Fig. 24.1
ECG performed at hospital admission
Sinus rhythm, heart rate 95 bpm, normal atrioventricular conduction (PQ 150 ms), cardiac electrical axis +60°, and coved-type ST-segment elevation about 4 mm, followed by a negative T wave in V1 and an ST-segment elevation with a saddleback appearance in V2 with a biphasic T wave. QTc 450 ms
Echocardiography
Normal dimension of both atria (LA diameter M-mode = 30 mm, LA area 4 c = 16 cm2, RA area 4 c = 12 cm2). Normal size and wall thickness of the left ventricle (iLVEDV 61 ml/m2) which shows a preserved systolic function (ejection fraction with Simpson’s method 0.61). Normal size and global function of the right ventricle (TAPSE 24 mm)
Normal morphology of the cardiac valves; mild tricuspid regurgitation and normal systolic pressure gradient (PASP = 20 mmHg)
The inferior vena cava has a normal size (16 mm) and physiological collapsing during inspiration.
Absence of pericardial effusion
Normal diastolic pattern without increased filling pressure (E/A 0.8, E/E’ 3.7, E dec time 193 m/s).
Conclusion
There are normal echocardiography findings for a 35-year-old man.
Routine Laboratory Tests
Complete blood count: mild leukocytosis (13.3 × 10^3/mmc)
Cholesterol (total, HDL, LDL) and TG: normal
Hepatic function (GOT, GPT, γ–GT, ALP, total bilirubin, direct and indirect): normal
Thyroid function (TSH, FT3, FT4): normal
Renal function (creatinine, BUN): normal
Electrolytes (Na +, K +, Ca ++, Mg ++, Cl −): normal
Fasting blood glucose: 94 m/dl (5.22 mmol/l)
Troponin I–hs: 0.006 ng/ml (n.v <0.055 ng/ml)
Inflammation index: VES 30 mm/h (n.v <27 mm/h) and CRP 0.9 mg/dl (n.v <0.6 ng/ml)
What Are the Possible Causes of Cardiac Syncope?
Arrhythmia
Bradycardia
Sinus node dysfunction (including bradycardia/tachycardia syndrome)
Atrioventricular conduction system disease (AV blocks)
Implanted device malfunction
Tachycardia
Supraventricular arrhythmias
Ventricular arrhythmias (idiopathic, secondary to structural heart disease or to channelopathies)
Drug-induced bradycardia and tachyarrhythmias
Structural Disease
Cardiac
Cardiac valvular disease
Acute myocardial infarction/ischemia
Idiopathic dilated cardiomyopathy
Hypertrophic cardiomyopathy
Arrhythmogenic right ventricular dysplasia (ARVD)
Cardiac masses
Pericardial disease/tamponade
Congenital anomalies of coronary arteries
Prosthetic valves dysfunction
Others
Pulmonary embolism
Acute aortic dissection
Pulmonary hypertension
A precise and careful medical history is the key to achieve a correct etiologic diagnosis of syncope. Thanks to this we have already removed some possible causes of syncope (orthostatic hypotension, reflex, and neurological syncope) and epilepsy (we executed an electroencephalography which did not show any abnormality). So we focused on the most likely cardiac causes.
The patient did not show any metabolic disorder at the laboratory tests or physical signs of intoxication. He did not assume any drug as possible cause of arrhythmias.
Physical exam together with ECG and echocardiography did exclude a structural heart disease together with pulmonary embolism and acute aortic dissection.
A possible arrhythmic origin seemed to us to be the most likely cause of this syncope. During hospitalization, the patient never showed bradycardia or paroxystic atrioventricular block of different grades. At ECG, the repolarization pattern did show a typical Brugada type 1 pattern with a coved ST-segment elevation ≥2 mm and a negative T wave in V1. The febrile state during which the ECG has been recorded could have unmasked the Brugada pattern, because the previous ECGs have been described to be normal. It is well known that the typical Brugada pattern may vary according to body temperature, autonomic tone, and also drug intake. This ECG pattern is described to be associated with risks of ventricular tachyarrhythmias (torsades de pointes or ventricular fibrillation mainly), as possible cause of syncope or sudden cardiac death.
Final diagnosis
Brugada syndrome (syncope in young man with Brugada type 1 pattern at the ECG)
An electrophysiological study was specifically not indicated in this particular situation because the patient was “symptomatic” for unexplained syncope and there was a familiar example of sudden death at young age.
Therefore, we implanted a subcutaneous cardioverter defibrillator (S-ICD) in primary prevention. We chose a subcutaneous device instead of an intravenous one because sudden death in Brugada syndrome is due to polymorphic ventricular tachycardia (e.g., torsades de pointes) or ventricular fibrillation (VF) that did not required anti-tachycardial pacing (ATP) but only defibrillation. Moreover, our patient was young and did not require cardiac pacing. Finally, the subcutaneous device implantation is less invasive (device lead is extrathoracic), and an eventual explant (e.g., for infection) is easier compared to an intravenous device.
Quinidine has been reported as a possible pharmacological aid, but the existing data are not so numerically sufficient to be considered a lifesaving therapy.
24.2 Brugada Syndrome
Definition
Pattern Versus Syndrome
Brugada pattern (BrP) and Brugada syndrome (BrS) differ each other for the presence or absence of symptoms:
Brugada pattern: patients with typical ECG features who are asymptomatic and have no other clinical criteria
Brugada syndrome: patients with typical ECG features who have experienced sudden cardiac arrest (SCA), sustained ventricular tachyarrhythmia, or unexplained syncope
ECG Patterns
Initial classification considered three main ECG patterns [4], but in the last consensus, this classification was changed unifying types 2 and 3 into a unique pattern (Fig. 24.2) [5]:
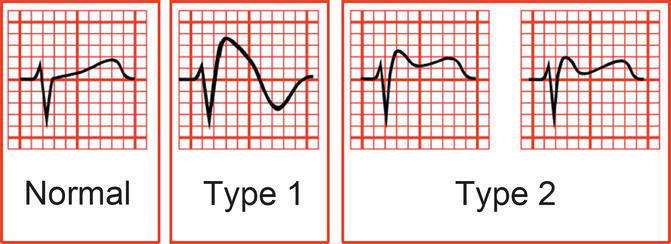
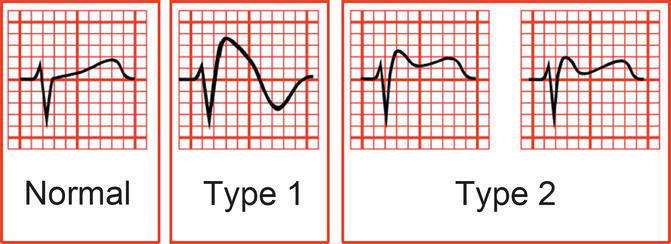
Fig. 24.2
Current electrocardiographic classification of Brugada pattern
Type 1 (classic Brugada type 1 ECG): ST-segment elevation (≥2 mm) descends with an upward convexity to an inverted T wave in at least one right precordial chest lead (V1–V2). This is referred to as the “coved type.”
Type 2 (combined from the original designation of type 2 and 3 patterns): ST segment has a “saddleback” ST–T wave configuration, in which the elevated ST segment descends toward the baseline and then rises again to an upright or biphasic T wave.
Moving the right precordial chest leads (V1–V2) up to the second or third intercostal space may increase the sensitivity of detecting these abnormalities [6]. This may be crucial because those with a type 1 Brugada pattern only in high chest leads seem to have a similar rate of cardiac events during >1 year of follow-up as those with type 1 Brugada ECG in standard position [7]. With that single ECG recording, it is likely to diagnose a Brugada type 1 without referring to a drug challenge (see below) in a high percentage of patients.
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


