotein I and transthyretin (TTR). Autosomal dominant. Can result in heart failure.
Senile—age related, secondary to accumulation of wild-type transthyretin. Can have significant cardiac involvement. Generally less aggressive than AL.
Atrial—related to age and valvulopathy. Protein is atrial natriuretic peptide and released in response to wall stretch. Uncertain clinical significance.
Hemodialysis—related to accumulation of B2-microglobulin in long-term hemodialysis patients.
Echocardiographic Findings
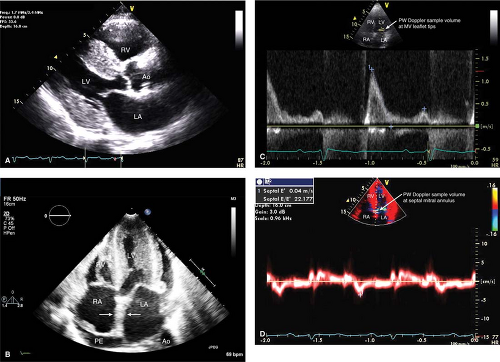
See Figure 19-1.
Early manifestations include progressive diastolic dysfunction and increasing biventricular wall thickness. The LV cavity is normal to slightly reduced in size though it may become dilated late in the disease.
A granular “sparkling” pattern may be noted in the myocardium. Given new harmonic imaging this is not specific for cardiac amyloidosis and can be seen in severe hypertensive heart disease, hypertrophic cardiomyopathy, and glycogen storage disease.
Amyloid deposits on cardiac valves with valvular thickening and insufficiency.
Advanced cardiac involvement from amyloid may show LV dilatation, LV failure, biventricular thickening, atrial septal thickening (specific for amyloid), biatrial dilation, and pericardial effusion.
Restrictive mitral filling pattern with markedly reduced mitral annular peak velocities.
Key Point:
Atrial septal infiltration/thickening is specific for cardiac amyloidosis in the correct clinical picture and in combination with other suggestive echocardiographic findings.
Carcinoid
Background
Slow growing neuroendocrine tumor often arising from enterochromaffin cells in the gastrointestinal tract. Cardiac involvement occurs following metastasis to the liver and exposure of the heart to active substances such as serotonin and bradykinin. Generally symptoms are limited to the right heart as the lungs clear carcinoid-related substances.
Echocardiographic Findings
See Figure 19-2.
Carcinoid substances cause valvular thickening and restricted leaflet movement resulting in a “club”-like appearance of the TV leaflets with severe TR and variable stenosis. The pulmonic valve may be similarly affected. These valvular changes lead to RV volume overload and eventually failure.
Subcostal views may reveal liver metastases. Check for hepatic vein systolic flow reversal in this view as a marker of severe TR.
Rarely, myocardial metastases may be seen.
Key Point:
Left-sided valvulopathy may occur in a patient with carcinoid disease if an intracardiac right-to-left shunt is present.
Hypereosinophilic Syndrome
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree