Chapter 4
Carbon monoxide transfer factor: single breath method
The carbon monoxide transfer factor (TLCO) measurement is one of the more physiologically and technically complex tests performed in the respiratory function laboratory. The TLCO, also known as the carbon monoxide diffusing capacity (DLCO), estimates the transfer of carbon monoxide from the alveolar gas to the red blood cell and represents the integrity of the gas exchange process of the alveolar–capillary membrane. The most commonly used method to measure the TLCO is the single breath method, which is discussed in this chapter.
The test is performed by asking the subject to attach to a mouthpiece and commence tidal breathing with lips tightly sealed and a nose peg in place. After a couple of tidal breaths, the subject is asked to exhale to residual volume (RV) and then take a rapid vital capacity (VC) breath in of a special test gas mixture to total lung capacity (TLC). The test gas mixture consists of carbon monoxide (CO), oxygen and nitrogen and an inert gas, commonly helium or methane. Once at TLC, the subject breath holds for approximately 8 s and then exhales to RV again. The first portion of the exhaled breath is discarded (dead space washout) and a sample of the remaining exhaled breath is collected for analysis (Figure 4.1). From the gas analysis, volume measurements and timing, parameters of carbon monoxide transfer factor can be calculated. A detailed explanation of the test methodology and calculations can be found in (1).
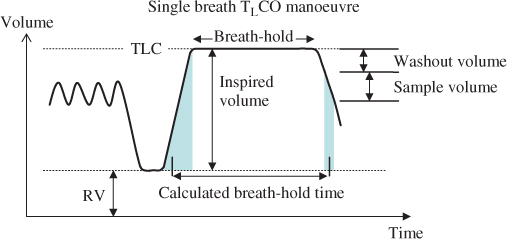
Figure 4.1 Spirogram of the single breath carbon monoxide transfer factor manoeuvre.
The parameters of carbon monoxide transfer factor used in the assessment of test quality and interpretation are as follows:
- TLCO: The transfer of CO across the lung; a measure of the ease of transfer of gas across the lung.
- Units: mmol/min/kPa (SI units) or mL/min/mmHg.
- To convert mmol/min/kPa to mL/min/mmHg, multiply TLCO by 2.987.
- Units: mmol/min/kPa (SI units) or mL/min/mmHg.
- VA, alveolar volume: the alveolar volume participating in gas exchange.
- Units: litres (L)
- KCO, transfer coefficient: the efficiency of uptake of CO in the alveoli, kCO, corrected for barometric pressure in the lung.
- Units: mmol/min/kPa/L (SI units) or mL/min/mmHg/L
- VI, the inspired volume: used for quality assessment.
- Units: L
- TLCOHbcorr: the TLCO corrected to a standard haemoglobin value (described in more detail later).
Test quality
- Acceptability criteria (1):
- VI is ≥85% of the largest VC.
- VI occurs in less than 4 s.
- Breath-hold time is 10 ± 2 s.
- Breath hold is stable with no evidence of Mueller or Valsalva manoeuvres, or leaks.
- Expiration of washout and sample collection occurs in <4 s (<3 s for sample collection time).
- Appropriate clearance of dead space volume.
- Proper analysis of alveolar gas sample.
- VI is ≥85% of the largest VC.
- Repeatability criteria(1):
- A minimum of two acceptable tests.
- The values of each test are within 1 mmol/min/kPa or within 10% of the highest value.
- A minimum of two acceptable tests.
- Tests not meeting the above criteria must be interpreted with caution.
- Breath hold and sample collection times are often increased in obstruction.
- VI < 85% of largest VC: TLCO and VA may be reduced when there is a failure to inhale to TLC. If VI is reduced due to an inability to exhale to RV, but a breath to TLC is achieved, there is thought to be little effect on TLCO or VA.
- Increasing or decreasing pulmonary capillary blood volume may lead to overestimation or underestimation of TLCO, respectively.
- Inadequate washout of dead space prior to collecting sample may lead to underestimation of TLCO.
- Where leaks are detected—the effort should be rejected and not used for interpretation.
- VI < 85% of largest VC: TLCO and VA may be reduced when there is a failure to inhale to TLC. If VI is reduced due to an inability to exhale to RV, but a breath to TLC is achieved, there is thought to be little effect on TLCO or VA.
- Breath hold and sample collection times are often increased in obstruction.
- Test quality should be noted by the operator in the technical comment to inform those interpreting results.
Factors to consider during interpretation
The carbon monoxide transfer factor test makes an assessment of gas exchange. Therefore, apart from the technical factors involved in the performance of the test, other factors that may impact on gas exchange need to be taken into consideration during interpretation.
Carbon monoxide transfer factor (TLCO)
TLCO may be affected by factors as shown in Table 4.1. Some of these factors can be accounted for by strict adherence to test performance criteria or by applying corrections to the measured values.
Table 4.1 Factors affecting TLCO.
| TLCO may be reduced due to following reasons: | Examples: |
|
|
|
|
|
|
|
|
|
|
| TLCO may be increased due to following reasons: | |
|
|
|
|
|
|
|
|
|
|
The effects of some of these factors are described in more detail:
- Haemoglobin (Hb)
- A reduced Hb results in a lower TLCO, and an increased Hb results in a higher TLCO due to the reduced or increased binding sites for CO on red blood cells, respectively.
- TLCO values are often standardised to account for variability of haemoglobin. The parameter is notated as TLCOHbcorr (TLCO corrected for Hb) and is standardised to Hb of 13.4 g/dL for children (<15 years) and females, and 14.6 g/dL for males. Haemoglobin correction equations are available in (1).
- Both the TLCO corrected and uncorrected for haemoglobin are important to consider in interpretation. The TLCOHbcorr provides insight into the integrity of the alveolar membrane and pulmonary vasculature, allowing comparisons to be made over time without the complication of variation in haemoglobin. The uncorrected TLCO provides information about functionality. For example, Case 5 shows that the integrity of the alveolar membrane and pulmonary vasculature is intact (TLCOcorrHb > LLN), while the uncorrected TLCO shows impaired gas exchange, due to anaemia, impacting on the subject’s functionality.
- A reduced Hb results in a lower TLCO, and an increased Hb results in a higher TLCO due to the reduced or increased binding sites for CO on red blood cells, respectively.
- Carboxyhaemoglobin (COHb)
- An elevated COHb results in an underestimation of TLCO due to a decreased diffusion gradient of CO from the alveolus to capillary blood, and due to the creation of an anaemia-like effect due to reduced binding sites.
- Smoking and exposure to cigarettes and other environmental sources may produce sufficient levels of CO to adversely affect TLCO measurement. Carbon monoxide correction equations are available in (1).
- Where a correction for COHb is not made, a cautionary comment could be added to the report describing the possible increased exposures (for example, cigarette smoking prior to test—5 in last 4 h—may result in underestimation of TLCO).
- An elevated COHb results in an underestimation of TLCO due to a decreased diffusion gradient of CO from the alveolus to capillary blood, and due to the creation of an anaemia-like effect due to reduced binding sites.
Alveolar pO2
An increased PAO2, for example, seen in patients on supplemental oxygen therapy, results in an underestimated TLCO due to increased competition for CO to haemoglobin-binding sites. Similarly, hyperventilation can also affect PAO2 and TLCO.
- Subjects on supplemental oxygen should have oxygen therapy removed for at least 10 min prior to the test being performed, where it is safe to do so, to minimise this effect. Correction equations for tests performed at higher PAO2 are available in (1).
- A decreased PAO2, as a result of assessment at altitude, for example, results in an overestimated TLCO due to reduced competition for CO to haemoglobin-binding sites. Correction equations for tests performed at altitude are available in (1). PAO2 can also be reduced as a result of an increased PACO2. It has been estimated that for every 0.133 kPa fall in PAO2, TLCO will increase by 0.31–0.35% (1).
- Pulmonary capillary blood volume.
- Increases in pulmonary capillary blood volume will result in increases in TLCO (e.g. Mueller manoeuvre, exercise) and decreases in blood volume will result in falls in TLCO (e.g. Valsalva manoeuvre). Avoidance of these conditions is included as acceptability criteria for the test.
- Moving from an upright to supine posture will result in an increase in TLCO due to changes in the distribution of the blood volume throughout the lung.
- There is some suggestion that changes in blood volume/distribution in the lungs account for increases in TLCO seen in some subjects with stable asthma or obesity (2).
- Increases in pulmonary capillary blood volume will result in increases in TLCO (e.g. Mueller manoeuvre, exercise) and decreases in blood volume will result in falls in TLCO (e.g. Valsalva manoeuvre). Avoidance of these conditions is included as acceptability criteria for the test.
Alveolar volume
VA may be reduced due to the following reasons:
- Incomplete expansion of the lungs (e.g. neuromuscular disease, incomplete inhalation to TLC)
- Loss of lung units (e.g. pneumonectomy, atelectasis, localised lung destruction)
- Poor mixing of inspired gas (e.g. significant airflow obstruction)
In an individual, it is possible that a reduced VA may be the result of more than one of the above causes (2).
The transfer coefficient, KCO
KCO will be affected by conditions affecting TLCO or VA.
Interpretation
- The main parameters used for the interpretation of TLCO are as follows:
- TLCO
- VA
- KCO
- TLCO
Carbon monoxide transfer factor test results are generally reported in conjunction with spirometry. Static lung volumes (SLV), TLC in particular, can also be helpful in interpreting changes in VA (see later).
Limits of the normal range
- For TLCO and VA, generally abnormally low results are of interest. The LLN is set at a z-score of −1.64.
- For KCO, both abnormally high and low results are of interest. The upper limit for normal (ULN) and lower limit of normal (LLN) are set at z-scores of ±1.96.
A reduced TLCO is functionally abnormal regardless of the cause (e.g. anaemia, reduced VA, parenchymal dysfunction).
- The impact of haemoglobin and carboxyhaemoglobin on TLCO should be considered where information is available. TLCO may be reduced due to transport issues primarily (anaemia, CO back pressure) rather than parenchymal or pulmonary vascular abnormalities.
- Similarly, the impact of changes in PIO2 should be accounted for where required.
When VA is reduced, TLC measured by SLV (plethysmography or multiple breath washout) may provide information regarding the cause:
- There is a relationship between worsening airway obstruction (FEV1/FVC) and a worsening VA/TLC (3, 4), probably explained by poor gas mixing.
- A VA/TLC close to unity may indicate loss of lung units as the cause of a reduced VA (3, 4).
Table 4.2 offers a strategy for interpretation using TLCO, VA and KCO.
Table 4.2 Interpretation strategy for carbon monoxide transfer factor using TLCO, VA and KCO.
| TLCO | Other parameters | Report |
| >LLN | VA > LLN | TLCO is within normal limits |
| VA < LLN | TLCO is within normal limits in the presence of a reduced alveolar volume | |
| <LLN | VA > LLN | Alveolar volume is within normal limits and TLCO is reduced, suggestive of parenchymal or pulmonary vascular disease |
| VA < LLN | Both TLCO and VA are reduced with a decreased KCO, suggestive of parenchymal or pulmonary vascular disease | |
| KCO < LLN | ||
| VA < LLN | Both TLCO and VA are reduced. As the KCO is in the normal range, the TLCO may be reduced due to the reduction in alveolar volume, parenchymal or pulmonary vascular disease or a combination of these. | |
| LLN < KCO < ULN | ||
| VA < LLN | Both TLCO and VA are reduced. The elevated KCO suggests that the reduction in TLCO is due to incomplete expansion of alveoli rather than parenchymal or pulmonary vascular disease. | |
| KCO > ULN |
KCO in the interpretation strategy
At the time of writing, the value of KCO in the interpretation strategy is uncertain and controversial. Although some (2) stress that KCO plays an integral role in the assessment of gas exchange and utilise it as a primary parameter in the interpretation strategy, others (5, 6) remain cautious about its value in the interpretation strategy and believe it has little role in interpretation of gas exchange.
Part of the reason for the differing views may be that KCO is often incorrectly described as a ‘correction for alveolar volume’. KCO is a rate constant describing the carbon monoxide transfer factor per unit alveolar volume for the alveolar volume at which the measurement is made. The relationship between TLCO and VA, measured as a proportion of TLC, is not linear (i.e. KCO changes as VA/TLC changes) (2) and, therefore, cannot be described as ‘correction’. For a detailed review of the use of KCO in interpretation, see (2).
For simplicity, we have used KCO in the interpretation strategy only after TLCO and VA have been examined. This limits the role of the KCO to a few isolated situations as follows:
- When both TLCO and VA are reduced and:
- KCO is elevated (>ULN), factors external to the lungs should be considered as the cause. KCO tends to be elevated when there is incomplete expansion of alveoli to TLC (e.g. poor inspiratory effort, respiratory muscle weakness, chest wall restriction) (2, 5).
- KCO is in the normal range, interpret with caution. Pathology may be present when KCO is normal in the presence of a reduced TLCO and VA. The result may be due to loss of lung units (discrete or diffuse), poor gas mixing, parenchymal or pulmonary vascular dysfunction or a combination of these. (2)
- KCO is low (<LLN), parenchymal or pulmonary vascular disease is probably the predominant cause (2, 7).
- KCO is elevated (>ULN), factors external to the lungs should be considered as the cause. KCO tends to be elevated when there is incomplete expansion of alveoli to TLC (e.g. poor inspiratory effort, respiratory muscle weakness, chest wall restriction) (2, 5).
- When TLCO is in the normal range and VA is reduced:
- Where KCO is elevated (>ULN), consider
- incomplete alveolar expansion (see explanation earlier).
- Where KCO is elevated (>ULN), consider
- When TLCO is in the normal range (usually markedly increased) and VA is within normal limits or reduced:
- Where KCO is elevated (>ULN), consider
- alveolar haemorrhage (2).
- Where KCO is elevated (>ULN), consider
Comparison to previous results
- Published studies (8, 9) suggest that a change > ±1.60 mmol/min/kPa over the short term and >10% in the longer term (year) probably reflect clinically significant changes.
Examples of interpretation of carbon monoxide transfer factor
Interpretation is performed using the following steps as applicable:
- Check for requirements of cautionary statements related to the following:
- Reference values (are values appropriate for this subject? See Chapter 1 for details.).
- Quality of test (read technical comments, check raw data if required).
- Factors affecting TLCO measurement (e.g. noting recent smoking if no correction for COHb is made).
- Quality of test (read technical comments, check raw data if required).
- Reference values (are values appropriate for this subject? See Chapter 1 for details.).
- Read clinical notes
- Interpret spirometry
- Interpret SLV measurements (if available)
- Assess response to inhaled bronchodilator (BD)
- Assess spirometry loop shape
- Interpret TLCO (Table 4.2)
- Write technical interpretation
- Compare results to previous
- Put results into clinical context
In the following examples, corrections have been made for haemoglobin. No corrections for altitude have been made as tests were performed near sea level. No corrections for carboxyhaemoglobin are required and no corrections for increased PIO2 (supplemental oxygen) are required.

Full access? Get Clinical Tree


