Brachial Artery Embolectomy
Chinenye Iwuchukwu
Vivian Gahtan
Indications
Acute limb ischemia of the upper extremities accounts for 5% of all cases of limb ischemia and less than 3% of all interventions for critical limb ischemia. The unique structure and layout of the vasculature in the upper extremity allows for collateral blood flow and tissue loss with an occlusion of one of the vessels being rare. The brachial artery is the most common location of occlusion in the upper extremity. Causes of acute upper extremity limb ischemia include:
Thromboembolic events (e.g., atrial fibrillation, hypercoagulable states)
Iatrogenic injury (e.g., brachial artery catheterization)
Traumatic injury (e.g., elbow dislocation)
Patients with brachial artery occlusion generally have diminished or absent pulses in the affected limb. They can present with the classic signs of acute limb ischemia: pain, pulselessness, pallor, parasthesias, and paralysis. In the setting of upper extremity ischemia, a window of opportunity for nonsurgical management exists, especially in cases where there is no evidence of a threatened limb and a short duration of symptoms. Nonsurgical treatment options include endovascular therapies such as thrombolysis and mechanical thromboembolectomy; however, these techniques are less commonly performed in the upper extremity as compared to the lower extremity. While there has been reported success, a failure of these procedures exists resulting in the need for surgical thromboembolectomy. Thrombolysis, if feasible, is preferred when there is distal thrombosis involving the hand. Anticoagulation alone in a patient with a brachial artery occlusion can be considered in an unstable patient or one with a short life expectancy (due to major comorbidities), who has wrist Doppler signals and intact motor function.
Indications for surgical thromboembolectomy include:
Threatened limb
Abnormal hand perfusion in a stable patient
Nonresolution after a course of lysis
Contraindications
There are a few true contraindications to performing thromboembolectomy in patients with brachial artery occlusion. For example, in the case of occlusion secondary to blunt trauma, it is likely that the vessel is injured and may require replacement with a bypass and thrombectomy alone may not be appropriate.
Early and focused evaluation of patients with a concern for acute limb ischemia is important for effective assessment and therapeutic planning. A complete history and physical must be performed. The history should include duration of symptoms, prior similar events and treatments, history of cardiac arrhythmias, alteration in medical regimens (e.g., holding warfarin for an upcoming procedure), prior upper extremity procedures, upper extremity disability, known arterial occlusive disease and whether there are known asymmetric pressures. The physical examination should include a description of appearance, pulse examination, and any sensory or motor deficits. Duplex ultrasound should be obtained to delineate the location of the occlusion and assist with operative planning. If the axillary pulse is absent, a computed tomography angiogram should be considered and can be helpful in the case of concurrent occlusive disease. Because the successful treatment of limb ischemia is time sensitive, the full assessment of the etiology of the occlusion may be delayed until after the procedure. Delays are reasonable for unstable cardiac arrhythmias that may need to be addressed at least for short-term stabilization.
Positioning
The patient is placed in the supine position with the operative upper extremity out on the table to better maximize working space for the surgeon and assistant (Fig. 6.1).
Technique
The approach to exposure of the brachial artery depends on the location of the clot. Occlusion in the proximal part of the brachial artery is generally approached through a proximal incision and an occlusion in the distal brachial artery or at the bifurcation and beyond, is better suited with a more distal incision in order to sufficiently expose the brachial bifurcation.
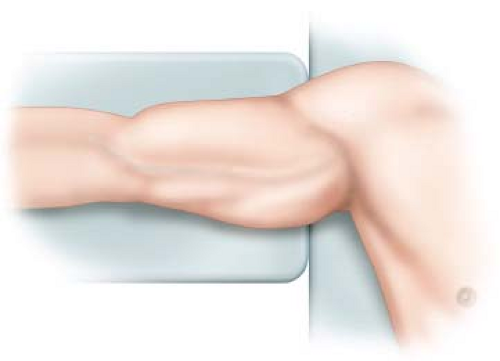 Figure 6.1 Positioning of the arm for surgery with the patient supine and the arm extended to 90 degrees. |
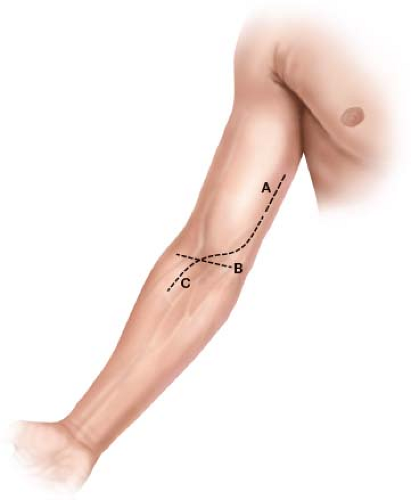 Figure 6.2 Incisions that can be used for the procedure depending on location of the clot. A: Proximal incision which is longitudinal. B: Transverse incision. C:
Get Clinical Tree app for offline access
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree


|