1. How have the cardiac manifestations of human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS) changed over the years?
Cardiac manifestations of AIDS up until the early 1990s would not infrequently include pericardial disease, myocarditis, dilated and infiltrative cardiomyopathy, pulmonary disease with pulmonary hypertension, arrhythmias, and marantic or infectious endocarditis. Because patients tended to be younger, very little coronary atherosclerosis was noted. As highly active antiretroviral therapy (HAART) has emerged as an effective treatment for HIV, HIV has transformed from a fatal infection to a chronically managed disease.
Cardiovascular disease is now the second most common cause of death in antiretroviral therapy (ART)-treated patients worldwide. HIV patients have a higher incidence of traditional cardiovascular risk factors, such as male gender, smoking, advanced age, glucose intolerance, insulin resistance, and dyslipidemia. They also have a higher incidence of nontraditional cardiac risk factors, including polysubstance abuse, lifestyle choices, immune dysregulation, and effects of ART.
Over the next decades, children born with vertically transmitted HIV will survive to adulthood, with attendant cardiac complications from chronic inflammation, drug therapy, and immunosuppression.
2. What are HIV-related cardiac complications?
Since the advent of ART in the 1990s, the incidence of HIV-related complications has significantly decreased, but cardiac complications include:
3. How common is pericardial effusion?
Pericardial effusion is an incidental finding in about 11% of HIV-infected patients and up to 30% of AIDS patients with CD4+ T cell counts (CD4 counts) less than 400 cells/μL who have cardiac echocardiograms. The effusions are typically small and patients are usually asymptomatic. The presence of an effusion is an independent predictor of mortality in these patients. It only rarely progresses to tamponade, which is more common in end-stage, cachectic patients who develop elevated intrapericardial pressures caused by low right-sided filling pressures (low-pressure tamponade). The effusion is mostly transudative. Mycobacterium tuberculosis and M. avium are the principal causes of infectious pericarditis. Rarely, Kaposi sarcoma can bleed into the pericardium, causing tamponade physiology.
4. Is HIV myocarditis or cardiomyopathy common?
In different series, one-third to one-half of patients in the pre-HAART era (or where HAART therapy was not available) dying of AIDS had lymphocytic infiltration at autopsy. Of these patients, 80% had no other pathogens identified. Additionally, up to 10% of endomyocardial specimens in HIV patients have evidence of other infections (e.g., Coxsackie B, Epstein-Barr virus, adenovirus, and cytomegalovirus).
The initiation of HAART therapy has significantly reduced the incidence of cardiomyopathy, likely due to both reduction in HIV itself and reduction in the presence of opportunistic infections.
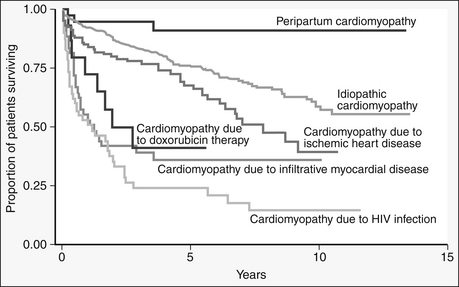
HIV is thought to cause myocarditis from direct action of HIV on myocytes or indirectly through toxins. Patients with HIV and cardiomyopathy have a worse prognosis than those with cardiomyopathy due to other causes of cardiomyopathy (Fig. 46-1). Heart failure caused by HIV-associated left ventricular dysfunction is most commonly found in patients with the lowest CD4 counts and is a marker of poor prognosis. Despite the association of HIV and myocarditis and cardiomyopathy, in patients with HIV and with cardiomyopathy, other possible causes of heart failure (e.g., ischemic, valvular, and toxin-related heart failure) should be excluded.
5. How is HIV cardiomyopathy treated?
A standard heart failure regimen should be used as tolerated, including angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs), beta-adrenergic blocking agents (β-blockers), aldosterone antagonists, diuretics for volume overload, and digoxin for advanced disease. Additionally, nutritional and electrolyte deficiencies should be replenished.
6. Why is infective valvular endocarditis a rarity in AIDS?
Valvular devastation usually seen with bacterial infections does not occur in HIV patients because of impairment of autoimmune response. Patients who have hemodynamically significant valvular disease warrant valve replacement if their HIV is well controlled. Fulminant infective endocarditis can occur in late AIDS with high mortality. Patients with AIDS rarely will develop marantic (noninfectious) endocarditis, with large, friable, sterile thrombotic vegetations. These can be associated with disseminated intravascular coagulation (DIC) and systemic embolization.
7. What malignancies can affect the heart in AIDS/HIV?
Kaposi sarcoma is associated with herpesvirus 8 in homosexual AIDS patients. This tumor is often found in the subepicardial fat around surface coronary arteries. About 25% of AIDS patients with systemic Kaposi sarcoma had incidental cardiac involvement, with death as a result of underlying opportunistic infections. Non-Hodgkin lymphoma is more common in HIV-positive patients, with a poor prognosis. Leiomyosarcoma is rarely associated with Epstein-Barr virus in AIDS patients.
8. Can nutritional deficiencies be responsible for HIV myopathy?
Only gold members can continue reading.
Log In or
Register to continue
Related

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 Pericardial effusion/tamponade
Pericardial effusion/tamponade Dilated cardiomyopathy (systolic and diastolic dysfunction)
Dilated cardiomyopathy (systolic and diastolic dysfunction) Marantic (thrombotic) or infectious endocarditis
Marantic (thrombotic) or infectious endocarditis Cardiac tumors (Kaposi sarcoma, lymphoma)
Cardiac tumors (Kaposi sarcoma, lymphoma)