Chapter 6
Burn Injuries
Written by S. Hanekom, M. Wilson, B.M. Morrow and H. van Aswegen
The skin performs an important role as a physical barrier by protecting the body against fluid loss, mechanical damage and infection, as well as assisting with temperature regulation. However, the most important function of the skin is that it gives each individual their own identifying characteristics. The physical and emotional trauma that result from burn injuries are complex and can result in life-long psychological and physical disability. Burn injuries have been described as a global public health problem that affects both developing and developed countries (Atiyeh et al., 2009a; Peck, 2011, 2012). Burn injuries rank in the top 15 leading causes of the burden of disease globally. They are the fourth leading cause of traumatic injuries worldwide, following motor vehicle accidents, falls and interpersonal trauma. Morbidity and mortality vary with age and region (Atiyeh et al., 2009b; Peck, 2011, 2012).
This chapter covers:
•The causes and mechanisms of burn injuries.
•Types of burn injuries.
•The systemic effects of a burn injury.
•The classification of burn injuries.
•The medical and surgical management of a patient who has sustained a burn injury.
•Physiotherapy aims for the management of a patient who sustained a burn injury in the intensive care unit and burns ward.
•The contraindications and precautions related to the physiotherapy management of a patient with burn injuries.
•Physiotherapy interventions for patients who have suffered burn injuries.
•Adult and paediatric clinical case scenarios.
6.1. Causes and Mechanisms of Burn Injury
The worldwide incidence of fire-related injuries was estimated to be 1.1 per 100000 populations in 2004 (Forjuoh, 2006). The most vulnerable groups for burn injuries are children, women and the elderly. Lack of supervision of children, frailty and co-morbid illnesses of the elderly, clothing made of flammable materials, parental illiteracy, congested housing, preexisting impairment of a child and low socioeconomic status are important risk factors for burn injuries (Atiyeh et al., 2009a; Parbhoo et al., 2010; Peck, 2011; Balan and Lingam, 2012).
6.1.1. Injury in adults
Most burn injuries are preventable. Burn injuries are more prevalent in the domestic setting for women and children. Cooking has been identified as the most common activity that poses a risk for burn injury, particularly in lower-income countries, in which there is exposure to open flames and non-electric appliances used for cooking, heating and lighting. The elderly are particularly at risk (Peck, 2011). This is due to the deterioration in judgement and coordination. Medication use by the elderly may lead to alterations in cognition and balance, which places them at further risk of injury. The elderly are more likely to sustain an injury inside the house if they smoke or because they tend to use heating devices more frequently than younger adults. Adult men are more likely to be injured in outdoor and work locations (Peck, 2011).
The majority of burn injuries worldwide are unintentional. Less than 5% are deliberate self-burnings or the result of abuse, with regional exceptions (Peck, 2012). Assault, usually by a spouse, is most often caused by throwing caustic chemicals or flammable liquids at the victim’s face or genitalia or by the ignition of clothing (e.g. dowry deaths in India) (Shaha and Mohanthy, 2006; Kumar et al., 2013). In locations with seasonal variations of temperature, burns occur more frequently in the colder winter months. Clothing ignition, such as bedclothes and loose-fitting cotton garments, is a common cause of unintentional and intentional severe flame burns. Work-related injuries account for 20–25% of all serious burns, with the most common being fire or flame and scald. Food service industries (e.g. restaurants that use deep fryers) are responsible for 12% of work-related injuries (Dissanaike and Rahimi, 2009; Dissanaike et al., 2009; Teo et al., 2012).
6.1.2. Injury in paediatrics
Infants in Africa have an incidence of fire-related burns that is three times the world average for this age group (Peck, 2011). In children younger than three years, scalds are responsible for most of the burns (Lowell et al., 2008). Scald burns usually occur when a child accidentally pulls a container with hot liquid onto themselves. It may also result from bathtub submersion injuries, usually by an unattended child. In older children, flame burns are more common. Young children are particularly vulnerable to thermal injury, partly due to a lack of discernment about what could be hazardous. In addition, the relative immobility of infants means that they may not be able to move away from the hot substance or surface, which can result in a deeper burn (Birchenough et al., 2008). Burns account for 10% of all cases of child abuse (Parbhoo et al., 2010). Contact with heated objects including cigarettes, irons, curling irons, hair dryers and heated kitchen utensils are commonly used in abuse cases (Van Niekerk et al., 2004; Parbhoo et al., 2010).
6.2. Types of Burn Injuries
A burn is a traumatic injury to the skin or other organic tissue primarily caused by thermal or other acute exposures. Burns occur when some or all of the cells in the skin or other tissues are destroyed by heat, cold, electricity or caustic chemicals. Burns are acute wounds caused by an isolated, non-recurring insult and the majority of burn injuries progress rapidly through an orderly series of healing steps. Flame injuries are the most common causes of burns. This is followed by scalding, contact with a hot object, electrical and chemical injuries (Sheridan, 2002).
The following types of burn injuries are discussed in this section:
•chemical,
•electrical,
•inhalation, and
•thermal.
6.2.1. Chemical burns
Chemical burn injuries may occur as a result of assault, attempted suicide or may be work-related. In work-related injuries the extremities are mostly involved, whereas in the case of assault or attempted suicide the head, neck and trunk are mostly affected (Olaitan and Jiburum, 2008; Tahir et al., 2012; Li et al., 2013). Injury to the skin and underlying structures is caused by a wide range of corrosive reactions. This includes alteration of pH, disruption of cellular membranes and direct toxic effects on metabolic processes. Injury severity is determined by the duration of exposure and the nature of the agent. Tissue coagulation will result from acid contact, while alkaline burns results in liquefactive necrosis. Systemic absorption of some chemicals is life threatening (Palao et al., 2010). Complications associated with chemical burns include respiratory failure, septicaemia, renal failure, blindness, axillary contractures and hypertrophic scarring, to name a few, and often lead to a prolonged hospital stay (Olaitan and Jiburum, 2008).
6.2.2. Electrical burns
Electrical injury occurs mostly in electricians, construction workers and children playing at home. Electrical injury has a mortality rate as high as 58% (Saracoglu et al., 2014). Electrical injury is classified as high-voltage, low-voltage, electric arc or lightning strike (Table 6.1). Electrical energy is converted to thermal injury as the current passes through body tissues with different levels of conductivity. Patient presentation differs from no external evidence of burn injury with major internal organ injuries to skin burns with no significant internal organ injury (Herrera et al., 2010; Salehi et al., 2014). The degree of injury sustained due to electrical current is influenced by the magnitude of the energy delivered, resistance encountered by bodily tissues (dependent on water content of tissues), type of current and current pathway, as well as the duration of contact. Tissues with high water content offer low resistance to electrical current flow (Herrera et al., 2010). Patients with total body surface area (TBSA) burns greater than 50% have an 18.8 times greater risk of mortality (Saracoglu et al., 2014). Patients who have suffered electrical burns need close monitoring for cardiac arrhythmias. Tissue oedema may lead to the development of compartment syndrome and reinforces the need for close patient monitoring after electrical burns (Kasten et al., 2011).
Table 6.1:Classification of electrical burns and complications associated with each type of burn*.
| Electrical injury | Definition | Complications |
| High voltage | Electrical current greater than 1000 volts. Most debilitating of all electrical injuries. | •Cardiac arrest •Cardiac dysrhythmias •Muscle necrosis (escharotomy, fasciotomy) •Amputation of extremities and digits •Fractures •Traumatic brain injury •Peripheral mono- or polyneuropathy •Exposed tendons •Sepsis •Pigmented urine (indicates muscle damage) •Renal failure •Cataract formation |
| Low voltage | Electrical current less than 1000 volts. Most common sources are electrical appliances in the home. | •Fewer complications than high voltage injuries •Fasciotomy •Amputation |
| Electric arc | Flash-type injury in which the current does not pass directly through the body. Lowest mortality rate of all electrical injuries. | •Fasciotomy •Seldomly amputation |
| Lightning strike | Injury results from sudden, short-duration, high-intensity electrical energy. It is associated with blunt trauma due to violent tetanic muscle contraction and large fluctuations in temperature during lightning strike. | •Cardiac arrhythmia •Cardiac and respiratory arrest (more frequently than high voltage injury) •Blunt head trauma •Spinal cord injury •Solid intra-abdominal organ injury •Fractures (long bones, orbit, scapula and vertebrae) •Rupture of tympanic membrane •Corneal burns •Cataracts •Peripheral neuropathy •Impaired mental ability |
*Sources: Whitcomb et al. (2002); Arnoldo et al. (2004); Russell et al. (2013).
6.2.3. Inhalation burns
Inhalation injury is defined as the aspiration of superheated gasses, steam, hot liquid and toxic products of incomplete combustion. Inhalation burns are a predictor of injury severity, need for ventilation and mortality (Osler et al., 2010; Kasten et al., 2011). Inhalation injuries will increase the risk of death by 20% irrespective of the victim’s age and the extent of the burn injury (Osler et al., 2010). There are three phases of inhalation injury (upper airway thermal injury, lower airway and lung parenchyma chemical injury and systemic toxicity), which are discussed below.
6.2.3.1. Upper airway injury
Thermal injury is usually limited to the oropharyngeal area due to the poor conductivity of dry air, rapid heat dissipation of the smoke-filled air and reflex closure of the glottis. Animal experiments have shown that at 142°C, inhaled air cools to 38°C by the time it reaches the carina. The thermal injury results in mucosal oedema; this peaks at 24 hours after the initial insult and resolves within the first week. This oedema can cause upper airway obstruction and will develop independent of fluid resuscitation. Steam can burn the airway below the glottis due to the high conductivity of moist air (Mlcak et al., 2007). Because the paediatric airway is much smaller than that of an adult, it may be more rapidly and readily occluded as a result of oedema after thermal injury (Sheridan, 2002).
6.2.3.2. Lower airway and lung parenchyma injury
The lower respiratory tract is mostly damaged by steam inhalation, but toxic chemicals (aldehides, oxides of sulphur and nitrogen) produced in fires may also injure the lower airways with chemical burns. Inhalation of the toxic products resulting from incomplete combustion destroys the epithelial layer of the airways, resulting in airway sloughing. In reaction to the damaged epithelium, mucosal oedema develops, causing airway obstruction. The release of oxygen free radicals and inflammatory mediators contribute to the development of pulmonary oedema, which may occur within two days after injury (Church et al., 2006). In addition, hyper-secretion of mucus and epithelial ciliary damage decreases the effectiveness of the mucociliary clearance system. As a result, patients present with excessive amounts of secretions which further increase airways obstruction. This, coupled with surfactant inactivation due to destruction of type II pneumocytes, could result in atelectasis. Ultimately, ventilation/perfusion (V/Q) mismatch develops as the alveolar injury progresses, while there is an increase in lung and bronchial blood flow (Demling, 2008). A clinical picture consisting of a decrease in lung compliance, hypoxia and hypercarbia develops. If not managed effectively, pneumonia may develop any time between four days and four weeks after inhalation injury (Demling, 2008).
Key Message
The physiotherapist must be aware that bronchospasm is a common problem for young children after inhalation injury.
6.2.3.3. Systemic toxicity
The inhalation of toxic gases causes extensive damage to cellular functioning. Carbon monoxide is produced during combustion and, when inhaled, carbon monoxide decreases the ability of oxygen to bind to haemoglobin due to its high affinity for haemoglobin. This results in decreased oxygen delivery to organs, thereby impairing cellular respiration. In addition, carbon monoxide also binds to the enzyme cytochrome oxidase and inhibits mitochondrial function at a cellular level. Carbon monoxide poisoning should be suspected if the inhalation injury took place in an enclosed area and the patient is unconscious. The symptoms of carbon monoxide poisoning include increased muscle tone, nausea and vomiting, headache, hyperventilation, hypotension and coma (Demling, 2008).
Combustion of plastics, polyurethane, wool, silk, nylon, rubber and paper products can all lead to the production of cyanide gas. Cyanide interferes with cellular metabolism by binding the ferric ion in cytochrome a3. Anaerobic metabolism ensues, with the development of lactic acidosis and decreased oxygen utilisation. Cyanide poisoning should be suspected in burn patients who present with persistent lactic acidosis despite adequate fluid resuscitation (Huzar et al., 2013). The extent of the damage caused during inhalation injury is related to duration of exposure and the nature of the materials aspirated.
6.2.4. Thermal burns
The depth of the burn injury is related to contact temperature, duration of contact with the external heat source and the thickness of the skin. Because the thermal conductivity of skin is low, most thermal burns involve the epidermis and part of the dermis. The most common thermal burns are associated with flames, hot liquids, hot solid objects and steam. The depth of the burn largely determines the healing potential and the need for surgical grafting and will be discussed in Section 6.4 (Sheridan, 2002; Church et al., 2006).
Cold temperatures can cause burn injury. In cold exposure, damage to the skin and underlying tissues occurs when ice crystals puncture the cells or when the crystals create a hypertonic tissue environment. As a result, blood flow can be interrupted, causing haemo-concentration and intravascular thrombosis with tissue hypoxia (Sheridan, 2002).
6.3. Systemic Effects of a Burn Injury
6.3.1. Burn shock
In the first 24 hours following a major burn incident (excess of 20% body surface area (BSA) involved) the functioning of the body is affected. Systemic inflammatory response develops due to the release of cytokines and other mediators into the bloodstream. As a result the capillary permeability increases, which allows for a ‘seeping’ of protein-rich fluid into the intravascular compartment with resultant build up of interstitial oedema in various organs and soft tissues; often referred to as ‘third-spacing’ of fluid. In addition, peripheral and splanchnic vasoconstriction occurs due to the release of catecholamines, vasopressin and angiotensin. Myocardial contractility may also be reduced (refer to Chapter 1 (Section 1.2) for information on shock). Bronchospasm can occur during this initial phase even in the absence of inhalation injury. Adequate fluid resuscitation is crucial to the survival of the patient during this phase of injury. The effective management of patients in this early phase has improved the survival of burn patients (Mosier et al., 2013).
Children have nearly three times the BSA to body mass ratio of adults, resulting in proportionally higher fluid losses in children than in adults. Therefore, children have relatively greater fluid resuscitation requirements and more evaporative water loss than adults (Sharma and Parashar, 2010).
6.3.2. Immune system responses
Patients with extensive burn injuries are at a significantly increased risk for developing severe sepsis. This is due to the loss of the cutaneous protective barrier, suppression of specific and non-specific immune systems, hyper-catabolism and the placement of invasive lines, which is essential for the effective monitoring and nursing of the patient (refer to Chapter 1 (Section 1.2.3.) for information on sepsis and septic shock).
6.3.3. Metabolic responses
There is an increased metabolic response rate as a result of burn injury. Metabolic rates increase up to three times the normal value and this increased rate can remain up to one year after the closure of a burn wound. Hyper-catabolism has been linked to an increased risk for sepsis, difficulty in wound closure and a decrease in lean body mass (Chan and Chan, 2009). Increased levels of circulating catabolic hormones result in decreased protein synthesis and a rapid breakdown of visceral and skeletal muscle. Increased osteoclastic activity can also make patients more susceptible to fractures. In children with burns that exceed 40% of BSA, a 5.8% incidence of fractures has been reported. The authors speculated that increased osteoclastic activity, decreased vitamin D levels, inadequate protein intake and decreased weight-bearing activity after burn injury were to blame (Mayes et al., 2003).
6.3.4. Thermoregulatory system
The thermoregulatory system resets to a higher baseline temperature of around 38.5ºC after burn injury. Adult patients suffer from hyperthermia due to the metabolic response to systemic inflammation or an infective process. Cellular injury and death may ensue if hyperthermia is sustained above 40ºC (Nachiappan et al., 2012).
The large BSA to body mass ratio of the child, in addition to the thinner skin and subcutaneous layers, predisposes the child to hypothermia, which is important to avoid. In very young children, temperature regulation is partially based on non-shivering thermogenesis, which further increases metabolic rate, oxygen consumption and lactate production. The thin skin in young children may make the initial burn depth assessment difficult (Sharma and Parashar, 2010).
6.4. Classification of Burn Injuries
The skin consists of two main layers, namely the epidermis and dermis. A basement membrane connects the epidermis to the dermis and the dermis is attached to the underlying bone and muscles through a hypodermis (does not form part of the skin). Table 6.2 lists the composition and functions of the layers of the skin.
Burn wounds are classified according to the depth of tissue injury and the extent of the burns.
6.4.1. Depth of tissue injury
Burn wounds are not usually uniform in depth and many have a mixture of deep and superficial components. A precise classification of the burn wound may be difficult and may require up to three weeks for a final determination. Thin skin, particularly on the volar surfaces of the forearms, medial thighs, perineum and ears, sustains deeper burn injuries than suggested by initial appearance. It is best to assume there are no shallow burns in these areas. Children under the age of five and adults over the age of 55 are also more susceptible to deeper burns because of thinner skin.
Table 6.2:Composition and functions of the epidermis and dermis.
| Skin layer | Composition | Function |
| Epidermis | •Keratinocytes •Melanocytes | •Provides a protective cover for the body against infiltration by micro-organisms •Assists with temperature regulation of the body through controlled water loss |
| Dermis | •Collagen fibrils •Elastic fibres •Nerve endings •Hair follicles •Sweat glands •Sebaceous glands •Lymphatic and blood vessels | •Protects the body against injury from external forces •Provides sense of touch and heat •Nourishes and removes waste from epidermal and dermal cells |
The traditional classification of burns as first, second, third or fourth degree is now replaced by a system that reflects the need for surgical intervention. Current designations of burn depth are superficial, superficial partial thickness, deep partial thickness and full thickness. The term fourth degree is still used to describe the most severe burns. These are burns that extend into the muscle, bone and joints.
6.4.1.1. Superficial burns
Superficial or epidermal burns involve only the epidermal layer of the skin. They do not blister but are dry, painful, red and blanch with pressure. Over the following two to three days the pain and erythema subside. By day four, the injured epithelium peels away from the newly healed epidermis. Such injuries are generally healed in six days without scarring. This process is commonly seen with sunburns (Rice and Orgill, 2012).
6.4.1.2. Partial thickness burns
Partial thickness burns involve the epidermis and portions of the dermis. They are characterised as either superficial or deep (Kasten et al., 2011; Rice and Orgill, 2012).
6.4.1.2.1. Superficial partial thickness burns
These burns characteristically form blisters between the epidermis and dermis within 24 hours and are painful, red, weeping and blanch with pressure. Burns that initially appear to be only epidermal in depth may be determined to be partial thickness 12–24 hours later. These burns generally heal in seven to 21 days; scarring is unusual, although pigment changes may occur. A layer of fibrinous exudates and necrotic debris may accumulate on the surface, which may predispose the burn wound to heavy bacterial colonisation and delayed healing. These burns typically heal without functional impairment or hypertrophic scarring.
6.4.1.2.2. Deep partial thickness burns
These burns extend into the deeper dermis and are characteristically different from superficial partial thickness burns. Deep burns damage hair follicles and glandular tissue. They are painful to pressure only, almost always blister, are wet or waxy dry and have variable mottled colorization from patchy cheesy white to red (Fig. 6.1). They do not blanch with pressure. If infection is prevented and wounds are allowed to heal spontaneously without grafting, they will heal in three to nine weeks. These burns invariably cause hypertrophic scarring (see Section 6.8.5.3.), particularly in children (Sheridan, 2002). If they involve a joint, joint dysfunction is expected even with aggressive physical therapy. A deep partial thickness burn that fails to heal in three weeks is functionally and cosmetically equivalent to a full thickness burn. Differentiation from full thickness burns is often difficult.
6.4.1.3. Full thickness burns
Full thickness burns extend through and destroy the epidermis, all layers of the dermis and often injure the underlying subcutaneous tissue. If a burn is deep and circumferential then eschar (dead and denatured dermis) will form. With oedema and increased pressures there can be compression of the neurovascular structures. This compression acts like a tourniquet and compromises the viability of structures distal to the eschar (limb or torso) (Fig. 6.2). Full thickness burns are usually anaesthetic or hypoaesthetic. Skin appearance can vary from waxy white to leathery grey to charred and black. The skin is dry, inelastic and does not blanch with pressure. Hairs can easily be pulled from hair follicles. Vesicles and blisters do not develop.
Fig. 6.1:A patient with deep partial thickness and full thickness burns to the legs as a result of exposure to hot tar. Skin grafting has been performed to enhance wound healing.
The eschar eventually separates from the underlying tissue and reveals an unhealed bed of granulation tissue. Without surgery, these wounds heal by wound contracture with epithelialisation around the wound edges. Scarring is severe with contractures and complete spontaneous healing is not possible (Rice and Orgill, 2012).
Fourth degree burns are deep and potentially life-threatening injuries that extend through the skin into underlying tissues such as fascia, muscle or bone (Rice and Orgill, 2012). Contractures potentially result in significant loss of function. Contractures commonly occur in the neck, the web spaces and flexor surfaces of the hand, the ante-cubital space of the arm, axilla, popliteal space of the knee and the hip flexor surfaces (Birchenough et al., 2008). In children, contracture bands may impede the growth of both bony and soft tissue structures (Sheridan et al., 1999).
6.4.2. Extent of burn wounds
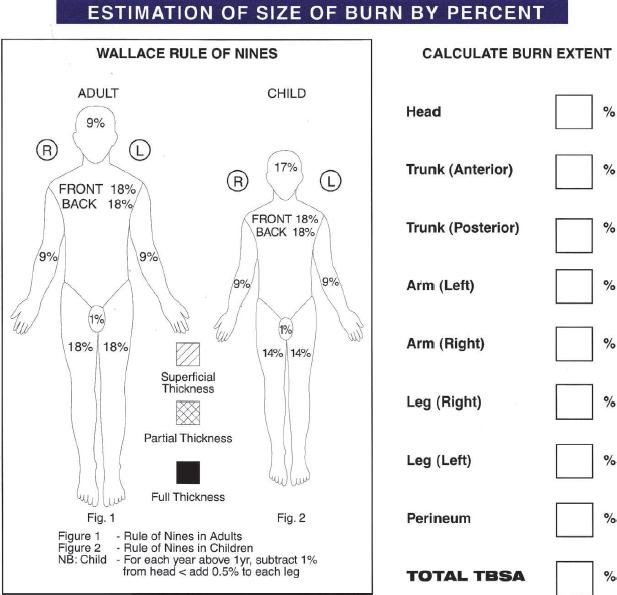
The extent of the burn wounds are expressed as a percentage of the TBSA involved in the injury. This is necessary to guide therapy (Freiburg et al., 2007). The two commonly used methods of assessing TBSA are the rule of nines and the Lund Browder chart. The Lund Browder chart is the most accurate method for estimating TBSA for both adults and children as it takes into account the relative percentage of BSA affected by growth. Children have proportionally larger heads and smaller lower extremities, so the percentage BSA is more accurately estimated using the Lund Browder chart (Panté et al., 2010; Alharbi et al., 2012). For adult assessment, the most expeditious method to estimate TBSA is the rule of nines (Fig. 6.3).
Fig. 6.3:Example of rule of nines chart used in the emergency department to calculate percentage of TBSA involved by burn injury.
The revised Baux score has been developed as a tool for the assessment of mortality risk for burn injured patients (Osler et al., 2010). This score considers the effect of inhalation burn, in addition to age and TBSA, on patient survival (refer to Section 6.10 for suggested further reading on the revised Baux score). Overestimation by health care providers of the percentage TBSA involved remains problematic and newer methods to calculate burn surface area are being investigated. These methods include computerised imaging, two- and three-dimensional graphics and body contour reproductions. Research is underway to establish whether these newer methods will improve accuracy in initial wound assessment (Kasten et al., 2011).
6.5. Medical and Surgical Management
Advances in the medical and surgical management of patients with burn injury have improved the mortality and morbidity. The medical and surgical management of patients with burn injuries is divided into:
•primary survey and resuscitation of vital functions;
•detailed secondary survey as adjunct to the primary survey; and
•definitive care.
6.5.1. Primary survey and resuscitation of vital functions
On admission to the emergency department, the adult or paediatric patient with burn injury will undergo initial assessment and treatment according to the ‘airways, breathing, circulation, disability, exposure’ (ABCDE) approach to basic life support, as described in Chapter 5 (Section 5.3.1.). Components of the ABCDE approach that are especially important for patients with burn injuries include the following (Alharbi et al., 2012).
•Airway patency. If soot is present in the mouth, early intubation should be considered even if the patient is breathing normally, as mild pharyngeal oedema can rapidly progress to upper airway obstruction (Latenser, 2009).
•Presence or absence of breathing. In the case of stridor, immediate airway intubation is indicated.
•Injuries by exposing the patient through the removal of clothes in order to visualise the skin and identify injuries. The patient’s clothes are removed but the patient is kept warm in order to prevent the onset of hypothermia. The room temperature should be kept between 28ºC and 32ºC in order to keep the patient’s core temperature above 34ºC. This is particularly important in the management of children with thermal injuries.
The type of radiological investigations performed and the care provided to the patient is similar to that described in Chapter 5 (Section 5.3.1.). Nasogastric tube placement is undertaken for patients with 20% or greater TBSA burns.
6.5.2. Secondary survey as adjunct to primary survey
The secondary survey may take place in the emergency department or in the burn unit. It is a ‘head-to-toe’ evaluation of the patient, which involves taking a detailed history of the patient as well as a complete neurological and physical examination including the abdomen, cornea, ears (especially with explosion trauma), genital region, lower and upper limbs. The history should include mechanism of injury, time of injury, consideration of abuse (especially if the patient is a child) and lastly, possibility of carbon monoxide intoxication (based on presence of soot in the mouth and nose and on a history of burns in a closed area) (Alharbi et al., 2012).
Care and treatment provided to the patient during the secondary survey is similar to that described in Chapter 5 (Section 5.3.2.).
6.5.3. Definitive care
Definitive care is initiated after completion of the primary and secondary surveys. Definitive care has been broken down into care provided over the first 24 hours, surgery and wound management. Each of these is discussed below.
6.5.3.1. Care provided over the first 24 hours
6.5.3.1.1. Fluid replacement
The Parkland formula is a formula used to calculate a patient’s fluid replacement requirements over the first 24 hours following burn injury in order to ensure they remain haemodynamically stable. It is the most widely used resuscitation guideline and has been renamed the consensus formula (Blumetti et al., 2008; Latenser, 2009; Alharbi et al., 2012). The amount of ringer’s solution to be administered is calculated using the consensus formula, 4 ml/kg/% TBSA burn. One half of the amount is administered during the first eight hours following injury and the other half is divided equally and administered over the next 16 hours. The formula is regarded as an excellent starting point for fluid resuscitation (Blumetti et al., 2008). Some patients may need more fluid volume than that predicted with the formula, especially those with burn inhalation injury, electrical burns or history of alcohol or illicit drug use; therefore close monitoring of each individual patient to assess whether their fluid needs are being met is of great importance (Latenser, 2009). Monitoring includes regular measurements of arterial blood pressure, heart rate and urine output. A heart rate less than 110 beats per minute indicates adequate fluid volume administration (Latenser, 2009). The aim of fluid replacement therapy is to maintain a urine output of 0.5 ml/kg/hour in adults and an output of 0.5–1 ml/kg/hour in patients who weigh less than 30 kg (Blumetti et al., 2008; Latenser, 2009; Alharbi et al., 2012). Invasive cardiac monitoring may become necessary for patients with severe injury in order to determine preload on the heart.
Ringer lactate, ringer acitate or balanced electrolyte solutions may be used for fluid replacement therapy over the first 24 hours of admission. The use of colloids and other blood products is not recommended during this time period as these have been shown to prolong tissue oedema and increase the risk for mortality (Latenser, 2009; Alharbi et al., 2012).
6.5.3.1.2. Calorie intake
Patients with burns have a markedly increased caloric requirement because of the development of a hypermetabolic response after injury as a result of the burn itself, catecholamine release, pain and anxiety, surgical interventions and tissue metabolic demands. Delivery of appropriate nutrition (including protein and carbohydrate) to a patient with burn injuries is vital for wound healing, management of inflammation, suppression of the hypermetabolic response and reduction of sepsis-related morbidity and mortality (Kasten et al., 2011). The patient’s caloric needs are determined using the Harris Benedict equation or the Curreri formula (Alharbi et al., 2012). Adult patients with 20% TBSA burn or greater will be fed through enteral feeding tubes (nasojejunal or orojejunal) to ensure adequate nutrition is supplied to meet the patient’s energy needs (Hall et al., 2012). In general, a child with a burn greater than 20-30% TBSA will require placement of a nasoduodenal feeding tube to provide the required caloric supplementation (Sharma and Parashar, 2010).
6.5.3.1.3. Routine interventions
Routine interventions include screening for bacterial colonisation. This is done using cotton swabs that are swiped over different bodily areas such as the mouth, nose, burn and inguinal areas. Re-evaluation of the TBSA and depth of burn wounds is performed after the patient is washed. At this stage determination of indications for emergent surgery (debridement, escharotomy or skin grafting) is done. Circumferential burns over the abdomen may lead to organ hypoperfusion and could lead to burn-induced compartment syndrome. Abdominal compartment syndrome can lead to impairment in renal function, gastrointestinal ischaemia, and poor perfusion of the cardiac and pulmonary systems (Latenser, 2009). Compartment syndrome may also develop in extremities with circumferential burns. Intra-abdominal pressure should be monitored regularly for the early identification of the development of compartment syndrome.
6.5.3.1.4. Laboratory tests
Laboratory tests that are ordered for patients with burn injuries within the first 24 hours of admission are listed in Table 6.3.
Urea, electrolytes, myoglobin and urine culture are performed to assess renal function and to identify renal injury. Prothrombin time, partial thrombin time and international normalised ratio are done to establish the patient’s blood clotting profile. Creatine kinase and C-reactive protein are inflammatory markers, indicative of the patient’s immune response to injury (Alharbi et al., 2012).
Table 6.3:Routine laboratory tests performed following burn injury.
•Complete blood count •Arterial blood gas •Urea and electrolytes •Prothrombin and partial thrombin time •International normalised ratio •Creatine kinase and C-reactive protein •Blood glucose •Albumin, thyroid and myoglobin •Sputum culture and sensitivity •Urine culture |
6.5.3.1.5. Impaired respiration and inhalation injury
Circumferential burns of the neck or chest pose the threat of airway and ventilation compromise. Burns of the neck area, especially in children, can result in eschar, which compresses and obstructs the airway. Early removal of eschar could decrease the external pressure exerted on the trachea, thereby protecting the airway. Circumferential burns in the chest area restrict natural chest wall movement and lead to increasing ventilatory demands for good gaseous exchange. This is a surgical emergency. Signs that may indicate respiratory compromise in a patient with severe chest wall burns are listed in Table 6.4.
Smoke inhalation injury should be suspected when a patient presents with singed nasal hair, soot in the mouth, history of suppressed level of consciousness and confinement in an enclosed space (with or without facial burns), change in voice and expectoration of carbonaceous sputum (Dries and Endorf, 2013). Fibre-optic bronchoscopy is used to determine the extent of damage to the airways. Typical bronchoscopy findings in patients with inhalation injury are listed in Table 6.5.
Chest x-ray and computed tomography (CT) may be insensitive to the diagnosis of inhalation injury early in the patient’s admission due to a relatively normal lung and airway appearance (Kasten et al., 2011). Indications for intubation in patients with inhalation injuries are listed in Table 6.6 (Mlcak et al., 2007).
Table 6.4:Signs of respiratory compromise in a patient with severe chest burns.
•Visible eschar on the chest wall •Increased respiratory rate in a spontaneously breathing patient •Wheezing •Voice hoarseness •Reduced tidal volumes in a ventilated patient, with visibly increased work of •breathing to maintain adequate oxygenation •Decreased chest wall excursion |
Table 6.5:Typical bronchoscopy findings that confirm the diagnosis of inhalation injury.
•Carbonaceous deposits below the glottis •Extensive airway oedema •Bronchial mucosal erythema •Bronchial mucosal haemorrhage •Bronchial mucosal ulceration |
Table 6.6:Indications for intubation in patients with inhalation injury.
•Stridor •Hypoxaemia or hypercapnia •Facial burns and lowered level of consciousness •Facial burns and full thickness burns to the neck •Full thickness burns to the lips and nose •Oropharyngeal oedema •Carboxyhaemoglobin > 20% |
Medication recommended for patients with inhalation injury include anti-inflammatory and anti-coagulant drugs, bronchodilator therapy, inhaled nitric oxide (to improve pulmonary blood flow) and heparin sulphate combined with N-acetylcysteine. This regimen has been reported by some to reduce mortality from inhalation injuries in adult and paediatric patients (Church et al., 2006; Mlcak et al., 2007; Alharbi et al., 2012); however, one case report has stated that coagulopathy developed in a patient exposed to inhaled heparin and N-acetylcysteine (Dries and Endorf, 2013). The majority of patients with inhalation injury are at risk of developing ventilator-associated pneumonia (VAP) (Latenser, 2009). Strategies for the prevention of VAP such as elevation of the head of the bed to 30º, regular oral care and body position changes should be part of standard care in the ICU (Latenser, 2009). Physiotherapeutic interventions like therapeutic coughing, humidification of inhaled gases, chest physiotherapy, airway suctioning and early mobility are indicated to effect facilitation of the removal of retained secretions (see Section 6.8).
In patients with suspected carbon monoxide intoxication as a result of inhalation injury, the levels of carboxyhemoglobin are evaluated with arterial blood gas analysis. A level greater than 3% in non-smokers or 10% in smokers confirms the diagnosis (Dries and Endorf, 2013). Oxygen therapy at 100% is commenced in the form of a non-rebreathing oxygen mask or through an artificial airway to speed up elimination of carbon monoxide from the lungs. Hyperbaric oxygen therapy is often advocated to further enhance clearance of carbon monoxide, but outcomes from this therapy remain controversial (Dries and Endorf, 2013). Complications associated with hyperbaric oxygen include air embolism, barotrauma, tympanic membrane disruption and seizures (Dries and Endorf, 2013).
6.5.3.1.6. Pain management
Pain originates from various sources in patients with burn injury. Pain management for patients with burn injury therefore becomes quite complex. Pain originates from the site of injury as a direct result of injury to and stimulation of nociceptors in the dermis and epidermis (De Castro et al., 2013). Pain is also generated from the local inflammatory response to injury, which is activated a few minutes after injury. Numerous chemical irritants are released into the area and sensitise and stimulate the nociceptors. This leads to primary hyperalgesia, which means the injured area remains painful and sensitive to mechanical and thermal stimuli (De Castro et al., 2013). Secondary hyperalgesia develops in the tissues that surround the burn site. As the inflammatory response subsides over time, a change in pain quality is observed. Where nociceptors are destroyed as a result of severe burn injury, insensitivity to pain may be noted initially; however, neuropathic pain may develop in these areas as nerve tissue regenerates in a disorderly fashion. Neuropathic pain develops in over half of patients with severe burn injury and is chronic in nature (De Castro et al., 2013). Pain also originates from procedures such as placement of lines or cleaning of wounds. Effective pain management is crucial for the successful management of patients following burn injuries. Ineffective pain management may result in the patient distrusting the interdisciplinary team and has a negative impact on early patient rehabilitation. It may also lead to the development of psychiatric disorders such as depression and post-traumatic stress disorder (De Castro et al., 2013).
Patients may experience four patterns of pain; for example, background pain (constant pain at rest and during movement), breakthrough pain (episodes of intense and sudden pain), pain produced by procedures and postoperative pain (De Castro et al., 2013). During the first 24 hours following burn injury, analgesic therapy is administered, monitored and regularly adjusted as needed. The dose and type of analgesia given is dependent on the size of the burn, depth, patient age and the presence of other traumatic injuries (Alharbi et al., 2012). Background pain is usually managed in the acute phase, with a continuous infusion of opioids (with or without patient-controlled analgesia), oral long-term opioids, non-steroidal anti-inflammatory drugs and anxiolytics (De Castro et al., 2013). Procedural pain is managed with opioids (remifentanil, fentynal or alfentanil) and anaesthetics (ketamine). The pharmacological management of neuropathic pain is achieved through administration of opioids (tramadol), anticonvulsants (gabapentin) and antidepressants (amitriptyline) (De Castro et al., 2013). The reader is referred to Section 6.8.2 for information on the non-pharmacological management of pain in patients with burn injury.
6.5.3.2. Surgery
Dead tissue is an excellent medium for the growth of bacteria, so it needs to be removed as quickly and thoroughly as possible in patients who have sustained burn injury. Evidence shows that early burn wound excision (between days two and seven of admission) leads to decreased mortality and length of hospital stay in patients aged 30 years or younger (Kasten et al., 2011).
6.5.3.2.1. Debridement
Deep cleaning and removal of dead tissue and contaminants from burn wounds is called debridement. Some units make use of burns baths or shower the patient in the cubicle even in the ICU setting. Autolytic, enzymatic or surgical means can be used to perform debridement and are discussed below (Alharbi et al., 2012).
6.5.3.2.1.1. Autolytic debridement. This type of debridement is usually performed on more superficial burns, but also if the patient is unable to tolerate a more aggressive form of debridement (such as the elderly or those with co-morbidities). Dressings such as hydrogels or hydrocolloids (which are moist) are used to retain wound fluids and allow the body to get rid of dead tissue on its own. Autolytic debridement is not suitable for infected wounds but can be used in moist wounds. Wounds generally heal without grafting (Edwards, 2010).
6.5.3.2.1.4. Repeat debridement procedures. Flammable liquid burns, hot oil, electrical and chemical burns all have a high potential for becoming infected. It may be necessary to debride such wounds more than once to ensure proper cleansing of the wound bed in order to promote healing. This is especially important when preparing the burn wound for grafting. In reality the patient may have a debridement every 24 or 36 hours. With deep debridement there may be extensive bleeding, which has the potential to make the acutely ill patient even more unstable. The physiotherapist needs to be aware of this and be prepared to adjust their treatment accordingly. This is usually a temporary situation from which the patient generally recovers in 24 to 48 hours (Alharbi et al., 2012). There is usually blood on standby for the patient, as often a blood transfusion is necessary. Other complications associated with debridement are pain, infection and risk of removal of healthy tissue (Alharbi et al., 2012). Despite the possibility of complications, early wound closure by skin grafts after debridement has been shown to lead to significantly lower mortality rates (Church et al., 2006; Alharbi et al., 2012).
6.5.3.2.2. Escharotomy
Severely burnt tissue can be tense, firm and leathery in appearance. It is immobile, rigid and constrictive in nature. This type of tissue is called eschar. If eschar is circumferential around a limb or the thorax it can restrict movement, circulation or respiration. In this situation the eschar must be cut to prevent damage. The surgical cutting of eschar is called escharotomy. If escharotomy is necessary, it is usually quite evident soon after admission or within the first few hours. Escharotomy is usually a surgical emergency to prevent death of tissue or limb loss. If eschar is affecting the limbs, longitudinal incisions are generally used, starting, if possible, on unburned tissue, cutting through the eschar to expose the fatty tissue below and ending in unburned tissue. These incisions can be very extensive and in multiple sites simultaneously (Alharbi et al., 2012). Due to the amount of tension in the tissues, this longitudinal incision often widens substantially after the procedure. This is in direct proportion to the amount of pressure the tissues were under prior to the escharotomy being carried out. The site may require grafting at a later stage for skin closure.
Key Message
The physiotherapist should observe for signs such as peripheral cyanosis, reduced capillary refill, reduced limb temperature and weak or non-palpable pulses, which would indicate poor circulation to the extremities. In patients with circumferential thoracic burns, look out for signs of respiratory compromise such as tachypnea, dyspnea, decreased chest wall excursion and deteriorating arterial blood gas values. If any of these signs are present, the surgical team should be alerted.
6.5.3.2.3. Fasciotomy
Fasciotomy is a surgical procedure in which an incision is made in the skin that extends into the fascia to relieve pressure for suspected compartment syndrome, such as in the case of circumferential burns to the wrist (carpal tunnel syndrome), thigh or calf (Fig. 6.4). If necessary, it is usually required in the early stages of wound care. Compartment syndrome can be life or limb threatening.
After fasciotomy, limb movement can continue, with elevation of the part to reduce postoperative swelling. Maintenance of joint range of motion (ROM) and muscle length is crucial after fasciotomy; splinting of the joint is effective to maintain muscle length. The area in which the fasciotomy was performed might need to be grafted once the tissue swelling subsides (Alharbi et al., 2012).
6.5.3.3. Wound management
The main aims of burn wound management are to prevent wound infection and facilitate the closure of wounds. This can generally be achieved spontaneously in superficial burns. After any of the abovementioned surgical procedures, the open wound will require coverage. The various methods of wound closure are discussed below.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree