Cardiac Anatomy and Physiology
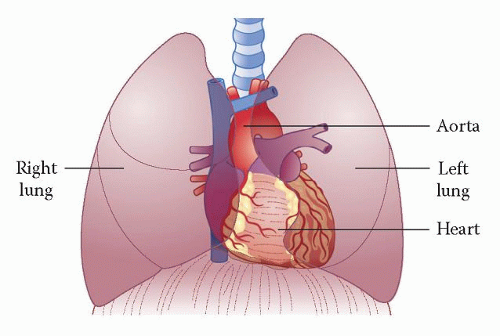
The heart lies within the thorax, to the left of the midline, protected by the rib cage and lying in close proximity to the lungs and, underneath, the diaphragm (Fig. 2.1). The ribs and lungs can provide a challenge for the sonographer trying to obtain clear images of the heart, as ultrasound does not penetrate bone or aerated lung well.
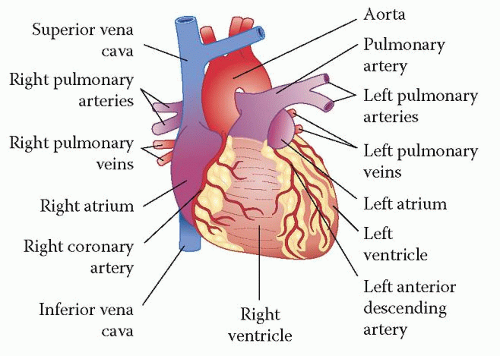
The heart consists of four main chambers (left and right atria, and left and right ventricles) and four valves (aortic, mitral, pulmonary and tricuspid). Venous blood returns to the right atrium (RA) via the superior and inferior vena cavae, and leaves the right ventricle (RV) for the lungs via the pulmonary artery. Oxygenated blood from the lungs returns to the left atrium (LA) via the four pulmonary veins, and leaves the left ventricle (LV) via the aorta (Fig. 2.2).
CARDIAC CHAMBERS AND VALVES
The aortic valve
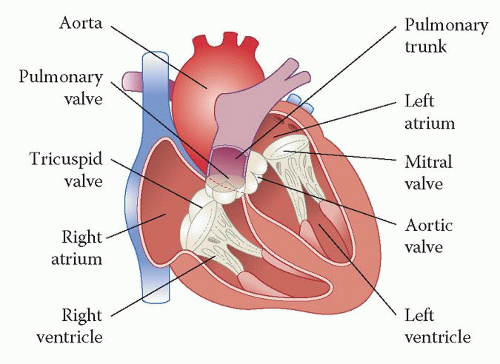
The aortic valve lies between the left ventricular outflow tract (LVOT) and aortic root (Fig. 2.3) and has three cusps, which open widely during systole. In diastole, the valve closes and, in the parasternal short axis view (aortic valve level), has a Y-shaped appearance (sometimes referred to as resembling a ‘Mercedes-Benz badge’; Fig. 6.5).
Upstream of the aortic valve are the sinuses of Valsalva, an expanded region of the aortic root, from which the coronary arteries originate. Each of the sinuses and aortic valve cusps is named according to its relationship to these coronary arteries: hence the right coronary cusp lies adjacent to the sinus giving rise to the right coronary artery (RCA), and the left coronary cusp to the sinus giving rise to the left coronary artery (LCA). The third sinus does not have a coronary artery, and the adjacent cusp is named the non-coronary cusp.
Where the valve cusps attach to the aortic root is often termed the aortic valve annulus, although the annulus is not a discrete structure (unlike the mitral valve annulus). The point where adjacent cusps meet is called the commissure. Each cusp has a small nodule at its centre, called the nodule of Arantius, which is more prominent in older patients. The ventricular surface of a cusp sometimes carries small mobile filaments, called Lambl’s excrescences, arising from the edge of the cusp. Lambl’s excrescences are of no clinical significance, but should not be mistaken for vegetations (Chapter 23) or papillary fibroelastoma (Chapter 27).
The left ventricle
The normal LV is an approximately symmetrical structure, which is cylindrical at its base (the mitral annulus) and tapers towards its apex. It is the main pumping
chamber of the heart and its wall is thicker (and myocardial mass greater), although less trabeculated, than that of the RV. The LV myocardium is conventionally subdivided into 16 or 17 segments, the function of each of which should be assessed individually (Chapter 16).
chamber of the heart and its wall is thicker (and myocardial mass greater), although less trabeculated, than that of the RV. The LV myocardium is conventionally subdivided into 16 or 17 segments, the function of each of which should be assessed individually (Chapter 16).
The mitral valve
The mitral valve lies between the left atrium and ventricle and has two leaflets that open during diastole and close in systole, to prevent regurgitation of blood from
the LV back into the LA. The mitral valve needs to be thought of as more than just two leaflets, however, because the mitral annulus, papillary muscles and chordae tendineae are all essential to the valve’s structure and function (Fig. 2.4).
the LV back into the LA. The mitral valve needs to be thought of as more than just two leaflets, however, because the mitral annulus, papillary muscles and chordae tendineae are all essential to the valve’s structure and function (Fig. 2.4).
The mitral leaflets are termed anterior and posterior and attach around their base to the fibrous mitral annulus, an elliptical ring separating the LA and LV. The anterior mitral leaflet is longer (from base to tip) than the posterior leaflet, but the length of its attachment to the annulus is shorter and so the surface area of both leaflets is about equal. Each leaflet is divided into three segments, or scallops, which are named A1, A2 and A3 (anterior leaflet) and P1, P2 and P3 (posterior leaflet), with the numbering running from the anterolateral commissure (A1/P1) to the posteromedial commissure (A3/P3) (Fig. 20.2).
There are two papillary muscles, named anterolateral and posteromedial (after the location of their attachment to the LV), and which are attached to the mitral leaflets via the chordae tendineae. Although there are two leaflets and two papillary muscles, each papillary muscle supplies chordae to both leaflets – it is not a 1:1 relationship. Chordae from the medial aspects of both leaflets attach to the posteromedial papillary muscle and from the lateral aspects to the anterolateral papillary muscle.
The chordae keep the mitral leaflets under tension during systole, preventing prolapse of the leaflets back into the LA. They are categorized into three groups:
first order or marginal chordae, which attach to the free edges of the mitral leaflets
second order or strut chordae, which attach to the ventricular surface of the leaflets (away from the free edges)
third order or basal chordae, which run directly from the ventricular wall (rather than the papillary muscles) to the ventricular surface of the posterior leaflet, usually near the annulus.
The mitral leaflets are normally thin and open widely during diastole, with the anterior leaflet almost touching the IVS. As the leaflets close (coapt) they overlap at their tips by several millimetres (apposition). A reduced degree of apposition results in poor coaptation and can cause mitral regurgitation.
The left atrium