The purpose of applying a high-pass filter is to attenuate low-frequency noise. This type of noise presents as baseline sway, which may hinder proper assessment of the electrocardiogram. Low-frequency noise is due primarily to slight movement of the electrodes on the skin, physicochemical skin-electrode changes, or body movement produced by breathing.
The American Heart Association in 2007 established the optimal cutoff for low-frequency filtering as 0.05 Hz, which may be extended to 0.67 Hz if linear-phase or zero-distortion filters are used. However, to achieve this, the linear phase filter order must be very high to filter the signal without modifying it, which involves a high computational cost. The order of a filter refers to filtering power. The higher the order, the more steeply it attenuates the undesired frequency band while preserving the desired frequency band. Kligfield and Okin showed that 62% of 256 electrocardiograms analyzed had higher cutoffs than recommended for high-pass filtering. Sometimes, the low-frequency components of the electrocardiogram, such as the ST segment, may be distorted by this type of filter, leading to diagnostic errors. The use of traditional analog filters with a cutoff frequency of 0.5 Hz can cause such artifacts.
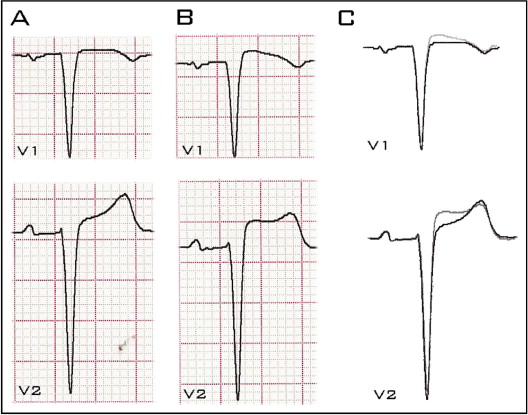
This alteration, although generally dependent on the baseline electrocardiogram, is more common in the right precordial leads. For such important diseases such as Brugada syndrome, for which the diagnosis is based on the signals from these leads, correct recording is essential to prevent misdiagnosis and unnecessary therapeutic measures. The diagnostic electrocardiographic pattern of this genetic heart disease, called the type 1 pattern, is characterized by concave morphology with high takeoff of the QRS complex ≥0.2 mV with respect to the baseline in the right precordial leads (V 1 to V 3 ), accompanied by a negative T wave. The type 2 pattern presents saddleback morphology, with minimum ST-segment elevation (>0.05 mV), high takeoff of r′ (which does not necessarily coincide with the J point) ≥0.2 mV in the right precordial leads, followed by positive or isobiphasic T waves. The type 2 pattern needs pharmacologic provocation tests to confirm the diagnosis of the disease.
Figure 1 shows leads V 1 and V 2 in a 55-year-old woman with hypertension, after applying the standard high-pass filter of 0.05 Hz and a nonstandard high-pass filter of 0.5 Hz. With the nonstandard high-pass filter, the ST segment is distorted, with coved type morphology in lead V 1 followed by a negative T wave, but with ST-segment elevation ≤2 (0.137 mV). In contrast, ST-segment elevation in lead V 2 is >2 mm (0.325 mV).