Bypass Grafts: Surgical Aspects and Complications
Siddharth Bhende
Patrick S. Vaccaro
VASCULAR CONDUITS
Modern vascular surgical bypass grafts are credited to work done by Carrel in the early 1900s where he described the use of autogenous vein bypass grafts in dogs. Since then there have been long-standing attempts to identify the best conduit for arterial reconstruction. The success of vascular bypasses depends on certain host characteristics including the quality of inflow, quality of outflow, and the characteristics of the bypass graft. These graft characteristics vary depending on whether it is a biologic or manufactured graft.
The ideal graft would be readily available in a variety of sizes, be antithrombogenic, and provide long-term durability and patency. It should be easy to handle and elastic to account for the normal pulsatility of the artery. The graft should be biocompatible, as antigenicity can promote an intense inflammatory response and promote thrombosis. Currently, the ideal vascular graft does not exist and so we must make do with a variety of natural and prosthetic conduits, which will be discussed in more detail below (Table 29.1).
Vein Grafts
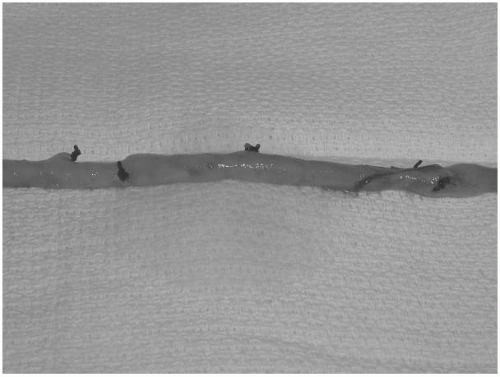
Vein grafts can be obtained from a variety of locations, but the most common site is the greater saphenous vein (GSV) (Fig. 29.1). The length and diameter of the GSV make it suitable for a variety of different bypasses. However, the saphenous vein may not be usable in 10 to 20% of cases for a variety of reasons, including previous saphenectomy for coronary or lower extremity revascularization, history of superficial phlebitis, poor caliber, or congenital absence. Contralateral GSV is an excellent choice for lower extremity revascularization if the ipsilateral vein is not available. In patients with peripheral artery disease, one must be cautious that the patient will be able to heal the vein harvest site from the contralateral leg. The lesser saphenous vein is another source for autogenous vein conduit. It generally extends from the lateral border of the Achille’s tendon to the popliteal fossa where it drains into the popliteal vein. During its harvest, the surgeon must be careful to avoid injuring the sural nerve. Upper extremity veins (basilic and cephalic) can also be used as autogenous vein alternatives. However, there is much variability in the size and duplication of these veins. Futhermore, in patients who have undergone repeated venipuncture these veins may be quite sclerotic.
There are a number of factors that can affect the patency of vein bypass grafts. These include the pressure at which the vein is distended at the time of harvest, the use of vasoactive substances to dilate the vein, and the temperature at which the vein is stored after harvest and prior to implantation. Overdistension of a venous conduit has a negative effect on the biologic responsiveness of the graft. If the distending pressure exceeds 200 mm Hg, significant endothelial cell dysfunction is observed. The use of vasoactive substances, such as papaverine, helps to preserve endothelial morphology. Cold storage of a vein graft is deleterious, but storage at body temperature is ideal for preserving endothelial cell function and prostacyclin production.
TABLE 29.1 TYPES OF VASCULAR BYPASS CONDUITS | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||
Care must be taken in harvesting vein grafts to prevent undue traction or pressure on the vein as well as to minimize handling. The vein can be removed through continuous or skip incisions. The use of skip incisions has been advocated when harvesting GSV to decrease the incidence of wound complications. Side branches are mobilized and ligated with silk sutures and hemoclips. Care must be taken to prevent crimping of the vein lumen during ligation of the side branches. Vein graft size is also important when determining whether a segment of vein is suitable for use as a bypass conduit. In general, veins less than 3 mm in diameter have lower patency rates. Vein sizes can be assessed preoperatively with the use of duplex ultrasonography (DUS). Smaller veins can be used if no other suitable conduit is available, but it requires meticulous dissection and the use of pharmacologic agents to prevent vasospasm. If a single segment of vein is not of adequate length for a bypass, particularly in lower extremity revascularization, multiple segments of veins can be spliced together. The patency rate of these spliced veins is less than that of a single piece of vein of adequate length.
Once implanted all vein grafts undergo morphologic changes in response to the hemodynamic forces of the arterial circulation. This process is termed arterialization and is a normal adaptive response. In some cases, however, the vein graft can deteriorate over time. Deterioration occurs in the first 30 days and is generally due to technical errors, patient selection, and the initial quality of the conduit. Between 30 days and 2 years of time, vein grafts can develop neointimal hyperplasia at anastomotic and valvulolysis sites. This occurs in approximately 10 to 30% of patients with the majority occurring within the first 12 months. After 24 months, changes that occur are generally due to progression of atherosclerosis. Aneurysmal degeneration of vein grafts can occur with time and is discussed later in more detail.
Arterial Grafts
Arterial bypass grafts are widely accepted as the best bypass conduit currently available. Many of their innate properties allow them to function with superiority. Arterial grafts are able to maintain their viability, do not degenerate with time, are resistant to infection, and demonstrate proportional growth when used in children. Arterial conduits are harvested from three main sites within the normal vascular tree: the internal iliac artery, the external iliac artery, and the superficial femoral artery. Most often, these donor sites can then be reconstructed using prosthetic conduits which are better tolerated in these locations than the original site of bypass. In children and young adults, the internal iliac artery has been harvested with no postoperative morbidity and no long-term morbidity. Even the thrombosed superficial femoral artery can be harvested to use as a bypass conduit. Patency is restored by performing an eversion endarterectomy of the resected portion. Most arterial bypass grafts are used in the abdomen for visceral vessel reconstruction or in the groin region. Due to size and availability, arterial conduits are rarely used in the aortic location or for lower extremity arterial bypass.
Biologic Grafts
When venous and arterial bypass grafts are not suitable, the surgeon must find another source for an adequate conduit. A variety of different conduits have been studied over the years and a few of the grafts that are still in clinical use are described here.
Umbilical Vein Grafts
The human umbilical cord provides approximately 50 cm of vein that can be dilated up to 7 mm in diameter. Initial experience involved the use of unmodified heterografts. Problems with immunologic rejection generally occurred several weeks after implantation. Rejection can lead to thrombosis or graft degeneration. This led to the use of glutaraldehyde-tanned umbilical veins. These grafts retain their basic architectural structure and the tanning process leads to protein cross-linking that increases the tensile strength of the grafts and masks its antigenicity. There are still instances of umbilical vein graft aneurysmal degeneration and therefore the graft is often wrapped in a polyester mesh.
Cryopreserved Grafts
Harvested vein and arterial segments from cadavers can be frozen for later use. Initial results with cryopreserved allografts resulted in high rates of immunologically derived biologic degradation and subsequent aneurysmal degeneration, calcification, rupture, and occlusion. Current cryopreservation techniques involve the use of cryoprotectants such as dimethylsulfoxide, atraumatic harvest of the vessel, and ultra-low-temperature freezing with liquid nitrogen. It has been reported that cryopreserved grafts can be stored up to a few years. Cryopreservation has been shown to preserve endothelium and reduce thrombogenicity. Degeneration of these grafts that is not attributable to immunologic rejection has been reported, including intimal disruption, luminal fibrin deposition, and cellular infiltrates in the media. Degenerative changes in the allograft are the major drawback of this technique. It has been suggested that a low dose of immunosuppression may prevent aneurysm formation, but many hesitate to use these drugs because of their serious potential adverse effects.
Prosthetic Grafts
Autogenous grafts are not always available or may be of inadequate length or caliber. The development of prosthetic vascular grafts arose to provide a substitute conduit in the absence of adequate autogenous material. Grafts are constructed in a variety of ways that affect their porosity, thrombogenicity, and compliance in order to help them mimic autogenous grafts. There are criteria that a prosthetic graft must meet in order to become an adequate conduit. First, the material must be biocompatible and free of toxic, allergic, and carcinogenic side effects. There is some reaction of the host to the foreign material, but this tissue reactivity is often a desirable
response leading to incorporation of the graft. Second, the graft must be durable and resist degradation and deterioration with time. Third, the graft should be readily available in a variety of lengths and diameters and should have adequate flexibility, yet be resistant to kinking.
response leading to incorporation of the graft. Second, the graft must be durable and resist degradation and deterioration with time. Third, the graft should be readily available in a variety of lengths and diameters and should have adequate flexibility, yet be resistant to kinking.
Porosity of prosthetic grafts is an important structural characteristic. The material obviously needs to be impervious to blood, but a porous framework has many potential advantages. Initial investigations suggested that a greater degree of porosity would promote fibrous encapsulation of the graft. Autogenous tissue ingrowth through the pores would initiate and provide adherence for a stable intimal lining. It has been hypothesized that unhindered ingrowth of tissue through large pores correlated with improved patency. This hypothesis has never been proven. In fact,it is more likely the innate thrombogenicity of the luminal graft surface plays a larger role in determining graft patency.
A variety of graft characteristics influence a prosthetic graft’s thrombogenicity. Upon exposure to blood, the graft is immediately coated with serum proteins, in particular fibrinogen. The ability of these proteins to interact with the graft is dependent upon the chemical and physical properties of the graft material. Platelets then adhere to the graft surface proteins to become activated, recruit more platelets, and activate local hemostatic reactions. The graft surface becomes lined with proteinaceous material and compacted fibrin to produce a pseudointima. Continuation of this process may lead to graft thrombosis. Much research has been devoted in attempts to “seed” prosthetic grafts with endothelial cells with the hopes of causing a complete endothelial lining, decreasing pseudointima formation and improving patency rates.
Graft compliance is an important mechanical property of grafts that affects their performance. Compliance is the ability of the graft to expand radially in response to increased pressure. In autogenous grafts this is related to the proportion of elastin and collagen within the vessel wall. Prosthetic grafts tend to be less compliant than autogenous grafts. Compliance has been shown to be directly related to the rate of thrombogenicity, but it is difficult to discern this factor from the many others that can affect graft thrombosis. External support can also be applied to prosthetic grafts that will minimize such events as kinking and mechanical compression.
A variety of materials have been investigated as possible materials from which to fabricate grafts. Two materials that have proven durable over time include Dacron (polyethylene terephthalate) and PTFE (polytetrafluoroethylene) (Fig. 29.2




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree