Name
Target channel
Applicability
CYP
Remarks
Dihydropyridines
Nifedipine
L
HBP, AP
3A4
Slow-release tablets
Nicardipine
L
HBP, HF
2D6, 3A4
Slow-release tablets, intravenous
Nilvadipine
L, T
HBP
3A4
Nisoldipine
L
HBP
3A4
Nitrendipine
L
HBP, AP
3A4
Manidipine
L, T
HBP
3A4
Benidipine
L, T
HBP, AP
3A4, 3A5
Anti-proteinuric
Barnidipine
L, T
HBP
3A4
Amlodipine
L
HBP, AP
3A4
Efonidipine
L, T
HBP, AP
3A4
Anti-proteinuric
Felodipine
L
HBP
3A4
Cilnidipine
L, N
HBP
3A4, 2C19
Aranidipine
L
HBP
2C9, 3A4
Azelnidipine
L, T, P/Q
HBP
3A4
Anti-proteinuric
Benzodiazepines
Diltiazem
L
HBP, AP, SVT
3A4
Intravenous
Tetrandrine
L
HBP
3A4
Phenylalkylamines
Verapamil
L
SVT, AP
3A4
Intravenous
Devapamil
L
SVT
3A4
37.2 Pharmacological Characters of CCBs
Dihydropyridines are the prototype CCBs. They are more potent and selective for vascular (over cardiac) smooth muscle than the other two classes of CCBs. DHPs bind to inactive state of L-type voltage-dependent calcium channels to prevent their activation and subsequent calcium influx [1], and are often used to reduce systemic vascular resistance and arterial blood pressure. At clinical doses, DHPs show little inhibitory effects on cardiac conduction and contraction. They slightly increase heart rate, cardiac output, and stroke volume probably through sustained elevation of global sympathetic nerve activity. Sometimes, when short-acting DHPs are used to treat angina, the vasodilation and hypotension can lead to reflex tachycardia which can increase myocardial oxygen demand and worsen ischemic symptoms. The dihydropyridines are useful for esophageal spasm and vasospasm such as angina. For example, amlodipine is the most widely used DHP-type CCB. It manifests less negative inotropic effects and reflexes tachycardia than nifedipine and has established safety to treat patients with angina. Main actions of amlodipine include calcium entry blockade into vascular smooth muscle cells, decreasing systemic vascular resistance and blood pressure. L-type calcium channels are preferentially expressed in artery and arteriole rather than vein. Peripheral edema is a common side effect of DHPs. Amlodipine is metabolized in the liver by CYP3A4; thus, the dosing interval should be adjusted in the patients with cirrhosis. Biological half-life of amlodipine in normal subjects extends to 39 h, which allows once-a-day administration. Compared to verapamil, amlodipine can be used to treat hypertensive patients with cardiac conduction abnormalities.
Verapamil (a phenylalkylamine CCB) is relatively selective for the myocardium, reduces myocardial oxygen demand, and attenuates coronary vasospasm (Chap. 20). It has minimal effect on vascular smooth muscle and therefore causes less reflex tachycardia. The major mechanism of action is causing negative chronotropic and inotropic effects [1]. Verapamil inhibits L-type calcium channels in use-dependent manner. Thus, verapamil can be the treatment of choice for supraventricular tachycardia and is often used to treat angina where tachycardia can be the most important contributor to the high myocardial oxygen demand. Verapamil is categorized as class IV antiarrhythmic agent (Chap. 52). It does not only slow down cardiac conduction including AV node but also reduces contractility. Thus, verapamil is contraindicated in pregnant patients (Chap. 60) and for patients with heart failure and cardiac conduction defects such as AV nodal block. In contrast, verapamil is the treatment of choice for rate control of atrial fibrillation to increase AV nodal refractory period, whereas it is not effective for Wolf-Parkinson-White (WPW) syndrome or in the conversion or maintenance of sinus rhythm. Verapamil is also effective for atrial flutter and paroxysmal supraventricular tachycardia (AV nodal reentry) (Chap. 50). Verapamil is metabolized in liver with CYP3A4. After perioral administration, its plasma concentration reaches peak at 2 h, and biological half-life is about 6 h.
Diltiazem (a benzothiazepine CCB) is an intermediate class between DHPs and phenylalkylamines in their selectivity for vascular calcium channels. By both cardiac depressant and smooth muscle relaxant actions, diltiazem reduces arterial pressure without producing the same degree of reflex cardiac stimulation caused by DHPs. Diltiazem is prescribed for hypertensive patients or those with non-transmural myocardial infarction [2] (Chap. 20). Diltiazem is metabolized by CYP3A4, and its biological half-life is approximately 5 h following to oral administration. Similarly to verapamil, it is contraindicated for patients with heart failure and cardiac conduction abnormality and for pregnant patients (Chaps. 52 and 60). Depressor actions of diltiazem are weaker than DHP-type CCBs. Large doses of DHPs can be used for hypertension to adequately decrease blood pressure, as DHPs are rather selective for vascular calcium channels. However, dose titration of diltiazem is limited for hypertension because it shows significant affinity for both cardiac and vascular L-type calcium channels, leading to significant cardiac side effects. Of importance, diltiazem does not induce reflex tachycardia, possessing good indication for angina, especially spastic angina.
Although CCBs manifest differing molecular structures (Fig. 37.1), all of the CCBs are metabolized in the liver mainly with the aid of CYP3A4. Thus, any medications that interact with CYP3A4 affect the pharmacokinetics of CCBs. The following substances inhibit CYP3A4 to potentiate or prolong the actions of CCBs: grapefruit juice, cimetidine, sildenafil, triazole antifungals, erythromycin, and HIV protease inhibitors including ritonavir and saquinavir. Flavonoids in grapefruit are reported to reduce the activity of CYP3A4. In contrast, all medications such as rifampicin, phenytoin, carbamazepine, and phenobarbital that activate CYP3A4 weaken the actions of CCBs.
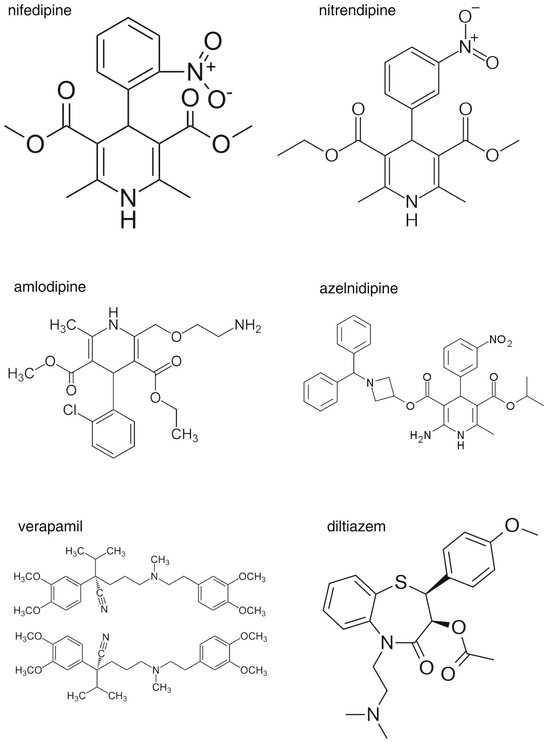
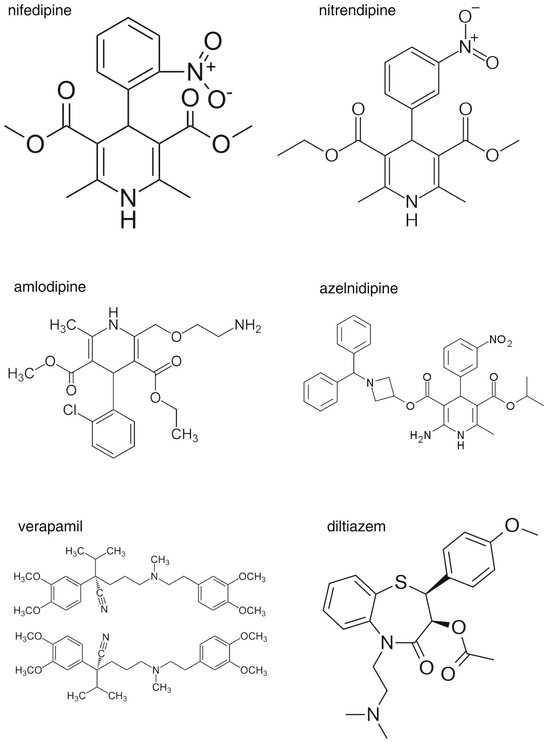
Fig. 37.1
Molecular structures of major calcium channel blockers used in clinical practice. As seen, 1,4-dihydropyridine is a molecule based upon pyridine that has been semi-saturated with two substituents replacing one double bond
37.3 Clinical Evidence for Calcium Channel Blockers to Inhibit Vascular Injury
In the early 1990s, several retrospective analyses pointed out that short-acting calcium channel blockers may increase the risk of myocardial infarction [3]; however, long-acting calcium channel blockers are safe for patients with coronary artery disease [4]. Observational studies reported that calcium channel blockers may increase the risk of cancer and bleeding [5, 6]. WHO responded to this confusion and published an ad hoc report stating there are no clinical evidences for serious adverse effects of calcium channel blockers [7]. Later, these concerns on calcium channel blockers were alleviated in a large-scale prospective randomized controlled trial [8]. Common adverse effects of CCBs include palpitation (reflex tachycardia), flushing (vasodilation), and peripheral edema (arteriolar dilation), related to their potent vasodilatory effects. In contrast to renin-angiotensin system inhibitors, CCBs can be used to control blood pressure during pregnancy.
Although salt restriction is essential for non-pharmacological treatment of hypertension, strict adherence to low dietary salt intake is not easy to achieve. The hypotensive effect of calcium channel blockers is less dependent on salt intake than other drugs, such as angiotensin-converting enzyme inhibitors [9, 10]. Therefore, calcium channel blockers could be prescribed for hypertensive patients who are addicted to salt. Calcium channel blockers established their safety for long-term use in the late 1990s.
37.4 Evidence of CCB to Improve CV Prognosis in Hypertensive Patients
In 1996, the STONE (Shanghai Trial of Nifedipine in the Elderly) study enrolled 1,632 elderly hypertensive patients to assess the effects of slow-release nifedipine on composite cardiovascular endpoints (stroke, heart failure, myocardial infarction, and sudden death) against placebo [11]. Slow-release nifedipine reduced the mean blood pressure by 22/13 mmHg and improved composite CV events. Subanalysis showed that slow-release nifedipine reduced stroke by 57 %.
In 1999, Syst-Eur (the Systolic Hypertension in Europe) study enrolled 4,695 elderly systolic hypertensive patients to compare the effect of nitrendipine against placebo on stroke [12]. Nitrendipine reduced blood pressure by 23/7 mmHg and the risk of stroke by 42 %. Subanalysis also showed that nitrendipine reduced cardiac events including heart failure, myocardial infarction, and sudden death. Collectively, CCBs reduce cardiovascular risk in hypertensive patients, compared to placebo.
37.4.1 Non-inferiority of Calcium Channel Blockers
The ALLHAT (the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial) enrolled 33,357 hypertensive patients over 55 years with any coronary risk factors to compare the effects of diuretics (chlorthalidone), calcium channel blocker (amlodipine), and angiotensin-converting enzyme inhibitor (lisinopril) on the composite endpoint of fatal and nonfatal myocardial infarction [8]. The primary results after a mean follow-up period of 4.9 years, published in 2002, showed similar risk reduction regarding the primary composite endpoint in all three groups. However, a statistically significant (P < 0.001) higher 6-year rate of hospitalized or fatal heart failure (secondary outcome) was observed with amlodipine (10.2 %) compared to chlorthalidone, diaretics (7.7 %).
Similar results were also noted in CASE-J (Candesartan Antihypertensive Survival Evaluation in Japan) study, which enrolled 4,728 Japanese high-risk hypertensive patients to compare the effects of amlodipine and candesartan on composite endpoints of sudden death, cerebrovascular, cardiac, renal, and vascular events [13]. The main results published in 2008 showed that the primary outcome for the composite endpoints did not differ between the two drugs, in spite of the candesartan group exhibiting a reduction in new-onset diabetes. Taking the findings of ALLHAT and CASE-J trials together, CCBs are not inferior to chlorthalidone, lisinopril, and candesartan in reducing cardiovascular risk.
In these clinical trials, the overall adverse event rates of hospitalization for gastrointestinal bleeding, cancer death, and angioedema were not significantly different for the amlodipine treatment group versus the comparator groups.
37.4.2 Superiority of CCB
In 2005, ASCOT-BRLA (the Anglo-Scandinavian Cardiac Outcomes Trial – Blood Pressure-Lowering Arm) study was published comparing the effects between amlodipine with perindopril and atenolol plus thiazide that included 19,257 high-risk hypertensive patients [14]. The primary endpoint was a composite of fatal and nonfatal myocardial infarction, and secondary endpoints were total and cardiovascular death, stroke, and coronary and total cardiovascular events. Although no difference was observed in the primary outcome, amlodipine-based treatment reduced the risk of total death (by 11 %), stroke (by 23 %), and total cardiovascular events (by 16 %) compared with atenolol. The data show that CCB-based treatment is superior to beta-blocker-based treatment in reducing vascular injury. Meta-analysis showed that CCBs are superior to the other antihypertensives including diuretics, angiotensin-converting enzyme inhibitors, and angiotensin receptor blockers in preventing stroke [15]. Even after the differences in blood pressure in each of the drug groups were adjusted, patients treated with CCBs showed a substantial reduction in the relative risk by 33 % for stroke. Of interest, CCBs decreased visit-to-visit variability of blood pressure, which could have contributed to a reduction of cardiovascular events, especially stroke [16].
37.5 CCBs Essentially Attain Target Blood Pressure Goal
Many clinical trials using CCBs have contributed to the determination of target blood pressure levels to which hypertensive patients should be treated [17, 18]. In other words, the use of CCBs helps to achieve target blood pressure levels for most hypertensive patients. Thus, CCBs are considered the basic drugs for the treatment of hypertension. The target diastolic blood pressure that prevents cardiovascular events and death was assessed in the HOT (Hypertension Optimal Treatment) trial, which enrolled 18,790 hypertensive patients treated with felodipine [17]. Patients were divided into three groups with differing target diastolic blood pressures: <90 mmHg, <85 mmHg, and <80 mmHg. The results showed that patients with diastolic pressures of 83 and 86 mmHg manifested the lowest cardiovascular events and deaths, respectively.
The FEVER (Felodipine Event Reduction) study enrolled 9,711 high-risk hypertensive Chinese patients 50–79 years old to assess the effects of felodipine on stroke against placebo [18]. At the end of study, blood pressure in the felodipine group was 137/82 mmHg, and that in the control group was 142/85 mmHg. The primary endpoint of fatal and nonfatal stroke was reduced by 27 % in the felodipine group compared to placebo (P = 0.001). Among secondary endpoints, all cardiovascular events were reduced by 27 % (P < 0.001), all cardiac events by 35 % (P = 0.012), all-cause deaths by 31 % (P = 0.006), coronary events by 32 % (P = 0.024), heart failure by 30 % (P = 0.239), cardiovascular death by 33 % (P = 0.019), and cancer by 36 % (P = 0.017) in the felodipine group compared to placebo. This suggests that systolic blood pressure lower than 140 mmHg is suitable as a target for preventing cardiovascular death and events including stroke, heart failure, and coronary events and that even a small difference in BP (4 mmHg systolic/2 mmHg diastolic) is associated with very substantial reductions in the incidence of most types of cardiovascular events. Do the results from clinical trials agree with epidemiological data? Japanese epidemiological data demonstrated that there is an increase in cardiovascular death or stroke when exposed to blood pressure above 140/90 mmHg [19, 20]. Thus, both epidemiological data and randomized controlled prospective trials provide evidence that 140/90 mmHg is a suitable target blood pressure for antihypertensive drug treatments.
37.6 High-Risk Hypertension
37.6.1 Elderly
Elderly patients may behave differently from young hypertensive patients in lowering of systolic blood pressure below 140 mmHg. To examine the effects of efonidipine on composite endpoint of cardiovascular events including cerebrovascular, cardiac, vascular, and renal events, JATOS (Japanese Trial to Assess Optimal Systolic Blood Pressure in Elderly Hypertensive Patients) study enrolled 4,508 Japanese elderly systolic hypertensive patients aged 65 to 85 years [21]. Patients were randomized into mild (140–160 mmHg) and strict (<140 mmHg) treatment groups and observed for 2 years. The study surprisingly demonstrated that the primary endpoint was similar in both treatment groups.
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


