(x axis) and pericardial pressure (y axis) is (see Fig. 9.1):
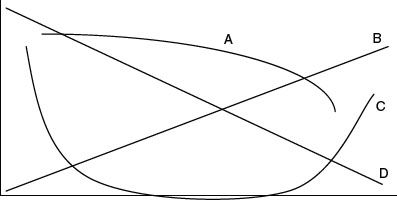
A. A
B. B
C. C
D. D
E. None of the above
37. A 6-month-old child with coarctation of the aorta returns after end-to-end anastomosis repair of the coarctation. The blood pressure is 136/70 mm Hg. Of the following, which pharmacologic agent is not an accepted therapy for hypertension after coarctation repair?
A. Esmolol IV
B. Labetalol IV
C. Nitroprusside IV
D. Hydralazine IV
E. Isoproterenol IV
38. A 6-month-old child with single ventricle who was previously palliated with an aortopulmonary shunt is now back from the operating room after a bidirectional cavopulmonary anastomosis. His oxygen saturation is 65%. Of the following, which is the least likely etiology for the systemic desaturation?
A. Pleural effusion
B. A decompression vein
C. Low arterial paCO2
D. Atrioventricular valve regurgitation
E. Elevated pulmonary vascular resistance
39. The therapeutic options for the treatment of junctional ectopic tachycardia includes all the following except which one?
A. Amiodarone IV
B. Hypothermia
C. Procainamide IV
D. Adenosine IV
E. Digoxin IV
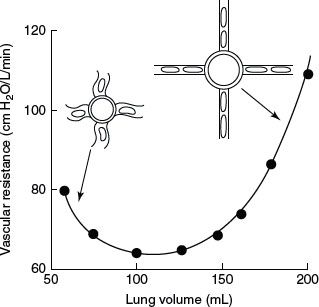
40. The curve in Figure 9.2. depicts (x and y axis) which of the following relationship?
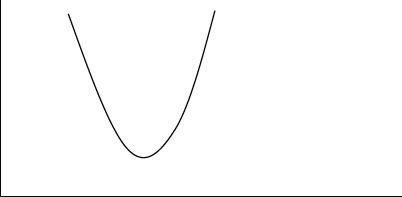
A. Lung volume versus pulmonary vascular resistance
B. Pericardial volume and pericardial pressure
C. Pericardial fluid and heart rate
D. Hematocrit and viscosity
E. Viscosity and pulmonary vascular resistance
41. Of the following pediatric patients, which would be the least likely to have an elevated right atrial pressure of 14 mm Hg?
A. A 5-year-old child with restrictive cardiomyopathy
B. A 3-year-old child after an atrial septal defect repair with a large pericardial effusion
C. A 3-month-old child with Ebstein’s anomaly and moderate tricuspid valve regurgitation
D. A 4-month-old child after tetralogy of Fallot repair with a residual RVOT gradient of 60 mm Hg
E. A 12-year-old child with chronic dilated cardiomyopathy
42. A neonate with the diagnosis of infracardiac total anomalous pulmonary venous drainage returns after corrective surgery. A pulmonary artery catheter is left in place and the pulmonary artery pressure is 3/4 systemic. The left atrial pressure is 8 mm Hg. What is the appropriate first step in managing this patient?
A. Echocardiogram and if needed catheterization
B. Inhaled nitric oxide
C. Inhaled nitric oxide and sildenafil IV
D. Milrinone IV
E. Milrinone and sildenafil IV
43. All the following therapies have been utilized for catecholamine-resistant shock after cardiopulmonary bypass except which one?
A. Vasopressin
B. Steroids
C. Phenoxybenzamine
D. Thyroxine
E. ECMO
44. The following are expected findings on an electrocardiogram for the lesions and/or repairs listed except which one?
A. Tetralogy of Fallot repair and complete right bundle branch block
B. Anomalous left coronary artery from the pulmonary artery and Q waves in leads I and avL
C. Subaortic resection and left bundle branch block
D. Transposition of the great arteries after arterial switch and Q waves in leads II, III, and avF
E. Truncus arteriosus repair and complete right bundle branch block
45. A 3-year-old child with single left ventricle and who has had a “fenestrated” Fontan operation returns from the cardiac catheterization laboratory. The following data are reported: pulmonary artery pressure 18 mm Hg, left atrial pressure 5 mm Hg, and oxygen saturation 99%. There is no pressure gradient between a simultaneous pulmonary artery wedge pressure and an end-diastolic pressure of the ventricle of 4 mm Hg. Which of the following statements is the least likely to be true?
A. The transpulmonary gradient is 13 mm Hg
B. The fenestration is patent
C. The patient has elevated pulmonary vascular resistance
D. The patient has normal end-diastolic pressure for a Fontan surgery patient
E. There is no evidence for atrioventricular valve or pulmonary venous stenosis
46. The LV pressure/volume curve is shown for a patient at times A and B (Fig. 9.3). The increase in stroke volume shown at time B is due to which of the following?
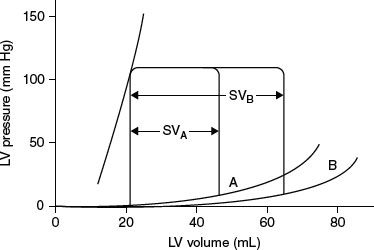
A. Increase in contractility
B. Afterload reduction
C. Improved lusitropy
D. Increased preload
E. Increased heart rate
47. A 4-year-old child is admitted to the cardiac intensive care unit with a history of a cerebrovascular accident. The electrocardiogram shows biatrial enlargement and intermittent atrial flutter. The echocardiogram shows dilated atria, LV ejection fraction of 62%, normal LV end-diastolic dimension, and an RV pressure estimated at 55% systemic pressure. Which of the following is the most likely diagnosis?
A. Dilated cardiomyopathy
B. Restrictive cardiomyopathy
C. Acute myocarditis
D. Hypertrophic cardiomyopathy
E. Pulmonary hypertension and RV failure
48. The following are vasoconstrictors that are part of the group of mediators that comprise of the neurohumoral response in heart failure except which of the following?
A. Angiotensin II
B. Arginine vasopressin
C. Norepinephrine
D. B-type natriuretic peptide
E. Endothelin
49. The electrocardiogram in Figure 9.4. obtained in a 3-year-old child who was admitted with cardiovascular collapse.
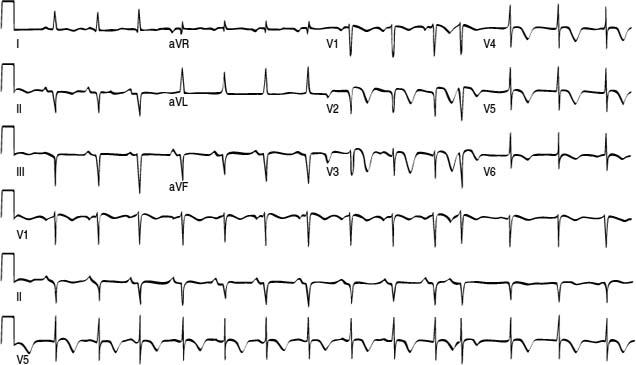
Which of the following is the most likely diagnosis?
A. Anomalous left coronary artery from the pulmonary artery
B. Ectopic atrial tachycardia
C. Myocarditis
D. Kawasaki disease and coronary thrombosis
E. Congenitally corrected transposition of the great arteries
50. A patient, after corrective surgery, is admitted with borderline LV function and milrinone is initiated. If LV pressure-volume curves are plotted before and after milrinone was started (see Fig. 9.5), which of the following would best characterize its effects?
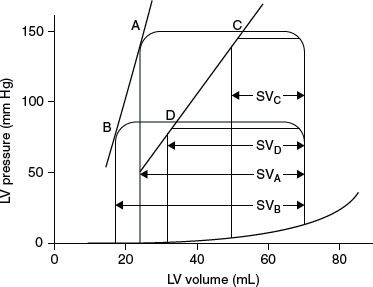
A. C to B
B. B to A
C. C to A
D. B to D
E. C to D
ANSWERS
1. ANSWER: A. The effect of lung inflation on pulmonary vascular resistance (see U-shaped curve in Figure 9.6.) is such that resistance is at its nadir and the lung volume is at FRC. Any volume below FRC results in under-inflation and thus atelectasis and alveolar hypoxia (reactive vasoconstriction) while any volume above the FRC results in over-inflation and thus increased airway pressure and vascular stretch (secondary vasoconstriction).
2. ANSWER: D. Any distortion of the pulmonary artery (in-situ thrombus, stenosis, external compression, etc.) would impede pulmonary blood flow and result in an elevated SVC pressure. This elevation in SVC pressure could result in opening of vestigial veins that would then drain venous blood into the heart, thus leading to systemic desaturation. In this case, there was insufficient decompression of these veins as the SVC pressure was still very elevated.
Other conditions that would result in similar hemodynamic profile (increased SVC pressure but without a concomitant increase in left atrial pressure) would be etiologic factors such as elevated pulmonary vascular resistance, pleural effusion, atelectasis, hyperinflation, pulmonary vein stenosis, etc. The other conditions listed in the answer section would result in not just an elevated SVC pressure but also an elevated left atrial pressure.
3. ANSWER: B. Junctional ectopic tachycardia (JET) can be common after cardiac surgery in infants after surgery for tetralogy of Fallot, VSD, or common atrioventricular canal. This postoperative dysrhythmia would be extremely uncommon after a bidirectional cavopulmonary anastomosis. Management includes hypothermia, diminution of catecholamines, sedation, and antidysrhythmic agents such as amiodarone or procainamide with establishment of atrioventricular synchrony.
4. ANSWER: A. The anatomy is consistent with asplenia (double-outlet right ventricle and common atrioventricular canal with pulmonary outlet obstruction as well as total anomalous pulmonary venous connection). These neonates can have ectopic atrial tachycardia and is often under-diagnosed.
Junctional ectopic tachycardia is more commonly associated with infants after VSD surgery (tetralogy of Fallot or common atrioventricular canal). The other types of SVT are not commonly associated with postoperative situations.
5. ANSWER: E. After the first few days of life, a neonate with transposition of the great arteries is not likely to have elevated pulmonary vascular resistance. The other lesions at the listed ages are well known to have elevated pulmonary vascular resistance before surgery and can therefore have exacerbation of pulmonary vascular resistance after cardiopulmonary bypass.
6. ANSWER: A. Tetralogy of Fallot after cardiac surgery is characterized by a restrictive right ventricular physiology with an elevated CVP while the left atrial pressure remains normal. The other cardiac defects will usually have a higher left atrial pressure than CVP for different reasons. In total anomalous pulmonary venous return, the left atrium and ventricle are relatively noncompliant and borderline hypoplastic; hence, a higher filling pressure is required. In transposition of the great arteries, it is not uncommon to have some degree of LV dysfunction (depending on age) and a higher left atrial pressure is often noted especially in older infants with this diagnosis. In infants with anomalous left coronary artery from the pulmonary artery, the left ventricle is usually dilated and with significant dysfunction so that the filling pressure after surgery will be elevated. Lastly, an infant with coarctation of the aorta and VSD would more likely to have a higher left atrial pressure than CVP.
7. ANSWER: E. Pulmonary hypertension would lead to an elevated CVP with a normal or slightly elevated left atrial pressure. An elevated left atrial pressure will be seen with the other answers: aortopulmonary collaterals and residual VSD will lead to increased pulmonary venous return while LV dysfunction and/or coronary ischemia will lead to higher filling pressures.
8. ANSWER: C. Postcoarctectomy hypertension has a biphasic pattern. The first phase is most likely secondary to surgical stimulation of the sympathetic nerve fibers in the tissue of the aortic isthmus. This process leads to release of norepinephrine (as well as epinephrine) and can be effectively neutralized with preoperative treatment with propranolol. The second phase of postcoarctectomy hypertension occurs after the initial 24 hours and is characterized by an increase in renin and an elevated diastolic pressure. This phase is also associated with mesenteric arteritis.
9. ANSWER: C. Elevated PA pressure after the Fontan operation can be categorized into (1) abnormal transpulmonary gradient (>5 mm Hg): etiologies include elevated pulmonary vascular resistance, pulmonary artery distortion, pulmonary issues (e.g., pleural effusion, pneumothorax, atelectasis), and pulmonary venous obstruction; and (2) normal transpulmonary gradient (but abnormal LA pressure): etiologies include ventricular dysfunction, unfavorable mass/volume changes (diastolic dysfunction), AV valve regurgitation, subaortic stenosis, AV dyssynchrony, and pericardial effusion.
10. ANSWER: C. In a CVP pressure tracing, the a wave is produced by atrial contraction and the c wave is caused by ventricular contraction against a closed tricuspid valve (with the valve bulging into the right atrium). The v wave is secondary to atrial filling. The x descent follows the c wave and is due to the tricuspid valve being pulled away from the right atrium during ventricular systole and the y descent occurs due to the blood filling the right ventricle. Cannon a waves have a myriad of etiologic factors, including right atrium contracting against an obstructed tricuspid valve (tricuspid stenosis, right atrial masses, right atrial myxoma, complete heart block, and atrioventricular dyssynchrony) and resistance to right ventricular filling (pulmonary hypertension or pulmonary stenosis).
11. ANSWER: D. The oxygen excess omega (Ω) can be calculated with the formula:
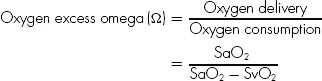
This neonate with an oxygen saturation of 90% and a SvO2 of 60% will have a calculated omega (Ω) of 3. Thus, the same neonate with poor ventricular function and SvO2 of 30% will have a calculated omega (Ω) of 1.5, which is much lower than the neonate described in the question.
12. ANSWER: A. The mediators that are decreased in pulmonary hypertension include prostacyclin, matrix metalloproteinases, nitric oxide, and thrombomodulin. The other mediators listed above are all elevated in pulmonary hypertension, and these also include Von Willebrand factor, P-selectin, plasminogen activating inhibitor, fibrinopeptide A, tissue plasminogen activator (tPA), angiotensin II, epinephrine, insulin-like growth factor, basic fibroblast growth factor, and platelet-derived growth factor A.
13. ANSWER: E. While it is possible to have a pulmonary hypertensive crisis after surgery for a VSD in an infant, a transesophageal echocardiogram is necessary to rule out the possibility of a significant residual VSD as the etiology for the elevated pulmonary artery pressure. Treatment for pulmonary hypertension should not be initiated until this possibility is ruled out. Otherwise, the measures to reduce pulmonary vascular resistance may actually further exacerbate hemodynamic instability if a significant residual VSD is present.
14. ANSWER: E. The Vaughn Williams classification for antiarrhythmic agents is as follows:
•Class I—local membrane stabilizing activity: blocks fast sodium channel.
IA- Moderate sodium blockade
Moderate phase 0 depression/intermediate slowing of conduction/prolongation of repolarization/prolongation of action potential and effective refractory period (quinidine, procainamide, and disopyramide).
IB- Weak sodium blockade
Minimal phase 0 depression/little slowing of conduction/shortening of repolarization/shortening of action potential and effective refractory period (lidocaine, mexiletine, and phenytoin).
IC- Strong sodium blockade
Marked phase 0 depression/marked slowing of conduction/little effect on repolarization/little effect on action potential and effective refractory period (flecainide, encainide, and propafenone).
•Class II—blocks β-adrenergic receptors (β-blockers).
•Class III—prolongs duration of cardiac action potential and repolarization but not conduction; blocks potassium channel (amiodarone, sotalol, bretylium).
•Class IV—blocks slow calcium channel and increasing effective refractory period of the AV node and slows conduction and reduces automaticity of sinus and AV nodes (verapamil).
15. ANSWER: A. The anticoagulants commonly used in the cardiac intensive care setting with their mechanisms of action:
•Aspirin—acetylation of cyclo-oxygenase to inhibit production of thromboxane A2, a platelet aggregator.
•Heparin—a mucopolysaccharide that increase the rate at which antithrombin III neutralize thrombin, factor X, and also IX, XI, and XII.
•Streptokinase—interacts with plasminogen to result in plasmin complex.
•tPA—binds to fibrin.
•Warfarin (Coumadin)—interfere with posttranslational modification of the vitamin-K-dependent coagulation factors (II, VII, IX, X, and proteins C and S).
16. ANSWER: C. A low CVP reading can be due to the pressure transducer above, not below, the level of the heart. The other answers are other causes of a reduced right atrial pressure.
17. ANSWER: E. A reduced oxygen saturation from the right atrium includes all the answers above except increased oxygen delivery, which increases oxygen saturation in the right atrium. An increased oxygen saturation in the right atrium can be due to an atrial level left-to-right shunt, an anomalous pulmonary venous vein, a left ventricular-to-right atrial shunt, increased oxygen delivery, decreased oxygen extraction, increased dissolved oxygen content, or catheter tip position near the renal vein.
18. ANSWER: A. A canal-type VSD with straddling tricuspid valve is a high-risk anatomic substrate for heart block. In addition, a perimembranous VSD is also at some risk for heart block as the bundle of His courses posterior-inferiorly to the defect. The other types of VSD, especially muscular and subpulmonary types, have much less risk for heart block.
19. ANSWER: D. In total anomalous pulmonary venous connection, the left-sided structures are borderline hypoplastic and noncompliant, resulting in relatively high left atrial pressure and tachycardia (although atrial flutter or atrial ectopic tachycardia will need to be ruled out). The other lesions usually do not lead to the left atrial pressure being higher than the right atrial pressure.
20. ANSWER: D. Neosynephrine is a pure α-agonist and is useful in the clinical situation of decreased pulmonary blood flow in the presence of an unrestrictive VSD or single ventricle as any increase in systemic vascular resistance will result in an increase in pulmonary blood flow. An infant with double-outlet right ventricle and transposition physiology would be the least likely to respond favorably to neosynephrine.
21. ANSWER: B. The diagnosis with the distinctive murmur is tetralogy of Fallot with absent pulmonary valve. This lesion is associated with an enlarged main and branch pulmonary arteries that compress the proximal airways. In addition, there is distal airway disease as the serpiginous pulmonary arterioles encircle the distal bronchioles. The prone position can often decrease the proximal airway obstruction due to the massively dilated pulmonary arteries.
22. ANSWER: D. Pulmonary vasoconstrictors include angiotensin II, leukotrienes C4, D4, and E4, prostaglandin F2α, thromboxane A2, and serotonin. Pulmonary vasodilators include acetylcholine, bradykinin, prostaglandin E1, E2, and I2, and nitric oxide.
Epinephrine, norepinephrine, endothelins, histamine, and prostaglandin D2 can have variable effect on the pulmonary circulation.
23. ANSWER: C. The first intervention in a Fontan patient with an elevated PA pressure should be an echocardiogram to rule out pericardial tamponade and to assess myocardial function. A CXR can also be very useful to assess pulmonary parenchyma. An EKG is of secondary importance as the heart rate is not exceedingly high to suggest intra-atrial reentrant tachycardia. A cardiac catheterization can be performed if both the echocardiogram and the CXR are normal to rule out thrombosis and stenosis of the pulmonary arteries. Initiation of IV milrinone and inhaled nitric oxide should be reserved after a diagnosis is made.
24. ANSWER: B. The pathophysiology is excessive pulmonary blood flow and resultant wide pulse pressure and low diastolic pressure. IV dopamine can increase the diastolic pressure as can transfusion of packed RBCs and volume. Decreasing the sedation can also increase the blood pressure. IV milrinone would be very risky given the low diastolic pressure.
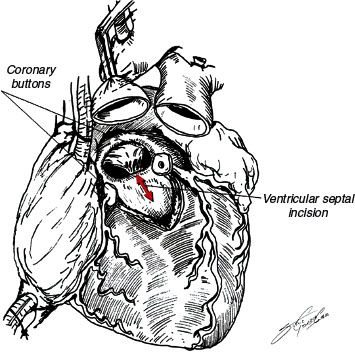
25. ANSWER: A. Ross–Konno operation involves enlargement of the LVOT through a patch; hence, there is the possibility of a residual VSD or RVOT narrowing. LV function with valvar aortic stenosis is often impaired as a result of concentric hypertrophy and suboptimal myocardial protection during bypass. In addition, coronary ischemia can occur with the coronary implantation. Occasionally the neoaortic valve can have some degree of insufficiency. Pulmonary hypertension would be uncommon and unexpected (see Fig. 9.7).
26. ANSWER: D. A pericardial tamponade can lead to elevated right and left atrial pressures with concomitant tachycardia. Junctional ectopic tachycardia, usually more common in infants with corrective surgeries that involve a ventricular septal defect, can result in elevated filling pressures due to atrioventricular dyssynchrony. At 4 weeks of age, an infant with transposition of the great arteries could have an unprepared left ventricle and thus higher filling pressures. Myocardial depression from either cardiopulmonary bypass or from a coronary transfer complication can both result in myocardial depression. While aortopulmonary collaterals can exist in transposition of the great arteries and result in some left ventricular volume load, it is highly unlikely that the collaterals will lead to an elevated left atrial pressure.
27. ANSWER: A. Infants with asplenia and infants who had repair of total anomalous pulmonary venous return can have increased likelihood of ectopic atrial tachycardia. Reentrant type of supraventricular tachycardia mostly likely would have a sudden onset and would have responded to adenosine, which is very effective in converting reentrant type of supraventricular tachycardia. Junctional ectopic tachycardia is usually observed in infants who had corrective surgery that involved VSD closure (such as tetralogy of Fallot or truncus arteriosus). Lastly, ventricular tachycardia in a postoperative setting is usually associated with myocardial ischemia.
28. ANSWER: B. Ischemic bowel syndrome is usually associated with left-sided obstructive lesions such as hypoplastic left heart syndrome, coarctation, and aortic stenosis. Truncus arteriosus, with run-off into the pulmonary arteries and with truncal regurgitation, has a low diastolic pressure and therefore suboptimal perfusion to the mesenteric tract. Tetralogy of Fallot, particularly in the absence of excessive pulmonary blood flow from numerous aortopulmonary collaterals, is unlikely to be associated with ischemic bowel syndrome.
29. ANSWER: C. Milrinone usually does not increase heart rate or blood pressure, the components of rate pressure index, an indirect determinant of myocardial oxygen consumption. The other agents all increase heart rate and therefore the rate pressure index or myocardial oxygen consumption.
30. ANSWER: C. The ratio of pulmonary to systemic blood flow can be easily calculated in single ventricle physiology patients by first making several assumptions.
First, the a-v O2 difference between the aorta and the mixed venous source is 25%. Second, there is no significant pulmonary venous desaturation, so that the pulmonary venous saturation is 95% to 100%. Third, the aortic and pulmonary artery saturations are equal (the former measured by pulse oximetry). The equation is (Ao – mixed venous saturation) / (pulmonary venous – pulmonary artery saturation). In this case, the equation is (25%) / (95–83%) or about 2:1.
31. ANSWER: A. After a bidirectional cavopulmonary anastomosis, a myriad of issues can lead to an elevated SVC pressure with a large transpulmonary gradient. In this case, the transpulmonary gradient is 14 mm Hg, which is elevated. Among reasons for this finding would be elevated pulmonary vascular resistance, pulmonary venous obstruction, pulmonary problems such as pleural effusion or pneumothorax, and thrombosis within the cavopulmonary circuit. Poor ventricular compliance would also result in an elevated SVC pressure, but with an increased left atrial pressure.
32. ANSWER: D. The three common risk factors for irreversible pulmonary hypertension include increased pulmonary blood flow, increased pulmonary artery pressure, and cyanosis. Additional risk factors include pulmonary hypoplasia and pulmonary venous hypertension.
Of the choices, the 9-month-old child with transposition of the great arteries is the oldest with all three risk factors (the other lesions with all three risk factors being common atrioventricular canal and truncus arteriosus) and therefore at highest risk for significant pulmonary hypertension after surgery. Children with atrial septal defect are at minimal risk for pulmonary hypertension, as they have only one of the three risk factors. Children with ventricular septal defects have more risk if the defect is unrestrictive.
33. ANSWER: D. A hypercyanotic spell in tetralogy of Fallot is thought to be a decrease in systemic vascular resistance leading to increased right-to-left shunting and cyanosis. A β-blocker such as esmolol can be utilized to decrease heart rate and possibly decrease the right ventricular outflow tract narrowing. Neosynephrine, an α-agonist, will increase systemic vascular resistance and thereby force more flow to the pulmonary circulation via the right ventricular outflow tract. Oxygen, albeit of limited benefit, can improve oxygenation particularly if the etiology for the cyanosis is partly from pulmonary disease. Isoproterenol, a pulmonary and systemic vasodilator, can potentially exacerbate the cyanosis by inducing tachycardia and further narrowing of the right ventricular outflow tract. Lastly, fluids and packed red blood cells can increase the flow out the narrowed right ventricular outflow tract and improve systemic oxygenation; packed red blood cells can also increase systemic vascular resistance.
34. ANSWER: B. The hemodynamic profile reveals left atrial hypertension while the right atrial pressure remains normal.
The etiological factors for elevated left atrial pressure include left atrial outlet obstruction (e.g., mitral stenosis), left ventricular dysfunction (systolic or diastolic), hypoplasia of the left ventricle, pericardial tamponade, and atrioventricular dyssynchrony. Anomalous left coronary artery from the pulmonary artery is associated with left ventricular dysfunction that will persist months after surgery. A 2-month-old child with transposition of the great arteries could have a left ventricle that has muscle regression and what is termed an “unprepared left ventricle.” Left-sided obstructive lesions will often have left ventricle hypertrophy, therefore a less compliant left ventricle. Lastly, total anomalous pulmonary venous return has a small and noncompliant left ventricle as a result of the dilated right ventricle. Tetralogy of Fallot patients usually have an elevated right atrial pressure due to restrictive physiology of the hypertrophied right ventricle.
35. ANSWER: B. A patient after tetralogy of Fallot repair has restrictive right ventricular pathophysiology. The right ventricle is noncompliant and has significant diastolic dysfunction. Judicious volume resuscitation will improve cardiac output as the right ventricle often requires a filling pressure >10 mm Hg. An electrocardiogram can be obtained to assess the possibility of junctional ectopic tachycardia. An echocardiogram at this point, while not critical, can be used to assess right ventricular volume status and rule out a significant pericardial fluid collection. Lastly, a milrinone infusion is efficacious as it has lusitropic properties. An isoproterenol infusion will have deleterious hemodynamic consequences of further tachycardia and lower systemic blood pressure.
36. ANSWER: E. The relationship between the pericardial volume and pressure is curvilinear, so choices B and D are incorrect. The curves A and C are also incorrect. The pericardial pressure does not increase with volume until a certain volume threshold is reached, and then the pressure rapidly increases with further increase in volume. The curve C is only partially correct as only the right half of the curve accurately reflects the pericardial volume–pressure relationship.
37. ANSWER: E. Hypertension occurring after coarctation repair is secondary to excess of endogenous catecholamines and can be treated with β-blockade (such as esmolol and labetalol). Vasodilators such as nitroprusside and hydralazine can also be used to lower systemic hypertension. Isoproterenol, a synthetic catecholamine, will increase heart rate and catecholamine state, and is not indicated for this situation.
38. ANSWER: D. In the bidirectional cavopulmonary circulation, any increase in pulmonary vascular resistance can open decompressing veins to result in a shunt of venous blood into the heart (often demonstrable with a contrast echocardiogram). A pleural effusion or any reason for an elevated pulmonary vascular resistance can result in this phenomenon. Low arterial paCO2 can reduce cerebral blood flow, thus indirectly reducing pulmonary blood flow and thus oxygen saturation. Of the choices, atrioventricular valve regurgitation is the least likely to affect systemic oxygenation.
39. ANSWER: D. The pharmacologic agents that have been demonstrated to have efficacy for junctional ectopic tachycardia includes amiodarone, procainamide, and digoxin. Hypothermia has also been shown to reduce the ectopic rate. As this is an ectopic tachycardia, adenosine can be a diagnostic agent but not a therapy for this tachydysrhythmia.
40. ANSWER: A. While the relationships B through E are curvilinear, only the relationship between lung volume and pulmonary vascular resistance is a “U”-shaped curve.
41. ANSWER: C. Restrictive cardiomyopathy patients have characteristically elevated right and left atrial pressures and pulmonary hypertension. A child with a large pericardial effusion will have elevated right atrial pressures. A child with tetralogy of Fallot will have right ventricular hypertrophy and a stiff right ventricle, and this is exacerbated by any residual right ventricular outflow tract obstruction. Finally, a child with chronic dilated cardiomyopathy will have elevated right and left atrial pressures. An infant with moderate tricuspid valve regurgitation, due to a relatively compliant right atrium, can have regurgitation and an enlarged right atrium but without significantly elevated right atrial pressure.
42. ANSWER: A. In patients after repair for total anomalous pulmonary venous drainage, pulmonary hypertension occurs often, but any residual pulmonary venous obstruction should be ruled out first by echocardiogram or, if necessary, cardiac catheterization. Any therapy (inhaled nitric oxide, IV sildenafil, or milrinone) should take place after significant residual pulmonary venous obstruction has been ruled out.
43. ANSWER: C. In catecholamine-resistant shock after cardiopulmonary bypass, vasopressin, steroids, and even thyroxine have been studied and used to ameliorate hemodynamic profile. Extracorporeal membrane oxygenation is used as a last resort in selected cases. Phenoxybenzamine is an α-antagonist and leads to vasodilation.
44. ANSWER: D. Both tetralogy of Fallot and truncus arteriosus surgeries involve significant incisions into right ventricular muscle, resulting in a complete right bundle branch block. Similarly, subaortic muscle resection can result in a left bundle branch block. Q waves in leads I and avL is the classic EKG finding for anomalous left coronary artery from the pulmonary artery. After a successful arterial switch operation, there should not be any Q waves on a 12-lead EKG.
45. ANSWER: B. The catheterization data show transpulmonary gradient of 13 mm Hg (pulmonary artery pressure – left atrial pressure). The patient therefore is likely to have an elevated pulmonary vascular resistance as the transpulmonary gradient is elevated. The end-diastolic pressure of 4 mm Hg is good for a single ventricle. Lastly, the simultaneous pulmonary artery wedge and end-diastolic pressure shows no gradient, thus supporting evidence for no stenosis of the atrioventricular valve or pulmonary venous anatomy. With an oxygen saturation of 99% despite a pulmonary artery pressure of 18 mm Hg, it is not likely that the fenestration is still patent.
46. ANSWER: C. The LV pressure–volume curves show an increase in stroke volume at time B compared to time A. The curves labeled A and B are depicting the end-diastolic pressure–volume relationship. Curve B shows improved diastolic function as the curve is more flat; this results in an increase in stroke volume.
47. ANSWER: B. The history and noninvasive findings are most consistent with restrictive cardiomyopathy, which is a cardiomyopathy characterized by abnormal diastolic function and very dilated atria. The systolic function is often intact. The atrial pressures are elevated, thus affecting pulmonary artery pressures so that there is often pulmonary hypertension. Lastly, children succumb to cerebrovascular accidents, atrial tachydysrhythmias, and sudden death. Acute myocarditis and dilated cardiomyopathy would have decreased LV ejection fraction and increased LV end-diastolic dimension. Children with hypertrophic cardiomyopathy do not have dilated atria but hypertrophied ventricles. Pulmonary hypertension patients sometimes have dilated right atrium from tricuspid regurgitation but left atrium is usually not dilated.
48. ANSWER: D. In heart failure, angiotensin II and arginine vasopressin as well as endothelin are known vasoconstrictors that result in cardiac stimulation and fluid retention. In addition, norepinephrine also stimulates the heart as part of the neurohumoral response in heart failure. B-type natriuretic peptide is a vasodilator and a natriuretic.
49. ANSWER: C. The 12-lead EKG is most consistent with myocarditis. The voltages are diminished, and there are T-wave flattening and inversions. Anomalous left coronary artery from the pulmonary artery would have Q waves in leads I and avL. Ectopic atrial tachycardia usually has an abnormal P-wave axis, although can be in the sinus region (thus mimicking sinus tachycardia). There is no evidence for myocardial infarction as seen with coronary aneurysm and thrombosis. The EKG has no suggested findings consistent with congenitally corrected transposition of the great arteries.
50. ANSWER: A. The LV pressure–volume curves show effects of both afterload reduction (A to B and C to D) as well as increase in inotropic state (line CD to line AB). Milrinone has both afterload reduction and inotropic state properties so would most likely change the pressure volume curve from C (high SVR and poor contractile function) to B (lower SVR and improved contractile function).
SUGGESTED READINGS
Chang AC, et al. Shunt lesions (Chapter 15). In: Chang AC, et al., eds. Pediatric Cardiac Intensive Care. Philadelphia, PA: Williams and Wilkins; 1998:216.
Chang AC, et al. Shunt lesions (Chapter 15). In: Chang AC, et al., eds. Pediatric Cardiac Intensive Care. Philadelphia, PA: Williams and Wilkins; 1998:227.
Chang AC, et al. Left ventricular outflow tract obstruction (Chapter 16). In: Chang AC, et al., eds. Pediatric Cardiac Intensive Care. Philadelphia, PA: Williams and Wilkins; 1998:234–
240.
Chang AC, et al. Left ventricular outflow tract obstruction (Chapter 16). In: Chang AC, et al., eds. Pediatric Cardiac Intensive Care. Philadelphia, PA: Williams and Wilkins; 1998:
251–254.
Hastings LA, et al. Perioperative monitoring (Chapter 19). In: Nichols DG, et al., eds. Critical Heart Disease in Infants and Children. Philadelphia, PA: Mosby; 2006:490–491 (Table 19.4).
Kulik TJ. Pulmonary hypertension (Chapter 32). In: Chang AC, et al., eds. Pediatric Cardiac Intensive Care. Philadelphia, PA: Williams and Wilkins; 1998:500–501.
Kulik TJ. Pulmonary hypertension (Chapter 32). In: Chang AC, et al., eds. Pediatric Cardiac Intensive Care. Philadelphia, PA: Williams and Wilkins; 1998:499 (Table 32.1).
Marino BS, et al. Single ventricle lesions (Chapter 38). In: Nichols DG, et al., eds. Critical Heart Disease in Infants and Children. Philadelphia, PA: Mosby; 2006:790–791.
Markowitz RI, et al. Perioperative radiographic studies (Chapter 27). In: Chang AC, et al., eds. Pediatric Cardiac Intensive Care. Philadelphia, PA: Williams and Wilkins; 1998:415–417.
Nelson DP, et al. Normal physiology of the respiratory system (Chapter 6). In: Chang AC, et al., eds. Pediatric Cardiac Intensive Care. Philadelphia, PA: Williams and Wilkins; 1998:76.
Perry JC, et al. Diagnosis and management of cardiac arrhythmia (Chapter 30). In: Chang AC, et al., eds. Pediatric Cardiac Intensive Care. Philadelphia, PA: Williams and Wilkins; 1998:473–
475.
Perry JC, et al. Diagnosis and management of cardiac arrhythmia (Chapter 30). In: Chang AC, et al., eds. Pediatric Cardiac
Intensive Care. Philadelphia, PA: Williams and Wilkins; 1998:
475–480.
Roth S. Postoperative care (Chapter 13). In: Chang AC, et al., eds. Pediatric Cardiac Intensive Care. Philadelphia, PA: Williams and Wilkins; 1998:168–170.
Smerling AJ, et al. Pulmonary hypertension (Chapter 43). In: Nichols DG, et al., eds. Critical Heart Disease in Infants and Children. Philadelphia, PA: Mosby; 2006:890 (Table 43.4).
Spray TL, et al. Right ventricular outflow tract obstruction (Chapter 17). In: Chang AC, et al., eds. Pediatric Cardiac Intensive Care. Philadelphia, PA: Williams and Wilkins; 1998:257.
Spray TL, et al. Right ventricular outflow tract obstruction (Chapter 17). In: Chang AC, et al., eds. Pediatric Cardiac Intensive Care. Philadelphia, PA: Williams and Wilkins; 1998:263–264.
Wernovsky G, et al. Cardiac intensive care (Chapter 20). In: Allen HD, Driscoll DJ, Shaddy RE, et al., eds. Moss and Adams’ Heart Disease in Infants, Children, and Adolescents. 7th ed. Philadelphia, PA: Lippincott, Williams and Wilkins, 2008:473–475.
Wernovsky G, et al. Single ventricle lesions (Chapter 18). In: Chang AC, et al., eds. Pediatric Cardiac Intensive Care. Philadelphia, PA: Williams and Wilkins; 1998:271–274.
Wernovsky G, et al. Single ventricle lesions (Chapter 18). In: Chang AC, et al., eds. Pediatric Cardiac Intensive Care. Philadelphia, PA: Williams and Wilkins; 1998:274–277.
Wernovsky G, et al. Single ventricle lesions (Chapter 18). In: Chang AC, et al., eds. Pediatric Cardiac Intensive Care. Philadelphia, PA: Williams and Wilkins; 1998:278–281.
Wernovsky G, et al. Single ventricle lesions (Chapter 18). In: Chang AC, et al., eds. Pediatric Cardiac Intensive Care. Philadelphia, PA: Williams and Wilkins; 1998:281–284.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


