Fig. 11.1
Chest radiograph in 1-year-old child, showing cardiomegaly and pulmonary venous congestion
In view of the abnormal chest radiograph and ECG, cardiac review and echocardiogram were arranged. Echocardiogram showed a normally connected heart. The right atrium and right ventricle were dilated, with mild tricuspid valve regurgitation giving an estimated right ventricular pressure of 50 mmHg by continuous-wave Doppler interrogation. There was no evidence of right ventricular outflow tract obstruction; the branch pulmonary arteries were confluent and unobstructed, the left pulmonary artery appearing smaller than the right. Flow was seen returning to the left atrium from all four pulmonary veins however in all but the right lower pulmonary vein, the flow was turbulent on colour-flow. Pulsed-wave Doppler interrogation showed high-velocity flow signal (2 m/s) not returning to the baseline. There were no intra-cardiac shunts.
In view of the findings on echocardiogram, pulmonary vein stenosis was suspected and cardiac catheterisation performed. This showed pulmonary hypertension with the pulmonary pressure at two-thirds of systemic blood pressure. There was a gradient of 18–20 mmHg across the left upper, left lower and right upper pulmonary veins. Angiography showed discrete narrowing of these three vessels as they entered the left atrium (Fig. 11.2). The distal veins were of normal size. The child subsequently underwent repeated catheter interventions to balloon dilate the stenoses with conventional and cutting balloons and obtained good symptomatic relief.
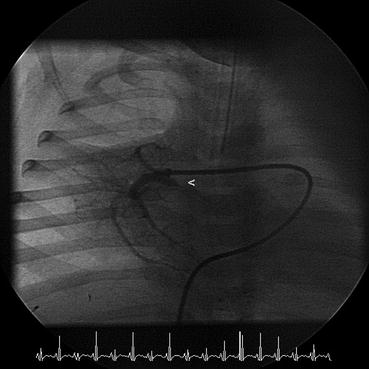
Fig. 11.2
Angiogram showing discrete right upper pulmonary vein stenosis (arrow)
Discussion
This case highlights the importance of assessing the pulmonary veins in infants that have chronic lung disease of prematurity but whose respiratory symptoms are more severe than would be expected from the degree of prematurity and early course.
Individual stenosis of one or more of the pulmonary veins was first described by Reye in 1951 in an 8-year-old girl with normal intra-cardiac anatomy. The lower pulmonary veins were stenotic, the left upper pulmonary vein was atretic and the right upper pulmonary vein ended blindly. The girl died of heart failure.
Pulmonary vein stenosis is rare, with two main categories found in children:
1.
Isolated pulmonary vein stenosis in the setting of a normally connected heart;
2.
Pulmonary vein stenosis in association with other forms of congenital heart disease and where the pulmonary veins return directly to the morphological left atrium. The incidence of associated cardiac defects is reported to range from 30 % to 80 %.
In 1988 Fong described three types of stenosis: bilateral tubular hypoplasia extending from the venoatrial junction for a variable length, intimal hourglass constriction at the venoatrial junction, and bilateral multiple short pulmonary veins that are hypoplastic for their entire extra-pulmonary course. Serial angiography has documented progression of disease with a discrete stenosis progressing to tubular and then more generalised narrowing. In some cases, the vein can became critically stenosed or atretic. Collateral pulmonary venous vessels may form, diverting pulmonary venous blood to either the systemic circulation or other lesser affected lobes of the ipsilateral pulmonary venous circulation.
The pathological mechanisms responsible for pulmonary vein stenosis remain unclear. Histological studies have shown a variable manifestation of intimal and medial interstitial fibromuscular proliferation, together with fibrotic displacement of the muscle bundles in the venous wall. This eventually results in occlusion of the lumen of one or more of the pulmonary veins connecting the lungs to the left atrium. Most commonly, the thickening of intimal tissue begins at the junction of the left atrium and pulmonary vein; the narrowing then extends outwards along the pulmonary vein towards the hilum of the lung.
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


