Fig. 4.1
Contrast echocardiography: administration of contrast enables a better delineation of the endocardial contours (apical four-chamber view in end-diastole and end-systole) (With courtesy of Dr. P. Burger, Bern)
The use of contrast is not generally recommended for 3D echocardiography in the longitudinal follow-up of patients with cancer. A study about the reproducibility of echocardiographic techniques for sequential assessment of left ventricular ejection in patients with breast cancer did not demonstrate any advantage for the measurement of LV volumes and LVEF [12].
4.1.4 3D Echo
Previous studies have shown 3D echocardiography to have lower interobserver and intraobserver variability probability in comparison to 2D echocardiography [6, 7].
The reason is that 3D echo lowers the probability of chamber foreshortening and allows for accurate identification of the true apex of the heart.
LV volume can be quantified without any preestablished assumption of LV geometry. This is of special interest in dilated ventricles with or without segmental alterations.
Jacobs et al. compared 2D and 3D echocardiography against CMR.
Three-dimensional echo correlated highly with CMR imaging values of EDV, ESV, and EF (r = 0.96, r = 0.97 and r = 0.93 for EDV, ESV, and EF, respectively) [13] (Fig. 4.2).
Fig. 4.2
Three-dimensional echocardiography: calculation of left ventricular volumes and ejection fraction using. (a) End-diastolic frame. (b) End-systolic frame (With courtesy of Dr. P. Burger, Bern)
Sugeng proved that 3D echocardiography is also an accurate modality for serial measurements of systolic function [14].
Furthermore, the test-retest variability by a separate operator has shown lower underestimation of LV volumes by 3D echo than by 2D echo when CMR is the reference technique [15, 16].
In a study of Thavendiranathan, non-contrast 3D echo showed minimal detectable EF differences of 6 %, ESV differences of 14 ml, and EDV differences of 34.8 ml.
In this study, contrast administration did not improve variability in measurements of EF or volumes in this population [17].
3D measures are of big interest for follow-up examinations for which exact plane duplication (what is needed in 2D measures) is almost impossible.
Some underestimation of LV volumes due to suboptimal resolution of trabecularization remains in comparison to MRI. This error can be minimized tracing the endocardium underneath the trabeculations and not on top of them [18, 19].
As a general recommendation, 3D echocardiography should be considered in patients with good acoustic windows.
4.1.5 Diastolic Dysfunction
In the past years, abnormalities of diastolic parameters were described.
Stoddard et al. prospectively evaluated 26 patients before administration of doxorubicin and three weeks after cumulative doses. He described an early enhancement of filling time and isovolumetric relaxation time that preceded and predicted a drop in LVEF of >10 %, occurring up to three months later [20].
Other studies confirmed these early changes of diastolic parameters but were not linked to a predictive value [21].
It should be noted that side effects associated with chemotherapy (e.g., diarrhea) might influence the diastolic parameters due to altered loading conditions in follow-up examinations.
A reduction of transmitral E/A ratio is associated with a reduction in longitudinal strain in patients with preserved LV EF late after treatment.
In summary, early chances of diastolic parameters after chemotherapy might not be useful in predicting late-onset systolic dysfunction.
Nevertheless, evaluation of diastolic function should be a part of comprehensive echocardiographic evaluation in the question of cardiotoxicity.
4.1.6 Strain
The measurement of LVEF by 2D echo is prone to a high variability, which can be higher than the thresholds used to define cardiotoxicity [17].
Furthermore, reduction of LVEF is often a late phenomenon and can be irreversible. Strain imaging seems to hold promise to detect chemotherapy-induced alterations very precisely and at a very early stage.
Myocardial deformation (strain) and the rate of deformation (strain rate) reflect intrinsic contractility of the myocardium.
The decrease in myocardial systolic function induced by anthracyclines could be documented already 2 h after the first anthracycline dose [2].
Histological studies have shown that cardiomyocyte apoptosis is not restricted to a single myocardial layer.
This is in line with the fact that anthracyclines seem to alter global, circumferential, and radial strains (Fig. 4.3).
Fig. 4.3
Abnormal global longitudinal strain of a patient with anthracycline-induced cardiomyopathy. Especially the septal segments exhibit abnormal regional strain (With courtesy of Dr. P. Burger, Bern)
Strain imaging requires a good 2D acoustic window to track endocardial borders correctly. In these cases, strain imaging provides an excellent interobserver and test-retest variability [22].
In a study of Sawaya, 81 women with newly diagnosed breast cancer were treated with anthracyclines followed by taxanes and trastuzumab.
Every three months during their cancer therapy (total of 15 months), a follow-up examination by echocardiography was investigated.
Left ventricular ejection fraction, peak systolic longitudinal, radial, and circumferential myocardial strain were calculated. Patients with a pathological longitudinal strain (GLS <19 %) developed later heart failure.
So in this study, global longitudinal strain predicted subsequent cardiotoxicity, whereas LVEF and radial and circumferential strain could not predict cardiotoxicity [23].
In a study of Fallah-Rad et al., patients who received Herceptin had a decrease in global longitudinal and radial strain but not LVEF as early as three months in patients who later developed cardiotoxicity [24].
Strain rate also decreased in half of patients receiving Herceptin in a study of Hare; only 16 % of those with a decrease in strain rate had a drop in EF ≥10 % [25].
However, whether early deformation measurements reflect heart failure in the subsequent years has to be proven by further studies.
Negishi tried to determine the best means of early detection of subsequent reduction of EF in patients with breast cancer treated with trastuzumab (with or without anthracyclines). The strongest predictor of cardiotoxicity was ΔGLS. An 11 % reduction was defined as the optimal cutoff which predicts a subsequent reduction of EF with sensitivity of 65 % and specificity of 94 %.
Patients with a reduction of GLS of <8 % compared with initial measurements were classified as not to be clinically meaningful, whereas those >15 % are very likely to be of clinical significance [26].
Although these findings suggest strain and strain rate as useful parameters with regard to screening for cardiotoxicity, it should be considered that many of these parameters should be used with caution in patients with comorbidities (e.g., LV hypertrophy, obesity, and myocardial infarction) that can affect LV strain. Age and gender also should be taken into consideration when interpreting strain values [27, 28].
Nevertheless, the most important limitation is intervendor variability. Actually, there is now consistent normal value for all vendors. This should be considered in follow-up examinations [29].
4.1.7 Stress Echocardiography and Cardiotoxicity
Stress echocardiography is helpful in the evaluation of patients with suspected coronary heart disease who will receive regimens that may cause ischemia (fluorouracil, bevacizumab, sorafenib, and sunitinib).
Stress echocardiography has also been used to identify chemotherapy-induced subclinical cardiac dysfunction. Jardfeld documented a reduced ejection fraction at stress compared with rest in ten out of 23 patients who received anthracyclines at childhood due to acute lymphatic leukemia. These young adults were examined median 21 years after remission, whereas 12 healthy controls had no reduced LVEF [30].
Bountioukos evaluated whether repetitive systolic and diastolic cardiac function evaluated by low-dose stress echocardiography can predict anthracycline cardiotoxicity. In this study, the assessment of contractile reserve had no incremental value for the early detection of cardiotoxicity [10].
In another study, high-dose dobutamine stress echocardiography detected subclinical anthracycline-induced cardiotoxicity at lower cumulative doses.
In conclusion stress, echocardiography can detect ischemia whether due to a coronary artery disease as a bystander or induced by chemotherapy.
Stress echocardiography might allow the earlier identification of disease based on recognizing a reduced cardiac reserve, but the results remain unclear.
4.1.8 Conclusion
Echocardiography is regarded as the standard imaging modality to detect cardiotoxicity.
LVEF assessed by 2D echo might not be accurate enough to detect small changes in LV contractility.
Especially in the case of any border line cases, the best available method should be used.
Three-dimensional echocardiography (if available or feasible) or switching to another imaging modality like cardiac MRI can help to identify pathologies.
Contrast echocardiography should be used if a clear endocardial delineation of two continuous segments is not possible.
Strain imaging is a very promising technique that helps to detect subclinical dysfunction.
Global longitudinal strain is the most often used parameter.
4.2 Nuclear Magnetic Resonance
Cardiac magnetic resonance (CMR) measures ventricular volumes, mass, and function very accurately; it is reproducible and it is today regarded as the gold standard for these measurements. CMR provides also much information about the morphology and function of the tissues of the heart and important information about paracardiac structures. It shows tissue alterations like myocardial edema and fibrosis. Finally, it helps to identify cardiotoxicity at a very early stage.
Furthermore, CMR is a radiation-free method.
CMR is therefore a very valuable tool especially if a prior echo examination is non-conclusive or shows borderline results.
4.2.1 Introduction
Cardiac MRI is an increasingly available method due to the situation that more and more MRI scanners include the technical conditions to perform heart examinations.
With its unique ability to characterize myocardial tissue and identify both cardiac and vascular dysfunction, cardiac MRI (CMR) provides a comprehensive overview about potential pathologies at early stages and/or in follow-up examinations.
Early detection of these abnormalities is of particular importance to initiate a tailored treatment.
Images can be obtained in any plane and any orientation which enables to measure in anatomical-corrected imaging positions.
In comparison to echocardiography that struggles sometimes with poor acoustic windows, CMR provides images without limitations.
Thus, cardiac MRI might be preferred in difficult imaging conditions like obese patients, individuals with lung diseases, prior radiation treatment, or surgery.
A field of view (FOV) of up to 50 cm accomplishes a good general overview from the heart and its neighboring structures.
In contrast to nuclear imaging and CT, CMR does not require the ionizing radiation and thus is useful for follow-up examinations.
An important limitation of CMR might be the existence of a pacemaker. Although in more and more countries MRI conditional devices are implanted, the gross of patients still have devices that are not approved for MRI.
The rate of claustrophobic attacks decreased with the upcoming wide bore (70 cm) scanner types and allows imaging of larger dimensions.
4.2.2 Ventricular Function/Volumes and Mass
A major strength of CMR is the accurate and reproducible measurement of ventricular volumes, mass, and function. Today, CMR is commonly regarded as the reference standard for these measurements [31].
Based on a stack of contiguous 2D cine slices, a real 3D dataset is acquired without limitations of geometric assumptions regarding the shape of the left ventricular cavity.
In the case of normal cardiac dimensions without any wall motions abnormalities, 2D measurements do not differ substantially from a measurement acquired by a 3D dataset and allow a quick overview.
Usually, the two- and four-chamber view of the left ventricle is used for the biplane calculations very similar to echocardiography. In contrast to 2D echo, the “real” LV apex can be displayed and the foreshortening of the left ventricle can be avoided. Therefore, generally, volumes quantified by 2D echo are smaller (in terms of an underestimation) than MRI volumes. This has to be considered comparing these modalities against each other. It is more likely to compare LVEF of both techniques because the systemic error of calculation of foreshortened end-diastolic and end-systolic volumes in echo is compensated.
Generally, the 3D acquisition of these LV volumes and EF is highly recommended, especially when cardiac function becomes reduced, the left ventricle assumes an abnormal shape, and/or regional wall abnormalities exist.
Distinguishing relatively small changes in LVEF related to cardiotoxicity from those related to variance in the technique can be problematic.
Cardiac MRI exhibits the best inter-study coefficient of variability for assessment of LV volumes, function, and mass [32].
In a study from Grothues, the inter-study reproducibility for CMR versus 2D echocardiography was measured as the following:
The high accuracy and precision of CMR may allow identification of early and possibly subclinical cardiac injury and enables a better differentiation between still normal and incipient pathologic findings. Furthermore, CMR is very suitable for detection of discrete changes in follow-up examinations.
The routinely utilized cine sequences provide an excellent contrast between the cavity blood pool and myocardium. Exogenous contrast agent is not needed (Fig. 4.4).


Fig. 4.4
3D volumetry of the left (red) and right (yellow) ventricle
The excellent signal-to-noise ratio depicts endocardial and epicardial borders of the left and right ventricle inclusive of the trabeculations.
To be consistent in the measurements, some points should be regarded.
The papillary muscles should be excluded from the LV volume whereas they should be included with the LV mass.
Generally, retrospective-gated movie covers the whole RR cycle, and thus the real systole and diastole can be calculated correctly. A breath-hold time about 10–12 s is needed.
Using the retrospective gating in case of arrhythmias, real systole and diastole cannot be depicted correctly, and thereby particularly, the EF can be underestimated.
Specific sequences exist for irregular rhythms. The so-called real-time cine acquires many images a second and provides cine sequences in a cardiac cycle. With help of different acceleration techniques, the signal-to-noise ratio and the spatial resolution are very acceptable and can be used routinely.
Acceleration techniques can also be used to decrease the breath-hold time (e.g., from 12 to 2 s) or to increase the temporal resolution (e.g., from 40 ms to less than 10 ms).
Short breath-hold sequences are really helpful for patients who are in bad general condition. In future time, it is expected that cine sequences are acquired in free-breathing techniques.
Cine sequences with a temporal resolution less than 10 s provide additional information about the diastole and depict subtle changes that can also be used for strain imaging, for instance.
4.2.3 Strain Imaging
In echocardiography, strain imaging was able to detect preclinical changes in LV systolic function, before conventional changes in LV EF [34, 35].
Strain imaging by MRI is an evolving field of investigation even though not widely used.
A study of Drafts et al. showed early after exposure to low to moderate doses of anthracycline-based chemotherapeutic regimens the development of subclinical abnormalities of cardiac function. End-systolic volume and strain increased, whereas LVEF decreased within 6 months. Moreover, these deteriorations remained present after the discontinuation of anthracycline chemotherapy [36] (Fig. 4.5).
Fig. 4.5
Abnormal global longitudinal strain of a patient with cardiomyopathy. Especially the septal and inferior segments exhibit abnormal regional strain
4.2.4 T2 in Cardiotoxicity
Increased signal in the myocardium on T2-weighted (T2-w) images has been described in the presence of acute myocardial inflammation and injury, as in myocarditis and myocardial infarction or stress-induced cardiomyopathy [37–39].
Myocardial edema after an anthracycline therapy has been documented in a small study, but reliable data of bigger studies are still lacking [40].
In future time, further results are expected that illuminate the question whether myocardial edema is an indicator for early cardiotoxicity and has a prognostic impact.
Besides the often-used STIR sequences (short tau inversion recovery), T2-mapping sequences are of special interest, and T2 mapping is less dependent on heart rate and arrhythmias. In addition, the breath-hold time of the mapping sequence is by far shorter than that of a conventional fast spin echo sequence, which makes imaging easier for a heart failure patient.
STIR sequences are prone to artifacts from respiratory and cardiac motion and surface coil signal nonhomogeneities and subendocardial bright signal artifacts caused by stagnant blood (Fig. 4.6).
Fig. 4.6
STIR sequence: focal myocardial edema (bright areas) in the lateral wall (arrowhead)
Thavendiranathan described in a poster presentation an increase of T2 values in T2-mapping sequences in breast cancer patients receiving sequential therapy with anthracyclines and trastuzumab.
They assumed that myocardial edema may be a feature of cardiotoxicity that results from treatment with sequential anthracyclines and trastuzumab [41] (Fig. 4.7).
Fig. 4.7
T2 mapping: higher values indicating a myocardial edema
Whether quantitative assessment of myocardial edema early during therapy can predict subsequent development of cardiotoxicity remains to be determined.
4.2.5 Late Gadolinium Enhancement
Late gadolinium enhancement (LGE) imaging allows detection of focal myocardial fibrosis after administration of Gd-based contrast material.
The mechanism of enhancement is not completely understood; however, the enlargement of the interstitial space and different wash-in and wash-out kinetics of fibrotic areas within the myocardium compared to normal myocardium seem to be most important factors.
Eight to fifteen minutes after application of gadolinium, myocardial fibrosis can be detected well below 1 g of mass [42, 43].
Besides the detection of myocardial fibrosis, late enhancement has a big importance in the differential diagnosis of their etiology.
The pattern and location enable the differentiation of ischemic from nonischemic causes [44].
Roughly a subendocardial distribution mostly points to ischemic causes, whereas an intramural or subepicardial distribution indicates a nonischemic cause (e.g., myocarditis, amyloidosis, autoimmune diseases).
Nonischemic diseases usually show a specific late enhancement pattern and thus can be classified.
A reliable discrimination sometimes is challenging due to an overlap of fibrosis in some diseases.
In addition, existence of late enhancement has an important prognostic value in many cardiovascular diseases.
The pattern of LGE described in anthracycline-treated patients includes subepicardial, intramural, and LGE at right ventricular insertion points [45–47] (Fig. 4.8).


Fig. 4.8
Though the potential great value of detection of myocardial damage, the incidence and the prognostic relevance of LGE is marginally investigated.
In the current studies, the incidence of LGE in patients treated with anthracyclines and trastuzumab showed a very wide range between 8 % [46] and 100 % [48–50] in the context of established cardiomyopathy.
Whether late enhancement has prognostic relevance is still part of further investigations.
4.2.6 T1 Mapping
Pathological myocardial fibrosis due to cancer therapy tends to be diffuse [51].
Myocyte loss and interstitial edema induce an expansion of the myocardial extracellular space and thus the volume of distribution of contrast agent.
This is fundamental change associated with early pathological remodeling in the course of cardiotoxicity [52].
Late enhancement imaging is excellent for the detection of focal myocardial fibrosis but may miss subtle diffuse myocardial fibrosis.
The T1 relaxation time can be measured pre- and post-contrast. The extracellular volume can be calculated out of it [56].
In patients with cardiomyopathy, the myocardial ECV assessment has prognostic value beyond assessment of LV EF.
Rats with histological evidence of chronic cardiotoxicity showed higher native T1 values compared with controls without an increase in myocardial water content or CMR-based T2 values [57].
Myocardial T1 and ECV were found to be early tissue markers of ventricular remodeling that may represent diffuse fibrosis. ECV has been correlated with anthracycline dose, functional capacity, LV dysfunction, and markers of adverse ventricular remodeling in pediatric [58] and adult patients well after completion of anthracycline-based chemotherapy [59].
Tham and his colleagues showed that subjects with increased T1 values and ECV had received higher cumulative doses, had reduced exercise capacity, and had showed myocardial wall thinning.
Quantitative myocardial T1 mappings, including the derived ECV, are thus potential biomarkers of chemotherapy cardiotoxicity that may have the ability to detect signs of remodeling or tissue damage earlier than conventional functional metrics.
Similarly, a study by Neilan shows an increased ECV in adults with previous anthracycline exposure [59].
In another study about occult cardiotoxicity in childhood cancer survivors exposed to anthracycline therapy, mean T1 values of the myocardium were significantly measured lower than that of control subjects at 20 min [60].
4.2.7 Cardiac and Pericardial Metastases
By comparison, metastases to the heart and pericardium are 100–1,000 times more frequent than primary tumors [33].
In autopsies at which a malignant neoplasm was diagnosed, cardiac metastases were found in 9.7–10.7 % of cases [34].
Cardiac involvement may arise through direct invasion, lymphatic or hematogenous spread, or transvenous extension.
CMR allows full coverage of the entire heart and provides further information about the tissue composition through the use of cine imaging, T1- and T2-weighted sequences, contrast perfusion, and late gadolinium enhancement.
Thus, it facilitates the differentiation between noninvasive and invasive growing and identifies a confine between malignant and benign tumors like lipomas, cyst, or thrombus (Fig. 4.9).
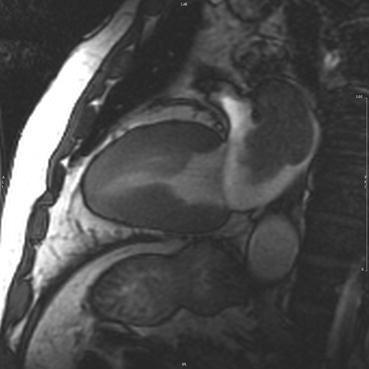
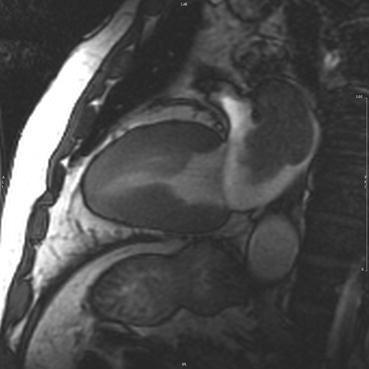
Fig. 4.9
Pulmonary metastasis of renal cancer with invasive growth into the left atrium
4.2.8 Conclusion
4.2.8.1 CMR: One-Stop Strategy
CMR provides many information about the morphology, function tissue of the heart, and important information about paracardiac structures.
4.2.8.2 CMR Is a Radiation-Free Method
CMR measures ventricular volumes, mass, and function very accurately; it has a high reproducibility and it is today regarded as the reference standard for these measurements.
CMR is therefore a very valuable tool especially if a prior echo examination is non-conclusive or shows borderline results.
CMR permits much information about tissue alterations like myocardial edema and fibrosis. It is assumed that this helps to identify cardiotoxicity at a very early stage.
4.3 Radionuclide Imaging
Radionuclide imaging evaluates functional and structural parameters of the heart and might be used to evaluate cardiotoxicity. Multiple-gated cardiac blood pool imaging (MUGA) is a widely accepted modality to evaluate LVEF due to its high reproducibility and low interobserver and intraindividual variability. Instead to quantify cardiac blood pool, SPECT detects myocardial contours and is less accurate than MUGA, but it can be regarded as an alternative technique for LV measurement. Generally, nuclear imaging offers with different approaches the possibility to detect cardiotoxic alterations at early stages. 123I-MIBG scintigraphy has been shown to be an excellent early predictor of cancer treatment-induced cardiac dysfunction.
Radiation exposition is the main concern for the use of radionuclide imaging, and in pediatric populations, these imaging techniques are not generally used.
4.3.1 Introduction
Evaluation of cardiotoxicity takes an important part in radionuclide imaging. Radionuclide imaging can assess functional parameters and structural parameters of the heart and might be sensitive to evaluate cardiotoxicity. Besides different techniques in evaluating cardiac function, a range of other targeted tracers are used. Assessment of systolic cardiac function is a common method of monitoring cardiac function during cancer treatment. Multiple-gated cardiac blood pool imaging is the most broadly used technique. SPECT detects myocardial contours (instead of quantifying cardiac blood pool) and is less accurate but can be regarded as an alternative technique for LV measurement.
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


