Bradyarrhythmias and Pacing
James V. Freeman
Paul J. Wang
BACKGROUND
Bradyarrhythmias result from abnormalities of sinus node function or A-V conduction. In this chapter we review the initial recognition, triage, acute management, and definitive therapy for the bradyarrhythmias.
DEFINITIONS
Bradycardia
Bradycardia is defined as a ventricular heart rate <60 beats per minute (bpm), and sinus bradycardia exists when each QRS complex is preceded by a P wave of sinus node origin on the electrocardiogram (ECG).
Sinus Node Dysfunction
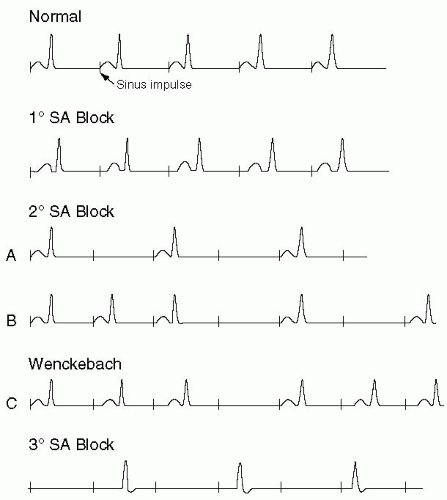
Sinoatrial blocks: Sinoatrial (S-A) blocks are uncommon and occur when there is disturbance of the conduction of the electrical impulse from the heart’s normal pacemaker, the S-A node, to the surrounding atrium. (See Figure 5-1.) The severity of dysfunction can vary widely and there are many ECG findings associated with S-A blocks (also called S-A exit blocks).1 The S-A blocks can be categorized as first, second, and third degree based on the characteristics of the conduction disturbance.
First Degree
In first-degree S-A block, there is an increased time for the S-A node’s impulse to reach and depolarize the rest of the atrium and form a P wave on ECG (Figure 5-1). There are no abnormalities seen on the 12-lead tracing with first-degree S-A block because impulse origination from the S-A node still produces a normal P wave on the 12-lead ECG.2
Second Degree
Type I (Wenkebach): In second-degree S-A block type I, there is a progressively increasing interval for each S-A nodal impulse to depolarize the atrial myocardium and produce a P wave on ECG (Figure 5-1). This
interval continues to lengthen until the S-A node’s impulse does not depolarize the atrium at all, which is manifested on ECG by a gradual shortening of the P-P interval with an eventual dropping of a P wave. It can be recognized by grouped beatings of the P waves, with sinus pauses.
interval continues to lengthen until the S-A node’s impulse does not depolarize the atrium at all, which is manifested on ECG by a gradual shortening of the P-P interval with an eventual dropping of a P wave. It can be recognized by grouped beatings of the P waves, with sinus pauses.
Type II: In second-degree S-A block type II, there is a fixed interval between the S-A node impulse and the depolarization of the atrium with an intermittent S-A nodal impulse that fails to conduct to the atrium (Figure 5-1). This manifests on ECG as a dropped P wave with a P-P interval surrounding the pause that is two to four times the length of the baseline P-P interval.3
Second-degree S-A Block with 2:1 Conduction
In second-degree S-A block with 2:1 conduction, every other impulse from the S-A node causes atrial depolarization while the other is dropped. It is impossible to differentiate this from sinus bradycardia on ECG unless the beginning or termination of the S-A block is recorded, in which case it manifests as a distinct halving (beginning) or doubling (termination) of the baseline heart rate.
Third Degree
In third-degree S-A block, none of the S-A nodal impulses depolarize the atrium, which appears on ECG as either atrial stand-still or P waves retrogradely conducted from a junctional rhythm (Figure 5-1). Sometimes there can be a long pause on the ECG until a normal sinus rhythm is resumed, which can be difficult to distinguish from sinus pause or arrest due to abnormalities of sinus impulse formation.
Sinus pause/sinus arrest: Sinus pause and sinus arrest are characterized by the failure of the S-A node to form an impulse, manifesting on the ECG as a sinus pause of varying length.1 Some sinus pauses follow the spontaneous termination of atrial fibrillation because of the overdrive suppression of the sinus node.
Sick sinus syndrome: Sick sinus syndrome includes a range of S-A node dysfunction that includes inappropriate sinus bradycardia, sinus arrhythmia, sinus pause/arrest, S-A block, A-V junctional (escape) rhythm, and the tachycardia-bradycardia syndrome (covered in the tachyarrhythmias chapter).4
Atrioventricular Conduction Dysfunction
Atrioventricular block: In atrioventricular block, electrical conduction is disturbed between the atrium and the ventricle. As with S-A blocks, A-V blocks are categorized into first-, second-, and third-degree blocks based on the characteristics of the conduction disturbance.
First Degree
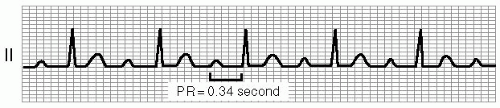
First-degree A-V block is defined as a prolonged P-R interval, greater than 200 milliseconds, which remains constant. (See Figure 5-2.) On ECG, the P wave and QRS complex have normal morphology, and a P wave precedes each QRS complex. The lengthening of the P-R interval results from a conduction delay from within the atrium, the A-V node, or the His-Purkinje system.
Second Degree
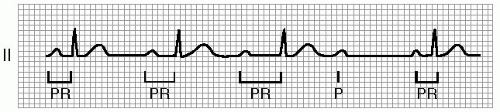
Mobitz Type I (Wenckebach): Second-degree A-V block Mobitz type I is characterized by a P-R interval that lengthens progressively until an impulse fails to conduct to the ventricles and a QRS complex is dropped. (See Figure 5-3.) This block usually occurs at the level of the A-V node and above the His bundle. The patient’s QRS complex is usually narrow (less than or equal to 120 milliseconds) although there may be a concomitant lower conduction disturbance leading to bundle branch block. On ECG, the P-R interval lengthens as the R-R interval shortens, and the R-R interval that contains the dropped beat is less than the sum of two of the shortest R-R intervals seen on the ECG. Also, on the ECG rhythm strip, a grouping of beats can be seen.2,7 A consistent and diagnostic feature of Wenkebach is that the PR interval after the dropped beat is shorter than those immediately preceding the AV block.
Mobitz Type II: Second-degree A-V block Mobitz type II is defined by a constant P-R interval that may be normal or prolonged (>0.20 s) and periodic abrupt failure of the atrial impulse to conduct to the ventricles. (See Figure 5-4.) The QRS complex is nearly always widened, since development of Mobitz Type II block almost always follows development of bundle branch block. This rule is so strong that apparently abrupt A-V block without measurable preceding P-R prolongation in a patient with a narrow QRS complex is more likely to be at the level of the A-V node and thus be an atypical Mobitz Type I A-V block rather than actually representing Mobitz Type II A-V block.
Second-degree A-V block with 2:1 conduction: In second-degree A-V block with 2:1 conduction, every other QRS complex is dropped, causing two P waves for each QRS complex. Since there is no way to determine on ECG if the P-R interval lengthens before the dropped QRS complex, the primary method of determining the level of the block is examining the QRS width. If the QRS complex is narrow, the 2:1 A-V block almost certainly exists at the level of the A-V node. If the QRS complex is widened, the level of the block could be either at the level of the A-V node or infrahisian.
Third Degree
Third-degree A-V block, or complete heart block, occurs when no electrical impulses from the atria conduct through to the ventricles. (See Figure 5-5.) The atria and ventricles thus depolarize and beat independently. An escape rhythm originating from the A-V junction or the ventricles below the level of the block maintains the ventricular rate. In third-degree A-V block, the P waves march out regularly and independently of the regular ventricular depolarization (QRS complexes). The atrial rate is generally faster than the ventricular rate, because the latter is an escape rhythm, and the ventricular rate can vary depending upon where the ventricular depolarization originates.1 In some cases, the P-P interval encompassing the escape QRS complex may be shorter than otherwise in the tracing, a phenomenon called “ventriculophasic phenomenon.”
Escape Rhythms
When electrical impulses fail to conduct to the ventricles from the atria, whether due to S-A block or A-V block, ventricular depolarization can originate from more distal locations in the conduction system that also possess automaticity. Generally the more distal the site of impulse origination, the slower the rate generated. The ventricular rate is generally 40 to 60 bpm with a narrow QRS complex when it is driven by a junctional pacemaker within the A-V node or above the His bundle. A ventricular pacemaker is characterized by a widened QRS and a rate less than 40 bpm (except an accelerated idioventricular rhythm with a rate >40 bpm). These rhythms originate in the His-Purkinje system and are usually associated with a poorer prognosis.7 If no escape impulse is generated, then the result is an asystolic arrest.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree