Cardiac Anatomy
The heart is a muscular organ, pyramidal in shape, consisting of two parallel-valved pumps, located within the middle mediastinum, two-thirds to the left of the centerline. The base of the heart is oriented superiorly, whereas the apex points leftward, anteriorly, and slightly inferiorly. The cardiac apex is located at the fifth intercostal space near the midclavicular line. The heart is enclosed by the fibrous pericardium, which is bordered by the diaphragm inferiorly; the sternum and ribs anteriorly; the pleurae laterally; and the esophagus, descending aorta, and vertebrae posteriorly.
The average adult heart measures 12 cm from base to apex, 8 to 9 cm in width, and 6 cm in depth, approximating the size of a clenched fist. The heart weighs approximately 325 ± 75 g in men and 275 ± 75 g in women, accounting for 0.45% of body weight in males and 0.40% in females.
Viewed from the front, visible structures include the superior and the inferior vena cavae draining into the right atrium, the right ventricle (the most anterior chamber of the heart), the main pulmonary artery that courses superiorly and posteriorly before bifurcating, the left atrial appendage, a small portion of the left ventricle visible to the left of the left anterior descending coronary artery, and the ascending aorta (Fig. 3.1). The right heart forms the largest part of the anterior surface, whereas the left heart is largely posterior. The epicardial surface of the heart usually is covered with fat, proportional to age and the amount of body fat. Beneath the epicardial fat, the interventricular grooves separate the right and left ventricles and contain arteries, veins, nerves, and lymphatics. The atrioventricular (AV) grooves, which separate the atria from the ventricles, are located at the base of the heart. The interatrial grooves mark the borders between the atria. Posteriorly, the crux (“cross”) is the intersection of the AV, interatrial, and interventricular grooves. The acute cardiac margin is the junction of the inferior and anterior walls of the right ventricle. The obtuse margin is the rounded lateral wall of the left ventricle.
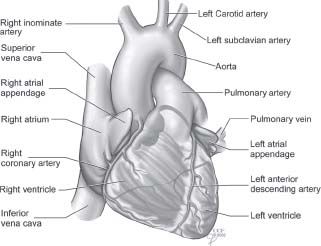
FIGURE 3.1 Frontal view of the heart and great vessels.
The heart is composed of four chambers. The right and the left atria are weakly contractile reservoirs that receive blood from the body and the lungs. They are positioned above the ventricles and are separated by the AV (tricuspid and mitral) valves. The right and left ventricles are muscular pumping chambers separated from each other by the interventricular septum. The ventricles eject blood through the semilunar (pulmonic and aortic) valves to the pulmonary artery and aorta, respectively.
The shape of the heart and the position of the valves are maintained by an internal fibrous skeleton. The cardiac skeleton consists of four valve annuli (or rings), the membranous septum, and the right and left fibrous trigones. The right fibrous trigone, also known as the central fibrous body, is located between the aortic, mitral, and tricuspid valves. It houses the His bundle and is the strongest component of the cardiac skeleton.
THE PERICARDIUM
The pericardium is a fibrous sac surrounding the heart and great vessels and containing 10 to 50 mL of pericardial fluid (Fig. 3.2). It maintains the position of the heart within the mediastinum, lubricates the cardiac surfaces, and provides a barrier against infection. Inferiorly, the pericardium is anchored to the central tendon of the diaphragm. Anteriorly, it is attached by ligamentous connections to the posterior sternum. Superiorly, the pericardium extends to the level of the second intercostal space, and laterally it is attached to the pleurae. The pericardium encloses the heart, portions of the vena cavae, most of the ascending aorta, the main pulmonary artery, and the four pulmonary veins. The pericardium consists of two layers. The inelastic fibrous pericardium is the outermost layer. The serous pericardium forms a thin mesothelial layer on the cardiac surface (the visceral pericardium or the epicardium) and lines the inferior surface of the fibrous pericardium (the parietal layer). The visceral pericardium covers the heart and contains the coronary arteries and veins, autonomic nerves, lymphatics, and fat. Posteriorly, the pericardium folds upon itself to create several distinct sinuses. The oblique sinus is a pericardial reflection along the vena cavae and the pulmonary veins. The transverse sinus is a pericardial reflection located between the aorta, pulmonary artery, and atria. The ligament of Marshall is a pericardial fold containing the remnant of the embryonic left superior vena cava.
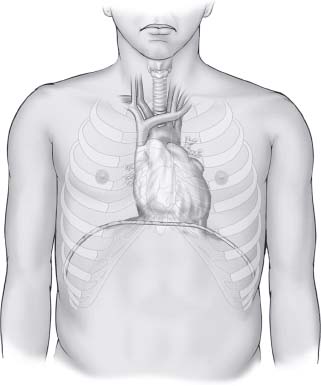
FIGURE 3.2 Frontal view of the pericardium.
CARDIAC CHAMBERS
Right Atrium
The right atrium is a low-pressure capacitance chamber that receives blood from the superior vena cava, inferior vena cava, and coronary sinus (Fig. 3.3). The right atrial volume is approximately 75 to 80 mL, and its free-wall thickness is 1 to 3 mm. The superior vena cava enters the superior aspect of the right atrium and directs its blood flow toward the tricuspid valve. The inferior vena cava returns blood from the lower body, and its eustachian valve directs blood flow toward the foramen ovale or the fossa ovalis. The coronary sinus returns most of the blood from the heart itself through an orifice partially guarded by the thebesian valve (valve of the coronary sinus). When the eustachian or thebesian valves are large and fenestrated, it is described as a Chiari net. Thebesian veins drain cardiac blood into the right atrium via multiple small orifices. The fossa ovalis, representing a closed foramen ovale, forms a 1.5- to 2.0-cm depression on the interatrial septum. A patent foramen ovale is found in up to one-third of adults. The crista terminalis is a C-shaped muscular ridge on the right atrial free wall that separates the smooth posterior portion of the right atrium from the muscular anterior portion. The pectinate (“comb”) muscles arise from the crista terminalis and course as bands anteriorly on the right atrial free wall. The right atrial appendage is a large triangular structure that overlies the right coronary artery and contains pectinate muscles. In the lower medial portion of the right atrium, Koch triangle overlies the AV node and the proximal His bundle. The tendon of Todaro is a fibrous band located between the valves of the inferior vena cava and the coronary sinus.
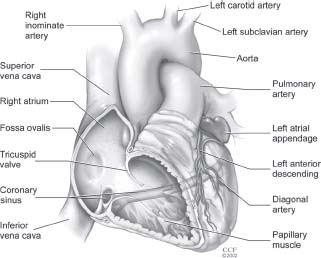
FIGURE 3.3 Frontal cutaway view of the right atrium and right ventricle.
Right Ventricle
The right ventricle is the most anterior chamber of the heart (Fig. 3.4). It is the smaller of the two ventricular chambers, separated from the left ventricle by the interventricular septum, which bulges into the right ventricle. It is triangular shaped when viewed from the right, and crescent shaped when viewed in cross section from the left. The right ventricular free wall is approximately 3 to 4 mm thick, or about one-third the thickness of the left ventricle. The right ventricle consists of an inlet portion, a trabeculated apical portion, and a smooth right ventricular outflow tract (infundibulum or conus portion). The walls of the right ventricle contain a latticework of muscle fibers called trabeculae carneae. The right ventricular apex is heavily trabeculated, more so than the left ventricle. The infundibulum (outflow tract or conus) portion of the right ventricle is smooth walled to the pulmonic valve. The right ventricle contains three papillary muscles, although the septal papillary muscle occasionally may be absent. Chordae tendineae (fibrous cords) extend upward from the papillary muscles and attach to the leaflet edges and to the ventricular side of the tricuspid valve. Chordae from one papillary muscle often attach to more than one tricuspid leaflet, and some chordae arise from the septum. The crista supraventricularis (supraventricular crest) separates the inflow and outflow portions of the right ventricle. It consists of a septal band on the ventricular septum and a parietal band on the right ventricular free wall. The moderator band is an intracavity muscular bridge that connects the distal septum with the right ventricular free wall at the anterior papillary muscle. Blood enters the right ventricle via the tricuspid valve, turns upward at a 45- to 60-degree angle, and passes through the pulmonic valve into the main pulmonary artery.
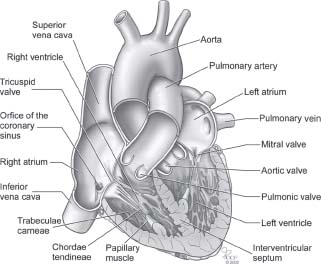
FIGURE 3.4 Coronal section of the heart and great vessels.
Left Atrium
The left atrium is the left upper posterior chamber of the heart (Fig. 3.5). It is cuboidal shaped, smaller than the right atrium (volume, 55 to 65 mL), but with thicker walls (3 mm) and higher pressure. It receives oxygenated blood from the lungs via four pulmonary veins (two from each lung). Unlike the right atrium, the left atrium has smooth interior walls and does not have bands of pectinate muscles except in the left atrial appendage. The left atrial muscle extends a variable distance within the pulmonary veins to prevent reflux during atrial contraction. The left atrial appendage, overlying the left circumflex coronary artery, is smaller, longer, more tortuous, and less triangular than the right atrial appendage, often containing two or more lobes. Left atrial contraction generates a stroke volume of 20 to 30 mL.
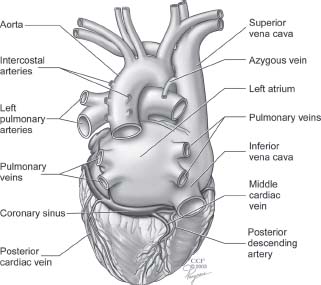
FIGURE 3.5 Posterior view of the heart and great vessels.
Left Ventricle
The left ventricle is a high-pressure, muscular chamber, 2.5 to 3 times thicker than the right ventricle (see Fig. 3.4). It is ellipsoid, or cone shaped when viewed from the right, and ring or doughnut shaped when viewed in cross section from the left. It is longer and narrower than the right ventricle, measuring approximately 7.5 cm in length and 4.5 cm in width. Structurally, the left ventricle consists of the inflow tract, the apical zone, and the left ventricular outflow tract. The anterior mitral leaflet separates the left ventricle into the posterior inflow tract and the anterior outflow tract. The septum consists of a large inferior muscular portion and a small superior membranous portion. The septum is thickest at the midportion and thinnest at the membranous portion near the aortic valve. The membranous septum has AV and intraventricular portions divided by the septal tricuspid leaflet. The His bundle is located within the interventricular portion of the membranous septum.
The left ventricular free wall measures approximately 8 to 12 mm and is thicker at the base than at the apex. It is composed of three layers: the endocardium, the myocardium, and the epicardium (or visceral pericardium). The outer two-thirds of the myocardium contains compact layers of muscle that twist and spiral inward from apex to base during contraction. The inner third of the myocardium consists of a latticework of trabeculae carneae that are more intricate than right ventricular trabeculations. The septal surface of the left ventricle is smooth.
Two papillary muscles, the larger anterolateral and the smaller posteromedial, arise from the free wall and have a variable number of heads. They anchor the chordae tendineae of the mitral valve, which are thicker than tricuspid valve chordae. Chordae tendineae restrict valve excursion during ventricular systole, thereby preventing the mitral valve leaflets from prolapsing into the left atrium. Most chordae arise from the heads of the papillary muscles, but some arise from the free wall. Chordae from one papillary muscle may diverge and attach to both mitral leaflets. False chordae occur in half of normal hearts, and may connect walls, papillary muscles, and the septum, but are not attached to the mitral leaflets. They often cross the left ventricular outflow tract and can be identified by echocardiography. Many false chordae contain extensions of left ventricular conducting fibers.
Blood enters the left ventricle via the mitral valve and is ejected at a 90- to 120-degree angle through the aortic valve. The ejection phase is shorter in the left ventricle, but the pressure is greater compared with right ventricular contraction.
CARDIAC VALVES
Tricuspid Valve
The tricuspid valve is the largest of the heart valves and maintains forward flow of blood through the right heart (Fig. 3.6). The functional components of the tricuspid valve include the three leaflets, commissures, annulus, chordae tendineae, papillary muscles, and the right ventricle. The leaflets are named for their anatomic position: anterior, posterior, and septal. The anterior leaflet, which is the largest and the most mobile, partially separates the right ventricular inflow and outflow tracts. The posterior leaflet is the smallest, whereas the septal leaflet is the least mobile and is occasionally absent. The valve leaflets are attached to a discontinuous fibrous annulus that has a “D” shape. Chordae tendineae (tendinous cords) are attached to the edges and undersurface of each leaflet and are anchored by the papillary muscles and the interventricular septum.
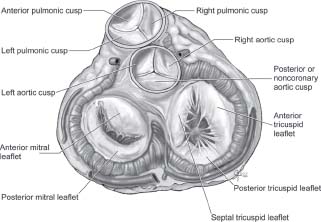
FIGURE 3.6 Cross-sectional view of the cardiac valves.
Pulmonic Valve
The pulmonic valve is the most anterior valve of the heart, located between the right ventricular outflow tract and the main pulmonary artery (see Fig. 3.6). It is the mirror image of the aortic valve, containing right, left, and anterior cusps (or leaflets) that are thinner than those of the aortic valve. The pulmonary sinuses are partially embedded within the right ventricular infundibulum. During systole, the valve opens to form a rounded, triangular-shaped central orifice.
Mitral Valve
The mitral valve is named after the miter, a tall ornamental hat worn by bishops and abbots (Figs. 3.6 and 3.7). The valve, located between the left atrium and the left ventricle, maintains the forward flow of blood in the left heart. The mitral valve has six components: leaflets, commissures, annulus, chordae tendineae, papillary muscles, and left ventricle. When viewed from the side, the valve is funnel shaped, with the leaflets forming an apex protruding into the left ventricle. There are two mitral leaflets, the anterior and the posterior, which have similar surface areas but different shapes. The anterior leaflet is semicircular or oval shaped, broader but narrow transversely. It partially separates the left ventricular inflow tract from the left ventricular outflow tract. The posterior leaflet is crescent shaped, longer and narrower, half the height but twice the length of the anterior leaflet. It attaches over two-thirds of the posterior valve circumference. The posterior leaflet has two or more indentations forming three scallops (the middle usually is the largest). During atrial contraction, the valve forms an ellipsoid orifice. During ventricular contraction, the atrial side of the leaflets coapt, preventing regurgitation of blood into the atrium. Two commissures, the anterolateral and the posteromedial, separate the two leaflets. The chordae tendineae prevent the mitral valve from prolapsing into the left atrium during ventricular systole. Approximately 100 primary, secondary, and tertiary chordae attach to the free edge and underside of the valve and are anchored by two papillary muscles in the left ventricle. Some of the posterior leaflet chordae arise from the left ventricular free wall. Unlike the tricuspid chordae, mitral chordae do not have insertions into the septum. The mitral valve is surrounded by a saddle-shaped fibrous ring, the mitral annulus, which anchors the valve. It is connected to the tricuspid annulus by the right fibrous trigone (central fibrous body), forming part of the fibrous skeleton of the heart.
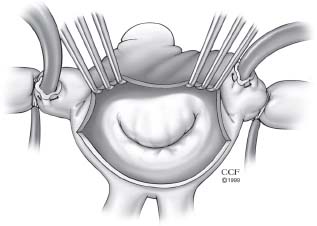
FIGURE 3.7 Surgical view of the atrial surface of the mitral valve.



