Chapter 14
Cardiac Catheterization, Angiography, IVUS, and FFR
1. What are generally accepted indications for cardiac catheterization?
 Class III-IV angina despite medical treatment or intolerance of medical therapy
Class III-IV angina despite medical treatment or intolerance of medical therapy
 High-risk results on noninvasive stress testing
High-risk results on noninvasive stress testing
 Sustained (more than 30 seconds) monomorphic ventricular tachycardia or nonsustained (less than 30 seconds) polymorphic ventricular tachycardia
Sustained (more than 30 seconds) monomorphic ventricular tachycardia or nonsustained (less than 30 seconds) polymorphic ventricular tachycardia
 Sudden cardiac death survivors
Sudden cardiac death survivors
 Most patients with non–ST-segment elevation acute coronary syndrome (NSTE-ACS) who have high-risk features and no contraindications to early cardiac catheterization and revascularization
Most patients with non–ST-segment elevation acute coronary syndrome (NSTE-ACS) who have high-risk features and no contraindications to early cardiac catheterization and revascularization
 Systolic dysfunction and stress testing results suggesting multivessel disease and potential benefit from revascularization
Systolic dysfunction and stress testing results suggesting multivessel disease and potential benefit from revascularization
 Recurrent typical angina within 9 months of percutaneous coronary revascularization
Recurrent typical angina within 9 months of percutaneous coronary revascularization
 For assessment of valvular dysfunction or other hemodynamic assessment when the results of echocardiography are indeterminate
For assessment of valvular dysfunction or other hemodynamic assessment when the results of echocardiography are indeterminate
 As part of primary percutaneous coronary intervention (PCI) for ST-segment elevation myocardial infarction (STEMI)
As part of primary percutaneous coronary intervention (PCI) for ST-segment elevation myocardial infarction (STEMI)
 Patients post-STEMI (with or without thrombolytic therapy) with high-risk features, depressed ejection fraction, or high-risk results on subsequent stress testing
Patients post-STEMI (with or without thrombolytic therapy) with high-risk features, depressed ejection fraction, or high-risk results on subsequent stress testing
 Within 36 hours of STEMI in appropriate patients who develop cardiogenic shock
Within 36 hours of STEMI in appropriate patients who develop cardiogenic shock
 In select patients who are to undergo valve replacement or repair
In select patients who are to undergo valve replacement or repair
 In assessment and management of patients with congenital heart disease and cardiac transplant recipients
In assessment and management of patients with congenital heart disease and cardiac transplant recipients
2. What are the risks of cardiac catheterization?
The risks of cardiac catheterization will depend to some extent on the individual patient. For “all comers,” the risk of death is approximately 1 in 1000, with the risk of myocardial infarction or stroke rarer than 1 in 1000. The risk of any major complication in “all comers” is less than 1%. These risks are summarized in Table 14-1.
TABLE 14-1
RISKS OF CARDIAC CATHETERIZATION AND CORONARY ANGIOGRAPHY

Reproduced from David CJ, Bonow RO: Cardiac Catheterization. In Libby P, Bonow RO, Mann DL, Zipes DP, editors: Braunwald’s heart disease: a textbook of cardiovascular medicine, ed 8, Philadelphia, 2007, Saunders, p 461.
3. How are coronary lesions assessed?
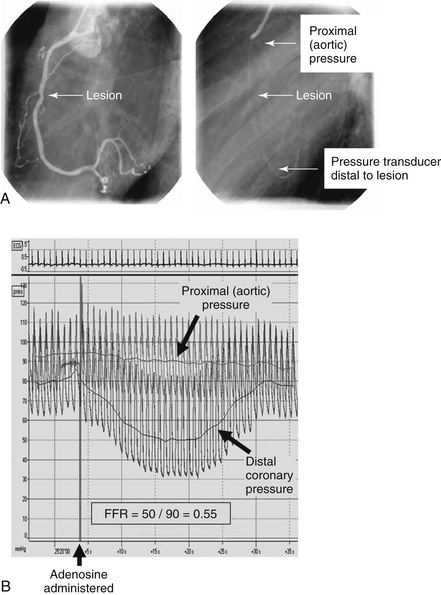
Coronary lesions are most commonly assessed in day-to-day practice based on subjective visual impression (Fig. 14-1). Lesions are subjectively given a percent stenosis, ideally based on ocular assessment of at least two orthogonal images of the lesion. Studies have shown interobserver and intraobserver variability in judging coronary stenosis from as little as 7% to as much as 50%. Quantitative coronary angiography (QCA) more objectively assesses the lesion severity than does “ocular judgment,” but is not commonly used in day-to-day practice. QCA generally grades lesions as less severe than does subjective ocular judgment of a lesion’s severity. Intravascular ultrasound (IVUS) can more accurately assess the total plaque burden and severity of a lesion than can ocular judgment or QCA. Fractional flow reserve (FFR) is increasingly being used to measure the severity of a lesion from a physiologic standpoint (see later).
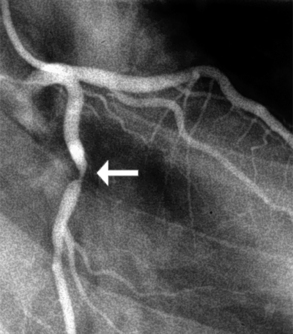
Figure 14-1 Coronary angiography of the left coronary artery demonstrates an approximate 90% lesion (arrow) in the left coronary artery.
4. What is considered a “significant” stenosis?
The classification of significant stenosis depends on the clinical context and what one considers “significant.” Coronary flow reserve (the increase in coronary blood flow in response to agents that lead to microvascular dilation) begins to decrease when a coronary artery stenosis is 50% or more of the luminal diameter. However, basal coronary flow does not begin to decrease until the lesion is 80% to 90% of the luminal diameter.
5. What is fractional flow reserve (FFR)?
Physiologic assessment of blood flow through a stenotic lesion can be safely and reliably performed in the catheterization laboratory using a coronary wire with a pressure sensor at its tip. The wire is advanced across the lesion of interest, and the ratio of distal coronary pressure to proximal aortic pressure is assessed after maximal hyperemia is achieved (Fig 14-2). This ratio is called FFR. Normal values are close to 1, and a ratio less than 0.75 to 0.80 is taken as indicating a “physiologically significant stenosis.” Adenosine is typically used as a pharmacologic agent to achieve maximal hyperemia.