Fig. 2.1
Program development: key factors
To maintain a collaborative working environment, regularly scheduled interest group meetings provide a venue for teams to discuss operative successes and difficulties. During early program development, a realistic timeline should be constructed and enforced though the interest group. Efficient program dynamics offer a great source for resident training and the development of research projects. Community education also is important, and should be part of the institutional mission and commitment.
When developing any new program, it is important to inform and have support from the departmental chairperson. This helps solidify support during structured business plan development. It is important to collect and analyze continuously data related to increase patient referrals and hospital savings. Moreover, programs must develop a partnership with industry representatives early in the venture to provide the best negotiating position for reducing equipment and instrument costs. Non-capital expenses include robotic system service contracts as well as “fixed-use” instruments and disposable supplies (i.e. sterile instrument drapes). During program planning with hospital administrators it is important for all to have realistic goals regarding growth potential and early clinical outcomes.
Robotic Surgical Team Training
Team training remains the most important step in program development and should follow an objective-based curriculum that measures clinical outcomes (Fig. 2.2). During our Phase I and Phase II clinical trials, the FDA mandated institutional team training with a designated lead surgeon. In the United States, ECU was the initial system and procedure-training site. Surgical teams must include the console or operating surgeon, the patient-side surgeon/assistant, a lead scrub nurse, and a dedicated circulating nurse. Moreover, both a senior perfusionist and anesthesiologist should be trained with this group. Proficient robotic cardiac surgery requires that the surgeon have necessary premonitory skills to perform traditional operations with excellent results. The robotic system is simply a device that provides the least invasive cardiac access and good results are predicated upon a surgical abilities acquired previously. We recommended that early in program development that the console surgeon masters the role of the patient-side surgeon/assistant. This enables the console surgeon to trouble shoot instrument port placement and instrument exchanges, which enhances patient-side surgeon/assistant speed as well as helps resolve end-effector conflicts.
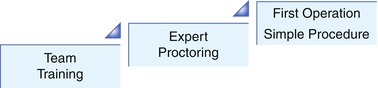
Fig. 2.2
Early robotic training: first operations
Training objectives for nurses and operating room staff are similar; however, they focus more on sterile draping, operating room arrangement, instrument care, and device maintenance. Our teams begin with “basic system training” that includes set-up, draping, and troubleshooting. Teams build upon their relationship with the preceptor/proctor and return to their home institutions to begin performing simple robotic procedures to reinforce learned objectives. Teams follow must follow both a carefully outlined clinical plan and timeline that is specific to their goals. After mastering these basic objectives, teams are advised to return to the training site for “advanced procedure specific training” (Fig. 2.3). Our training programs have been developed for all disciplines of surgery, including general surgery, gynecologic surgery, urologic surgery, thoracic surgery, and cardiac surgery [14]. The curriculum advancement levels may include case observations, didactic sessions, inanimate and live animal practice sessions, and fresh cadaver training (Tables 2.1 and 2.2). In many specialties, inanimate models can emulate the body habitus of live patients and allow practice with port and camera placement. Training sessions are intended to be interactive, and all involved are expected to contribute. For cardiac training, intact animal hearts provide life-like tissues for resecting tissue and suturing. Fresh cadavers provide hands-on training and provide the complexities associated with port placement and efficient access to internal structures. Since August 2000, over 500 surgical teams have completed the ECU training curriculum. This includes “basic system training” and “advanced procedure specific training.”
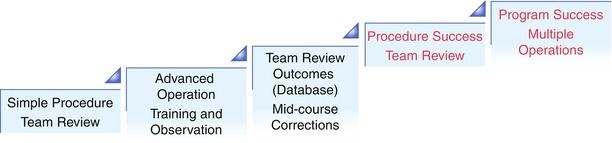
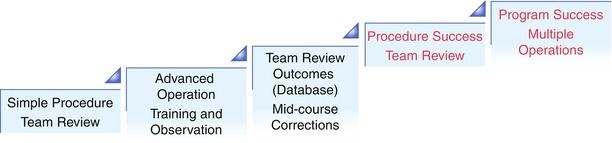
Fig. 2.3
Program advancement: complex operations
Table 2.1
Robotic system training
Objective-based curriculum |
|---|
System training |
A. Didactic overview |
Understand robotic vision and electronics |
Understand robotic instrumentation |
Understand common troubleshooting issues |
B. Inanimate laboratory |
Master robotic operative cart (draping and set-up) |
Master operative console controls
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|