26 Bradyarrhythmias
Etiology and Pathogenesis
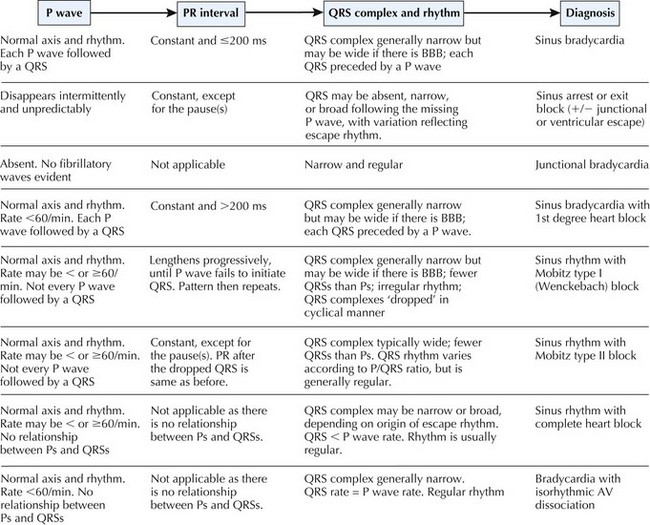
It is simplest to regard bradycardia as a manifestation of quite a few noncardiac and cardiac causes (Box 26-1). When due to cardiac causes, bradycardia may be further categorized according to the site(s) of delay or block within the cardiac conduction system: the sinus node, the atrioventricular (AV) node, the bundle of His, and the bundle branches/Purkinje network. Conditions that alter the autonomic inputs to the sinus and AV nodes, diseases that interrupt the blood supply or the electrophysiology of these structures, or drugs that modify the ionic properties of conductive cardiomyocytes can all lead to bradycardia. By far, sinus node dysfunction and AV block (either nodal or infranodal) account for the majority of clinically significant bradyarrhythmias. Reflex-mediated syncope (subtypes of which retard the heart to varying extents) is described in Chapter 31. In this chapter, we focus on the cardiac causes of bradyarrhythmia (Fig. 26-1).
Box 26-1 Causes of Bradycardia
Sinus Node Dysfunction
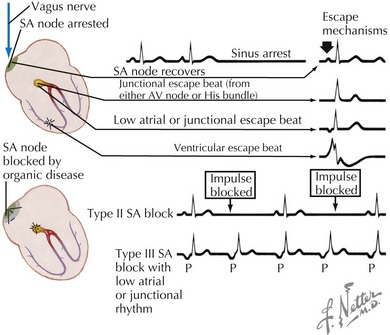
Sinus Arrest
In sinus arrest, the sinus node fails to depolarize, resulting in an atrial pause. The P-P interval encompassing this pause is not an exact multiple of the basic P-P interval (Fig. 26-2), indicating that the abnormality is not simply a blocked sinus impulse. Sinus pauses exceeding 3 seconds are highly suggestive of SND. Conversely, it is not uncommon to encounter asymptomatic sinus pauses of 2 seconds or less in the well-conditioned athlete or even in normal individuals.
Sinoatrial Exit Block
In SA exit block, the SA node does fire automatically, but the impulse either fails to propagate into the atria (because of a conduction barrier within or around the SA node) or does so after a delay. In the former scenario, the atria are not depolarized, and the expected P wave fails to materialize. Like AV block, SA exit block can be graded as first, second, or third degree, with second-degree SA block further classified into Mobitz type I (Wenckebach) or Mobitz type II. Type II SA block is the most common. In this circumstance, the failure of the sinus impulse to exit the node is intermittent, and the atrial pause produced is an exact multiple of the prevailing P-P interval (see Fig. 26-2). In Wenckebach SA block, the P-P interval shortens progressively before the dropped beat. With third-degree SA block, the ECG only records the escape rhythm (see Fig. 26-2). If no P waves are present, it is impossible to distinguish (by ECG criteria alone) third-degree SA block from prolonged sinus arrest. Clinically, this distinction is not important; what matters is whether the patient is symptomatic. In first-degree SA block, there is an abnormally long interval between the sinus impulse and atrial capture. This condition, too, cannot be diagnosed from the surface ECG.
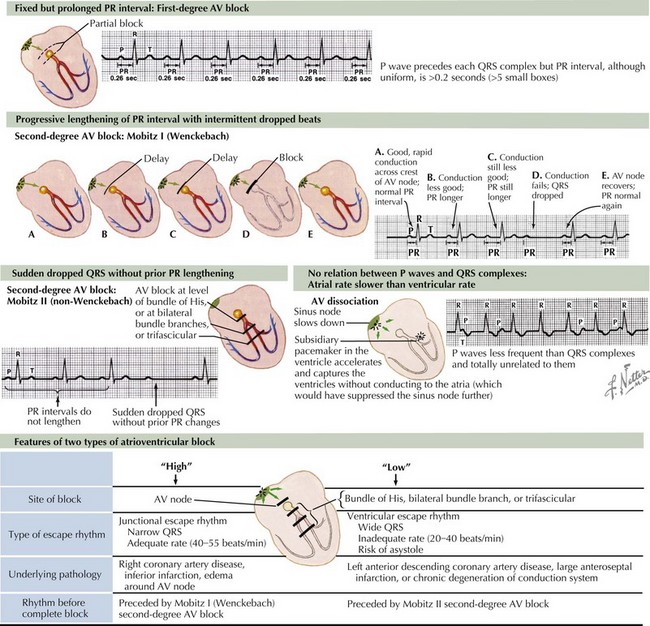
Atrioventricular Block
AV block occurs when there is a delay or nonconduction of an atrial impulse to the ventricles. It can result from normal or abnormal cardiac electrophysiology, can be transient (e.g., following inferior myocardial infarction) or permanent, and can occur at any or several levels of the AV node–His–Purkinje axis. Based on the ECG, AV block may be graded as first, second, or third degree, depending on whether AV conduction is merely delayed, intermittently blocked, or completely blocked. This classification has clinical implications, because the site of AV block (and hence the patient’s prognosis) may be inferred with reasonable accuracy from the rhythm. It is important to note that when the atria and ventricles beat independently of each other, AV dissociation occurs (Fig. 26-3). In clinical parlance, this term is applied when the ventricular rate, driven by a subsidiary pacemaker, is the same or faster than the atrial rate. Because of this, the ventricles are functionally refractory to the slower atrial impulses.
First-Degree Atrioventricular Block
First-degree AV block is defined as a PR interval greater than 0.2 seconds. Each P wave is followed, after a constant delay, by a QRS complex (see Fig. 26-3). In that sense, the label “AV block” is incorrect, because no P waves are actually “blocked.” Because the PR interval reflects the time between the earliest recorded atrial activity and the onset of ventricular depolarization, first-degree AV block can arise from conduction delay in the AV node (the commonest mechanism), abnormally slow intra-atrial conduction (less common), or, even less often, His-Purkinje disease (in which case the evoked QRS complex will be broad). In individuals with dual AV node physiology, transient, abrupt, first-degree AV block may be seen when antegrade conduction jumps from the fast pathway (used normally) to the slow pathway (see Chapter 27
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree