Chest trauma
Chest trauma accounts for almost one half of all trauma occurrences and almost one fourth of all trauma-related deaths. Chest trauma is commonly classified as penetrating or blunt, depending on the type of injury. Penetrating chest trauma involves an injury by a foreign object, such as a knife (most common stabbing injury), bullet (most common missile injury), pitch fork, or other pointed object that penetrates the thorax. These are considered open injuries because the thoracic cavity is exposed to pressure from the outside atmosphere. Blunt chest trauma, which is considered a closed chest injury, results from sudden compression or positive pressure inflicted by a direct blow to the organ and surrounding tissue. Blunt chest trauma commonly occurs in motor vehicle accidents (when the chest strikes the steering wheel), falls, or crushing injury.
Typically, penetrating chest trauma is fairly limited, usually involving isolated organs and lacerated tissues. In some cases, however, extensive tissue damage can occur if a bullet explodes in the chest cavity. Blunt chest trauma can cause extensive injury to the chest wall, lung, pleural space, and great vessels. Injuries resulting from blunt chest trauma include pulmonary contusion, rib fractures, pneumothorax, hemothorax, and rupture of the diaphragm or great vessels. (See
Injuries Associated with Chest Trauma, pages 36-41.) Blunt injuries are associated with multisystem organ injuries and carry a higher mortality rate than penetrating injuries.
CAUSES AND INCIDENCE
Motor vehicle accidents cause two-thirds of major chest trauma in the United States. Other common causes include sports and blast injuries and cardiopulmonary resuscitation. About 50% of these injuries affect the chest wall; 80% of those with significant blunt chest trauma also have extrathoracic injuries.
Chest trauma accounts for 70% of all trauma-related deaths in the United States. Injuries to the chest usually involve one or more of these conditions:
• hypoxemia resulting from airway alteration, damage to the chest muscles, lung parenchyma or ribs, severe hemorrhage, collapse of the lungs, or pneumothorax
• hypovolemia resulting from massive fluid loss
• cardiac failure resulting from an increase in intrathoracic pressure or
subsequent cardiac injury such as cardiac tamponade or contusion.
Tissue damage caused by penetrating trauma, such as an impaled object or foreign body, is related to the object size as well as the depth and velocity of penetration. For example, penetrating chest trauma by a bullet has many variables. The extent of injury depends on the distance at which the weapon was fired, the type of ammunition, the velocity of the ammunition, and the entrance and (if present) exit wounds. Additional factors to be considered when assessing the extent of a penetrating chest injury include the type of weapon; for example, the caliber, barrel, and length of a gun and the powder composition. An intact bullet causes less damage than a bullet that explodes on impact. A bullet that explodes within the chest may break up and scatter fragments, burn tissue, fracture bone, disrupt vascular structures, or cause a bullet embolism.
Injury resulting from blunt chest trauma is related to the amount of force, compression, and cavitation. Blunt force that strikes the chest wall at high velocity fractures the ribs and transfers that force to underlying organ and lung tissue. The direct impact of force is transmitted internally and the energy is dissipated to internal structures. The flexibility or elasticity of the chest wall directly affects the degree of injury. The first and second ribs take an enormous amount of blunt force to fracture and therefore are associated with significant intrathoracic injuries.
SIGNS AND SYMPTOMS
Signs and symptoms of blunt chest trauma depend on where the trauma initiates.
Rib fractures
• Tenderness
• Slight edema over the fracture site
• Pain that worsens with deep breathing and movement
• Shallow, splinted respirations
Sternal fractures
• Persistent chest pain, even at rest
• Severe dyspnea
• Cyanosis
• Agitation
• Extreme pain
• Subcutaneous emphysema
Flail chest
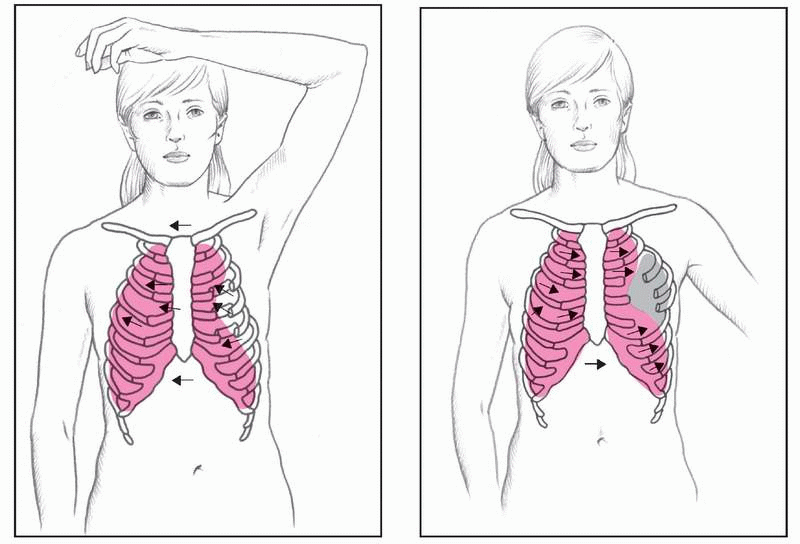
Multiple rib fractures within two or more places may cause flail chest, in which a portion of the chest wall “caves in,” causing a loss of chest wall integrity and preventing adequate lung inflation. (See
Flail chest: Paradoxical breathing, page 40.)
Signs and symptoms include:
• bruised skin
• extreme pain caused by rib fracture and disfigurement
• paradoxical chest movements
• tachycardia
• hypotension
• respiratory acidosis
• cyanosis
• rapid, shallow respirations
• tension pneumothorax.
Tension pneumothorax
• Severe dyspnea
• Absent breath sounds (on the affected side)
• Agitation
• Jugular vein distention
• Tracheal deviation (away from the affected side)
• Cyanosis
• Shock
Hemothorax
• Respiratory distress
• Severe dyspnea with restlessness and pallor or cyanosis
• Asymmetrical chest movements
• Flat jugular veins
• Bloody sputum or hemoptysis
• Unilateral decreased fremitus and decreased chest expansion on inspiration
• Dullness over the area of fluid collection
• Unilateral diminished or absent breath sounds
• Hypotension and tachycardia
Myocardial contusions
• Tachycardia
• Ecchymosis
• Chest pain
• Electrocardiogram (ECG) abnormalities
Diaphragmatic rupture
• Severe respiratory distress
• Bowel sounds in the chest
• Decreased vital capacity
COMPLICATIONS
• Hemothorax
• Hemorrhagic shock
• Airway compromise
• Pneumothorax
• Tension pneumothorax
• Diaphragmatic rupture
• Arrhythmias
• Liver laceration
• Myocardial tears or rupture
• Cardiac tamponade
• Pulmonary artery tears
• Ventricular rupture
• Rupture of the aorta
• Bronchial, tracheal, or esophageal tears
DIAGNOSIS
A history of trauma with dyspnea, chest pain, and other typical clinical features suggest a blunt chest injury. To determine its extent, a physical examination and diagnostic tests are needed.
• In hemothorax, percussion reveals dullness. In tension pneumothorax, it reveals tympany. Auscultation may reveal a change in position of the loudest heart sound.
• Chest X-rays may confirm rib and sternal fractures, pneumothorax, flail chest, pulmonary contusions, lacerated or ruptured aorta, tension pneumothorax, diaphragmatic rupture, lung compression, or atelectasis with hemothorax.
• With cardiac damage, the ECG may show abnormalities, including unexplained tachycardias, atrial fibrillation, bundle-branch block (usually right), ST segment changes, and ventricular arrhythmias such as multiple premature ventricular contractions.
• Serial aspartate aminotransferase, alanine aminotransferase, lactate dehydrogenase, creatine kinase (CK), and CK-MB levels are elevated. However, cardiac enzymes fail to detect myocardial damage in up to 50% of patients.
• Retrograde aortography, computed tomography angiography, and transesophageal echocardiography reveal aortic laceration or rupture.
• Contrast studies and liver and spleen scans detect diaphragmatic rupture.
• Echocardiography, computed tomography scans, and cardiac and lung scans show the injury’s extent.
TREATMENT
Blunt chest injuries call for controlling bleeding and maintaining a patent airway, adequate ventilation, and fluid and electrolyte balance. Further treatment depends on the specific injury and complications.
• Single fractured ribs are managed conservatively with mild analgesics and follow-up examinations to check for indications of a pneumothorax or hemothorax. To prevent atelectasis, the patient should perform incentive spirometry, deep breathing, and coughing for lung expansion. Intercostal nerve blocks may help with more severe fractures.
• Treatment for a pneumothorax involves inserting a spinal, 14G, or 16G needle into the second intercostal space at the midclavicular line to release pressure. Then the physician inserts a chest tube in the affected side to normalize pressure and reexpand the lung. The patient also receives oxygen and I.V. fluids. He may require intubation and mechanical ventilation.
• Shock related to hemothorax calls for I.V. infusion of lactated Ringer’s or normal saline solution. If the patient loses more than 1,500 ml of blood or more than
30% of circulating blood volume, he’ll also need a transfusion of packed red blood cells or an autotransfusion. He may also require intubation, mechanical ventilation, and possible thoracotomy. Chest tubes are inserted into the fifth or sixth intercostal space at the midaxillary line to remove blood.
• Treatment of flail chest may include endotracheal intubation and mechanical ventilation with positive pressure. The patient may also receive I.V. muscle relaxants. If the patient requires controlled ventilation, he’ll receive a neuromuscular blocking agent. If an air leak occurs, the patient may need operative fixation of the flail chest.
• Pulmonary contusions are managed with colloids to replace volume and maintain oncotic pressure. (Steroid use is controversial.) The patient may also need endotracheal intubation and mechanical ventilation as well as antibiotics, diuretics, and analgesics.
• Myocardial contusions call for cardiac and hemodynamic monitoring to detect arrhythmias and prevent cardiogenic shock. Drug therapy depends on the type of arrhythmia. Treatment is similar to that for myocardial infarction.
• Immediate surgical repair is mandatory for myocardial rupture, septal perforation, and other cardiac lacerations. Less severe ventricular wounds require use of a digital or balloon catheter. Atrial wounds require a clamp or balloon catheter.
The patient with an aortic rupture or laceration who reaches the hospital alive needs immediate surgery, using synthetic grafts or anastomosis to repair the damage. Such a patient requires a large volume of I.V. fluids (usually lactated Ringer’s solution) and whole blood along with oxygen at a very high rate. A pneumatic antishock garment is applied, and the patient is promptly transported to the operating room.
For a patient with a diaphragmatic rupture, a nasogastric tube is inserted to temporarily decompress the stomach, and the patient is prepared for surgical repair.
Drugs
• Mild analgesics for pain associated with fractures
• Analgesics and antibiotics to treat pneumothorax
• I.V. infusion of lactated Ringer’s or normal saline solution for shock
• I.V. muscle relaxants to relieve muscle spasms in flail chat; neuromuscular blocking agents may be needed if the patient requires mechanical ventilation
• Antibiotics, diuretics, and analgesics for pulmonary contusions
• Antiarrhythmics, analgesics, and inotropic drugs such as dobutamine or dopamine for myocardial contusions
• Short-acting beta-blocking agents such as labetalol or esmolol (Brevibloc) to control the heart rate and decrease the mean arterial pressure for myocardial rupture, septal perforation, and other cardiac lacerations
SPECIAL CONSIDERATIONS
• Check all pulses and level of consciousness. Evaluate skin color and temperature, depth of respiration, use of accessory muscles, and length of inhalation compared to exhalation.
• Check pulse oximetry values for adequate oxygenation.
• Observe tracheal position. Look for distended jugular veins and paradoxical chest motion.
• Listen to heart and breath sounds carefully; palpate for subcutaneous emphysema (crepitation) or a lack of structural integrity of the ribs.
• Obtain a history of the injury. Unless severe dyspnea is present, have the patient locate the pain, and ask if he’s having trouble breathing. Obtain laboratory studies (arterial blood gas analysis, cardiac enzyme studies, complete blood count, type, and crossmatch).
Simple rib fractures
• Have the patient cough and breathe deeply to mobilize secretions while splinting to decrease pain.
• Give adequate analgesics, encourage bed rest, and apply heat. Don’t strap or tape the chest.
Severe fractures
• Administer intercostal nerve blocks.
• Obtain X-rays before and after the nerve blocks to rule out pneumothorax.
• Intubate the patient with excessive bleeding or hemopneumothorax.
• Chest tubes may be inserted to treat hemothorax and to assess the need for thoracotomy.
• To prevent atelectasis, turn the patient frequently and encourage coughing and deep-breathing exercises.
Pneumothorax
• Placement of a chest tube anterior to the midaxillary line at the fourth intercostal space may be required to aspirate as much air as possible from the pleural cavity and to reexpand the lungs.
• When time permits, insert chest tubes attached to water-seal drainage and suction.
Flail chest
• Place the patient in semi-Fowler’s position.
• Reexpanding the lung is the first definitive care measure.
• Administer oxygen at a high flow rate under positive pressure.
• Suction the patient frequently and as completely as possible.
• Maintain acid-base balance.
• Observe carefully for signs of tension pneumothorax.
• Start I.V. therapy using lactated Ringer’s or normal saline solution.
Hemothorax
• Treat shock with I.V. infusions of lactated Ringer’s or normal saline solution.
• Administer packed red blood cells for blood losses greater than 1,500 ml or circulating blood volume losses exceeding 30%.
• Administer oxygen.
• The patient may need insertion of chest tubes in the fourth intercostal space anterior to the midaxillary line to remove blood.
• Monitor and document vital signs and blood loss.
• Watch for and respond immediately to falling blood pressure, rising pulse rate, and hemorrhage, all of which require a thoracotomy to stop bleeding.
Pulmonary contusion
• Give limited amounts of colloids (such as salt-poor albumin, whole blood, or plasma) as appropriate to replace volume and maintain oncotic pressure.
• Give analgesics, as necessary
• Monitor blood gas levels to ensure adequate ventilation; provide oxygen therapy, mechanical ventilation, and chest tube care.
Cardiac damage
• Close intensive care or telemetry may detect arrhythmias and prevent cardiogenic shock.
• Impose bed rest in semi-Fowler’s position (unless the patient requires shock position); administer oxygen, analgesics, and supportive drugs to control heart failure or supraventricular arrhythmias, as needed.
• Watch for cardiac tamponade, which calls for pericardiocentesis.
• Provide essentially the same care as for a patient with a myocardial infarction.
Diaphragmatic rupture
• Insert a nasogastric tube to temporarily decompress the stomach, and prepare the patient for surgical repair.
Chronic bronchitis
Chronic bronchitis is inflammation of the bronchi caused by irritants or infection. The distinguishing characteristic of bronchitis is obstruction of airflow. In chronic bronchitis, a form of chronic obstructive pulmonary disease, hypersecretion of mucus and chronic productive cough are present during 3 months of the year for at least 2 consecutive years. Only a minority of patients with the clinical syndrome of chronic bronchitis develop significant airway obstruction.
CAUSES AND INCIDENCE
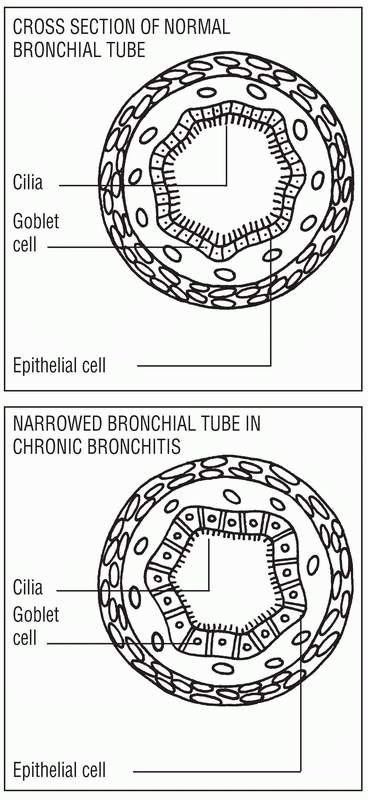
According to the National Center for Health Statistics, approximately 14 million people have chronic bronchitis, but this number may be underestimated. Chronic bronchitis develops when irritants are inhaled for a prolonged time. The irritants inflame the tracheobronchial tree, leading to increased mucus production and a narrowed or blocked airway. As the inflammation continues, changes in the cells lining the respiratory tract increase resistance in the small airways, and severe imbalance in the ventilation-perfusion ([V with dot above]/[Q with dot above]) ratio decreases arterial oxygenation.
Chronic bronchitis can result from a series of attacks of acute bronchitis or recurrent respiratory infections, or it may gradually evolve because of smoking or inhalation of air contaminated with other pollutants in the environment. Smoking is by far the most important of these factors; smoking impairs ciliary action and macrophage function, inflames airways, increases mucus production, destroys alveolar septa, and causes peribronchiolar fibrosis. The mucusproducing layer of the bronchial lining becomes thickened over time with such narrowing of the airway, whereby breathing becomes increasingly difficult. With immobilization of the cilia that sweep the air clean of foreign irritants, the bronchial passages become more vulnerable to further infection and the spread of tissue damage.
Chronic bronchitis causes hypertrophy and hyperplasia of airway smooth muscle and hyperplasia of the mucous glands, increased number of goblet cells, ciliary damage, squamous metaplasia of the columnar epithelium, and chronic leukocytic and lymphocytic infiltration of bronchial walls. (See
Changes in chronic bronchitis.)
Hypersecretion of the goblet cells block the free movement of the cilia, which normally sweep dust, irritants, and mucus away from the airways. Accumulating mucus and
debris impair the defenses and increase the likelihood of respiratory tract infections. (See
Mucus buildup in chronic bronchitis, page 48.)
Additional effects include narrowing and widespread inflammation within the airways. Bronchial walls become inflamed and thickened from edema and accumulation of inflammatory cells, and smooth muscle bronchospasm further narrows the lumen. Initially, only large bronchi are involved, but eventually all airways are affected. Airways become obstructed and close, especially on expiration, trapping the gas in the distal portion of the lung. Consequent hypoventilation leads to a [V with dot above]/[Q with dot above] mismatch and resultant hypoxemia and hypercapnia.
SIGNS AND SYMPTOMS
• Chronic bronchitis, insidious in onset, with productive cough and exertional dyspnea
• Upper respiratory infections associated with increased sputum production and worsening dyspnea, which take progressively longer to resolve
• Copious sputum (gray, white, or yellow)
• Weight gain due to edema
• Cyanosis
• Tachypnea
• Wheezing
• Prolonged expiratory time
• Use of the accessory muscles of respiration