Increased prevalence of cardiac arrhythmias has been reported in patients with severe obstructive sleep apnea (OSA), but this may not be generalizable to patients from the general population with a milder form of the condition. The aim of this study was to assess the association between cardiac arrhythmias and OSA of mainly mild and moderate severity. In total, 486 subjects (mean age 49 years, 55% men) recruited from a population-based study in Norway underwent polysomnography for OSA assessment and Holter recordings for arrhythmia assessment. Of these, 271 patients were diagnosed with OSA (apnea–hypopnea index [AHI] ≥5, median AHI 16.8, quartiles 1 to 3 8.9 to 32.6). Mean nadir oxygen saturations were 82% and 89% in patients with and without OSA, respectively. Ventricular premature complexes (≥5/hour) were more prevalent in subjects with OSA compared to subjects without OSA (median AHI 1.4, quartiles 1 to 3 0.5 to 3.0) during the night (12.2% vs 4.7%, p = 0.005) and day (14% vs 5.1%, p = 0.002). In multivariate analysis after adjusting for relevant confounders, AHI was independently associated with an increased prevalence of ventricular premature complexes at night (odds ratio per 1-U increase of log-transformed AHI 1.5, 95% confidence interval 1.1 to 2.0, p = 0.008) and during the day (odds ratio 1.37, 95% confidence interval 1.0 to 1.8, p = 0.035). In conclusion, the prevalence of ventricular premature complexes is increased in middle-aged patients with mainly mild or moderate OSA, suggesting an association between OSA and ventricular arrhythmias even in mild OSA.
The association between obstructive sleep apnea (OSA) and cardiac arrhythmias is supported by observations from several sleep clinic-based studies, in which up to 60% of patients with severe OSA were found to develop cardiac arrhythmias. Furthermore, the Outcomes of Sleep Disorders in Older Men Study and the Sleep Heart Health Study have recently complemented these results by showing that elderly subjects and subjects with severe OSA from the general population also have a high prevalence of cardiac arrhythmias. However, there is limited information on the prevalence of cardiac arrhythmias during the night and day in community-dwelling middle-aged subjects with predominantly mild and moderate unrecognized OSA. Accordingly, we aimed to assess the prevalence of arrhythmias in this population and assess the association between arrhythmias and indexes of OSA severity, i.e., apnea–hypopnea index (AHI) and nadir oxygen saturation (SaO 2 ).
Methods
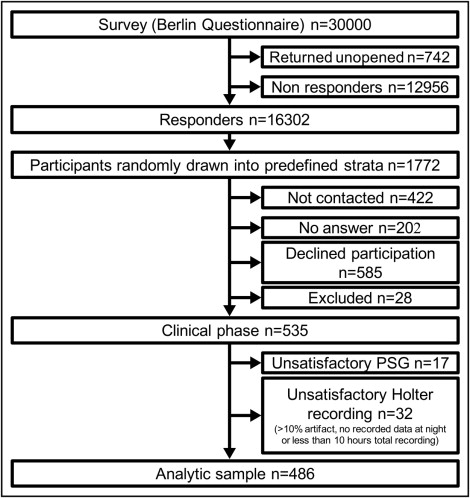
This is a substudy of the Akershus Sleep Apnea Project (ASAP). The recruitment protocol and main inclusion and exclusion criteria have been previously reported. In brief, the Berlin Questionnaire was mailed to 30,000 randomly selected patients 30 to 65 years of age ( Figure 1 ) . The Berlin Questionnaire includes questions on daytime sleepiness, snoring, and obesity/hypertension and is used to stratify patients for risk of OSA. Of the 16,302 responders, 1,772 subjects were further categorized in predefined strata based on the Berlin Questionnaire and randomly drawn for participation in the clinical phase of the ASAP. In all strata there was a balanced age and gender distribution, whereas subjects with previous ear surgery for recurrent otitis media, cardiovascular disease, and diabetes mellitus were oversampled. Fifty percent to 70% of subjects in each stratum were considered at high risk of having OSA.
All subjects participating in the clinical phase of the ASAP were interviewed and subjected to a standardized clinical examination. Cardiovascular disease was defined as coronary artery disease (angina, previous myocardial infarction, previous coronary artery intervention), heart failure, or history of stroke. Data on diabetes mellitus (fasting blood glucose ≥7 mmol/L or antidiabetic medication) and hypertension (systolic blood pressure ≥140 mm Hg, diastolic blood pressure ≥90 mm Hg, or on antihypertensive medication) were also recorded. Blood pressure (Dinamap, ProCare 400, GE Healthcare, Milwaukee, Wisconsin) was measured 3 times with the patient sitting down and the mean of the last 2 recordings was used for analyses. Body mass index was measured by dividing weight (kilograms) by height (meters) squared. Waist–hip ratio was measured by dividing waist circumference (centimeters) by hip circumference (centimeters). Fasting blood samples were drawn in the morning after the sleep recordings and lipids were measured by standard laboratory methods.
Participants who agreed to participate in the clinical phase of the ASAP completed a full in-hospital polysomnographic procedure. Number and duration of apneas and hypopneas were recorded with Somnologica 3.2 (Flaga-Medcare, Buffalo, New York). AHI was calculated by 2 United States board-certified polysomnographic technicians blinded to Berlin Questionnaire scores and results of Holter recordings. OSA was defined as an AHI ≥5. SaO 2 was recorded by finger plethysmography (Nonin, Plymouth, Minnesota). The nadir SaO 2 was recorded after all results had been manually checked for technical artefacts.
A 5-channel ambulatory electrocardiograph (MedilogAR12, Oxford Instruments Medical, Ltd., Surrey, United Kingdom) was fitted to all subjects on arrival during the midday/afternoon before polysomnographic recordings. The Holter recorder was retained throughout the examinations, permitting continuous assessment of heart rate and arrhythmias. Electrocardiograph recordings were automatically interpreted by a software engine (Medilog Darwin, ScanMed Medical, Gloucestershire, United Kingdom) and subsequently manually reviewed by 2 researchers (S.K.N., G.E.) according to predefined criteria. Cardiac arrhythmias were divided into supraventricular arrhythmias, ventricular arrhythmias, and conduction delay arrhythmias ( Table 1 ). Among ventricular arrhythmias, bigeminy, trigeminy, and nonsustained ventricular tachycardia were also grouped together as complex ventricular ectopies. All arrhythmias were coded as dichotomous outcomes (present or absent) according to acknowledged cutoffs applied in previous community-based studies. Ventricular premature complexes were divided by a cutoff of 5 events/hour (pathologic) and ≥30 events/hour (severe). Interpreters were blinded to Berlin Questionnaire scores and polysomnographic results and scoring was performed separately. The intraclass correlation coefficient between the 2 reviewers was 0.99 to 1 (n = 25) for arrhythmic events measured by Holter recording. For uncertain classification of an arrhythmia, a third reviewer (T.O.) was consulted.
| Supraventricular arrhythmias |
| 1. Atrial premature complexes |
| 2. Supraventricular tachycardia |
| 3. Chronic atrial fibrillation |
| 4. Paroxysmal atrial fibrillation |
| Ventricular arrhythmias |
| 1. Ventricular premature complexes |
| 2. Bigeminy |
| 3. Trigeminy |
| 4. Nonsustained ventricular tachycardia; minimum 3 consecutive ventricular beats ≥110 beats/min |
| 5. Complex ventricular ectopy: bigeminy, trigeminy, or nonsustained ventricular tachycardia |
| Conduction delay arrhythmias |
| 1. Sinus pause >2 seconds |
| 2. Atrioventricular block |
Categorical data are presented as absolute numbers and percentages and continuous data as mean ± SEM (normal distribution) or median and quartiles 1 to 3 (nonparametric data). Continuous data were assessed by histograms and normal Q–Q plots to check for normal distribution. Differences between groups, including prevalence of arrhythmias were assessed by chi-square test or Fisher’s exact test and by Student’s t test or Mann–Whitney U test as appropriate. Correlations were calculated by Spearman rank correlation. For arrhythmias with divergent prevalence in the OSA versus non-OSA group, the association between AHI and arrhythmias was assessed by univariate and multivariate logistic regression analyses with results reported as odds ratio (OR) per 1-U increase of logarithmically transformed AHI and 95% confidence interval (CI). Covariates such as age, gender, body mass index, diabetes mellitus, hypertension, total cholesterol/high-density lipoprotein cholesterol ratio, and history of cardiovascular disease were entered into multivariate models if they were significant in univariate models. In a second set of logistic regression analyses, AHI was substituted by nadir SaO 2 as the variable assessing OSA severity. A p value <0.05 was considered statistically significant for all analyses. Analyses were performed with SPSS 16.0 or 18.0 for Windows (SPSS, Inc., Chicago, Illinois).
The main protocol and all subprotocols of the ASAP were approved by the regional ethics committee. The study was conducted in accordance with the Declaration of Helsinki and all participants signed an informed consent before study commencement.
Results
In total, 535 participants were included in the clinical phase of the study ( Figure 1 ). Of these, 49 subjects were excluded because of unsatisfactory polysomnographic recordings or technical problems with Holter registration. Baseline characteristics of subjects with and without OSA are presented in Table 2 . In general, subjects diagnosed with OSA were older, more obese, and more likely to be men compared to subjects without OSA. Subjects with OSA also exhibited a higher prevalence of co-morbidities including hypertension, diabetes mellitus, and previous myocardial infarction, and the difference in co-morbidities was also reflected in medication use.
| Variable | OSA | p Value | |
|---|---|---|---|
| No(n = 215) | Yes(n = 271) | ||
| Age (years) | 44.1 ± 0.8 | 51.9 ± 0.6 | <0.001 |
| Women | 57% | 36% | <0.001 |
| Body mass index (kg/m 2 ) | 27 ± 0.3 | 30 ± 0.3 | <0.001 |
| Waist–hip ratio | 0.9 ± 0.01 | 1.0 ± 0.01 | <0.001 |
| Mean heart rate (beats/min) | 70.8 ± 0.6 | 72.1 ± 0.6 | 0.2 |
| Current smokers | 29% | 26% | 0.4 |
| Hypertension | 41% | 67% | <0.001 |
| Diabetes mellitus | 7% | 17% | 0.001 |
| Stroke | 2% | 4% | 0.4 |
| Heart failure | 0% | 0% | — |
| Angina pectoris | 0.5% | 3% | 0.05 |
| Myocardial infarction | 4% | 13% | <0.001 |
| Coronary artery bypass grafting | 0.5% | 1.5% | 0.4 |
| Percutaneous coronary intervention | 2% | 5% | 0.09 |
| Cardiovascular disease ⁎ | 6% | 18% | <0.001 |
| Triglycerides | |||
| mmol/L | 1.2 (0.9–1.7) | 1.5 (1.1–2) | <0.001 |
| mg/dl | 46.4 (34.8–65.7) | 58 (42.5–77.3) | |
| Total cholesterol | |||
| mmol/L | 5.4 (4.8–6.2) | 5.5 (4.8–6.2) | 0.3 |
| mg/dl | 208.8 (185.6–239.8) | 212.7 (185.6–239.8) | |
| High-density lipoprotein cholesterol | |||
| mmol/L | 1.3 (1.1–1.6) | 1.3 (1.0–1.5) | 0.009 |
| mg/dl | 50.3 (42.4–61.9) | 50.3 (38.7–58) | |
| Platelet aggregation inhibitors | 8.4% | 22.1% | <0.001 |
| Diuretics | 5.1% | 18.5% | <0.001 |
| β Blocker | 8.8% | 21.8% | <0.001 |
| Calcium channel blocker | 4.7% | 13.3% | 0.001 |
| Angiotensin II–converting enzyme inhibitor/angiotensin II receptor blocker | 12.6% | 29.2% | <0.001 |
| Statin | 11.2% | 26.6% | <0.001 |
| Apnea–hypopnea index (events/hour) | 1.4 (0.5–3.0) | 16.8 (8.9–32.6) | <0.001 |
| Nadir oxygen saturation | 89 ± 0.2 | 82 ± 0.4 | <0.001 |
⁎ Defined as coronary artery disease (angina, previous myocardial infarction, previous coronary artery intervention), heart failure, or history of stroke.
Of the 486 subjects included in the final analysis ( Figure 1 ), 271 subjects (56%) were diagnosed with OSA. Only 72 subjects (14.8%) were diagnosed with severe OSA as defined by AHI ≥30. AHI correlated with established risk factors for OSA such as age (r = 0.40), body mass index (r = 0.35), and waist–hip ratio (r = 0.48, p <0.001 for all comparisons). Subjects with OSA had lower SaO 2 during sleep compared to subjects without OSA as evaluated by the recorded nadir SaO 2 .
Median Holter recording time was 18.5 hours (quartiles 1 to 3 17 to 20). A larger proportion of subjects with OSA had ventricular premature complexes at night and during the day compared to subjects without OSA ( Table 3 ). This was also evident when examining the proportion of subjects exhibiting severe ventricular premature complex activity (≥30/hour) at night and during the day. There was a higher prevalence of complex ventricular ectopies during daytime recordings in subjects with OSA. For conduction delay arrhythmias and supraventricular arrhythmias including atrial fibrillation, we found no differences between the OSA and non-OSA groups ( Table 3 ).
| Variable | Daytime OSA | Night-Time OSA | ||||
|---|---|---|---|---|---|---|
| No (n = 215) | Yes (n = 271) | p Value | No (n = 215) | Yes (n = 271) | p Value | |
| Ventricular premature complexes ≥5/hour | 5.1% | 14.0% | 0.001 | 4.7% | 12.2% | 0.004 |
| Ventricular premature complexes ≥30/hour | 1.9% | 5.9% | 0.036 | 1.4% | 5.2% | 0.026 |
| Nonsustained ventricular tachycardia | 1.9% | 2.6% | 0.76 | 0.5% | 0.4% | 1.0 |
| Complex ventricular ectopy ⁎ | 4.7% | 10.7% | 0.015 | 1.9% | 5.5% | 0.057 |
| Atrial premature complexes ≥5/hour | 48.4% | 41.7% | 0.14 | 49.8% | 49.4% | 0.94 |
| Atrial fibrillation/paroxysmal atrial fibrillation | 0% | 1.5% | 0.13 | 0% | 1.5% | 0.13 |
| Pause >2 seconds | 4.2% | 5.9% | 0.34 | 4.7% | 7.7% | 0.17 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


