Fig. 4.1
Determining procedural unit space needs
General Requirements of Procedural Area
Hospital procedural suites must adhere to many regulatory bodies including but not limited to internal and external groups. An interventional pulmonology advanced procedure suite may be subject to the control of some of these:
1.
Internal Regulatory Groups
(a)
Life safety
(b)
Infection control
(c)
Radiation safety
(d)
Invasive procedures committee
2.
External Regulatory Groups
(a)
Department of Public Health (DPH)
(b)
The Joint Commission (TJC)
(c)
Centers for Medicare and Medicaid Services (CMS)
General Information that Should Be Available Regarding the Procedural Unit
Scope of services provided
List of physicians approved to perform specific procedures
Qualifications of staff support
Policy and procedures manual
Spaces Required for Procedural Unit Design
1.
Reception
2.
Preop and recovery
3.
Procedure
4.
Nursing workstation
5.
Physician workstation
6.
Storage
7.
Reprocessing
8.
Other?
Flow of Patients, Staff, and Equipment
Before we discuss the actual procedure spaces, we should consider the optimum flow through the unit for patients, staff, and equipment. In a perfect world, patients would experience their procedure by stopping at the reception area for a very short time, answering a couple of simple questions, and proceed to the procedure suite with no interruptions or delays and with no exposure to anything else going on in the unit that does not have to do with their own care. So, at least to address the last part, in a perfect world, we might have a procedural unit that has separate flows for the patient, staff, and equipment.
Patient flow may be designed to have patients begin their experience at the reception center and complete the required administrative duties, while family members are escorted to a nearby waiting area. From there, the patient is brought to the preoperative area in privacy through a corridor that is dedicated for patient transport only, unexposed to other patients or family sitting in waiting areas or equipment being rolled by the staff. Then, through the same hall to the procedure suite for their case and after, brought back to the recovery area in privacy to their bay to recover until it is time to be discharged. The patient is then reunited with family via this separate corridor to either the reception or waiting area.
Staff would use a more common hall to flow from their nursing station to the area that they are responsible for, whether to care for patients in the preop area, the procedure suite, or recovery. On this common side would also house the physician workroom and storage areas for nursing supplies and technical equipment. This hall would by its nature be much busier than the private hall used to escort patients. Nurses might be moving from one area to another and technical staff shuffling equipment and supplies to and from the storage, preop, recovery, procedure, and reprocessing areas (Fig. 4.2).
Fig. 4.2
Flow of patients, staff, and equipment
Realistically, space restrictions and funding may not allow this ideal flow to occur. Hopefully, there will be some middle ground that will be found to allow minimum exposure to the workings of the procedure unit for patients while providing the staff with the most efficient way to perform their roles. This means providing storage areas that are in proximity for nursing supplies to the areas that need them and other areas for storage of technical equipment that does not require movement over large distances.
Procedural Unit Requirements
1.
Reception Area to Greet Patients
(a)
Allows for administrative responsibilities to be completed/registration verified
(b)
Provides area where family members are directed toward waiting area
2.
Preop and Recovery
(a)
Number of beds required depends upon number and utility of procedural rooms.
(b)
Staff requirements depend upon above and practice model used (dedicated staff for this area vs. same staff used to prep/recover and assist in procedure).
(c)
Requires a private area for outpatients to change from street clothes to hospital garments.
(d)
Necessary equipment for area includes hemodynamic monitoring which should be flexible (modular) to adjust for acuity of patient served.
(e)
Isolation room with negative airflow for potential of infectious airborne disease transmission.
(f)
There are minimum standards for room sizes but must consider occasional equipment that may need to be placed there (x-ray, emergency equipment in event of cardiac arrest).
(g)
Need to consider in the design the use of fixed walls for privacy vs. curtains which offer flexibility in their use. We have found that the combination of fixed walls on the side and a curtain across the front provides the advantages of both.
(h)
Consider flexibility in cabinet design for the ease of restocking should product selection change over time. Also the use of portable storage carts for nursing supplies allows for carts to be replaced in there entirety and restocked at a location that does not interfere with patient care (Fig. 4.4).
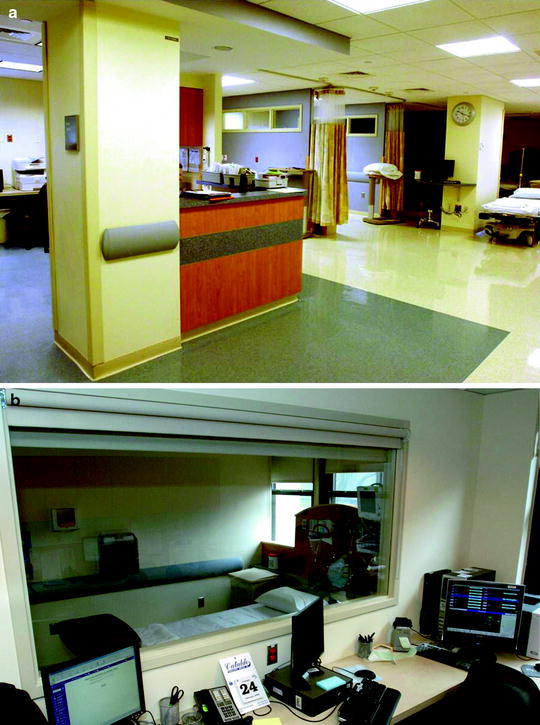
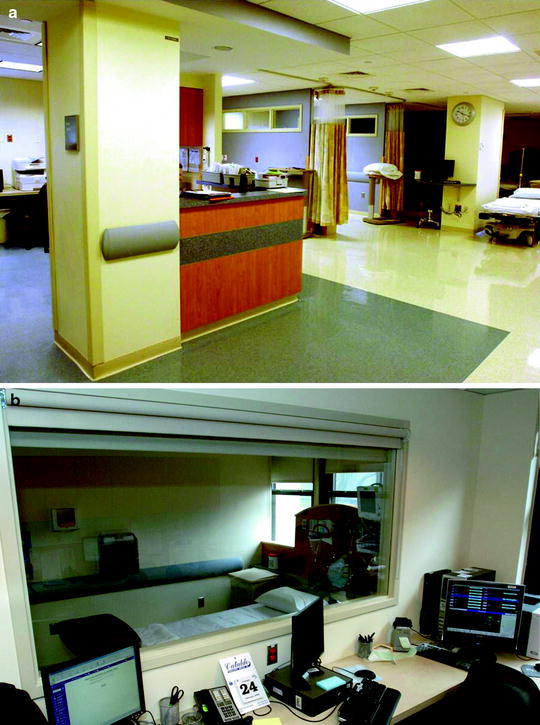
Fig. 4.4
(a) Nursing workstation centered around preop and recovery and (b) view of isolation room from nursing station
3.
Procedure Space
Before design plans can be considered, one must decide upon how the room will function. For instance, the location of medical gas lines in the room cannot be determined until you know where the patient will be positioned in the room. The architectural team cannot proceed with their drawings until the clinician makes this decision. You do not want to leave these decisions up to someone else and be left in a situation that you had control over but decided not to act upon. Too many times, a standard cookie-cutter model is selected, and the end users are left tripping over gas lines, extension cords, and video cables that were not placed in the best locations.
Therefore, the key to this space is the location of the patient bed with regard to movement into and out of the room; the flow of staff during the procedure as well as the required movement of equipment in and around the patient after patient is on the procedure bed.
Considering that there will probably be only one door used to move the patient to and from the room, then this area from the door to the procedure bed should be kept free of any permanent fixtures. I also think it is very helpful to be able to see the operator from the entrance to the room. This allows for easier communication and may allow for a sense of the progress of the procedure.
Given the above information, I believe it makes the most logical sense to locate the head of the bed toward the left hand wall as one would look into the room. Because bronchoscopy equipment connects to their processors and light sources on the left side, then any booms incorporated into the design to hold this hardware need to be positioned on this side of the patient. If the patients’ location was reversed and the head was at the right hand with the feet facing the left as you looked into the room, then the boom used to house the processors and light sources would obstruct the entrance to the room, and visualization of the operator would be compromised.
If one wanted to locate the head of the patient at the rear wall with feet facing the entrance to the room, then the boom (or booms) for the video monitors would obstruct the view and may be a bit more obstructive moving the patient. We have found that locating the patients head toward the left hand wall works best for most of our applications. But equally important in the design is to have the flexibility to modify the locations of these booms for different applications. The logistical flow of staff positioning and the determination of equipment locations including booms all hinge upon how you decide to position the patient for their procedure.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



