Fig. 1
A massive area of opacification involving the upper and middle zones of the right lung, enlargement of the entire cardiac silhouette, an elongated and sclerotic aorta. Free intraabdominal air visible under the diaphragm

Fig. 2
An area of consolidation with an air bronchogram in the upper lobe of the right lung. The right upper lobe bronchus gradually narrows towards the described lesions
Flexible bronchoscopy revealed a cauliflower-like lesion at the origin of the right upper lobe bronchus. The lesion contained necrotic masses, occluded approximately 90 % of the bronchial lumen and a purulent discharge was oozing from underneath the lesion (Fig. 3). The bronchoscopy also revealed a macroscopically changed (infiltrated) upper-lobe carina. The histopathological examination of the tissue samples collected during bronchoscopy revealed ‘chronic bronchitis’. The bronchoalveolar lavage fluid cultures revealed Citrobacter braakii and the patient received targeted antimicrobial treatment.


Fig. 3
Flexible bronchoscopy reveals a nearly 90 % narrowing of the right upper lobe bronchus by a cauliflower-like lesion containing necrotic masses
Given the radiographic findings suggestive of free intraabdominal air under the diaphragmatic dome, while the patient denied any abdominal symptoms and had no history of surgery, a CT scan of the abdomen was requested. Other than the free intraabdominal gas, the scan revealed no pathologies. Following a surgical consultation a decision to perform exploratory laparotomy was made. Surgery revealed a perforated diverticulum of the large intestine. After surgery to the intestine for treatment of the perforation, the patient was re-admitted to the Department of Respiratory Medicine in April of 2013 to continue the treatment of persisting cough accompanied by a slight expectoration.
Repeated laboratory tests revealed that CRP persisted to be elevated at 111.1 mg/l. A chest radiogram (Fig. 4) and a CT scan (Fig. 5) showed a partial regression of the parenchymal changes in the right upper lung lobe seen in the previous imaging studies obtained in August of 2012. However, the CT scan revealed a complete obstruction of the right upper lobe bronchus. The patient underwent another flexible bronchoscopy, which revealed a foreign body in the right upper lobe bronchus and inflamed hypertrophic mucosa at the ostium of the bronchus (Fig. 6). An attempt was undertaken to remove the foreign body. However, not all its fragments could be removed (Fig. 7). Biopsies were collected form the mucosa lining the right upper lobe bronchus. Histopathological examinations of biopsy specimens revealed exacerbated chronic bronchitis, and necrotic and inflammatory masses. The foreign body consisted of plant fragments.
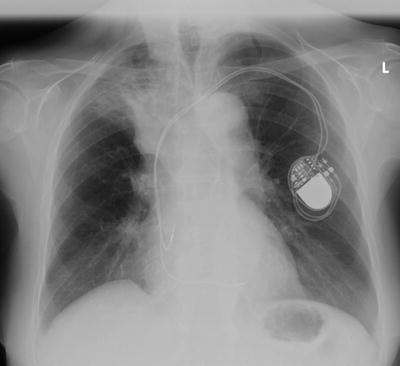



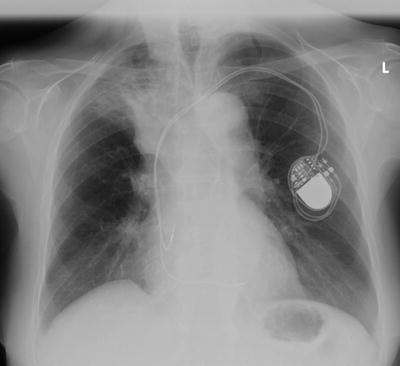
Fig. 4
Compared with the radiogram of Fig. 1, there was a partial regression of the lesions in the upper zone of the right lung and no air under the diaphragmatic domes

Fig. 5
Compared with the CT scan of Fig. 2, the previously revealed area of consolidation in the upper lobe of the right lung was decreased and lay along the outlines of the mediastinum and the oblique fissure. A complete obstruction of the right upper lobe bronchus was visible

Fig. 6
Flexible bronchoscopy revealed that the upper lobe bronchus was completely obstructed by a foreign body, with overlying growth of hypertrophic mucosa. An attempt to remove the foreign body was undertaken

Fig. 7
The right upper lobe bronchus after removal of the foreign body fragments shown in Fig. 6. However, not all the fragments could be removed flexible bronchoscopy
One week later in April of 2014 the patient underwent rigid bronchoscopy with jet ventilation. The foreign body in the bronchus, macroscopically, resembling a bone, completely obstructed the origins of the apical, posterior, and anterior segmental bronchi. It spontaneously defragmented, but all the fragments were successfully removed. The post-bronchoscopy course was uneventful. The patient remained under the care of a respiratory clinic. She reported no further respiratory complaints. The radiographic lesions in the right lung have completely regressed.
3 Discussion
Foreign body aspiration is a common occurrence in children. It is far less frequent in adults and mainly occurs in elderly patients with deglutition disorders (Sharma et al. 2006), which are due mostly to neurologic, rheumatologic, or iatrogenic causes (e.g., post-radio or chemotherapy) (Sentürk and Sen 2011). The neurologic causes of deglutition disorders include myasthenia gravis (Klair et al. 2014; Sura et al. 2012).
Myasthenia gravis is an autoimmune disease caused by the formation of antibodies to neuromuscular junction proteins. The diagnosis of myasthenia is based on the history (worsening of symptoms as the day progresses is characteristic), electrodiagnostic studies, detection of elevated anti-acetylcholine receptor antibody titer, and a positive anti-cholinesterase test, i.e., a transient resolution of myasthenic symptoms. While the reports of foreign body aspiration in patients with myasthenia can be found in the literature, they all concern children with juvenile myasthenia gravis (Murray and McAllister 2001; Winter and Koopman 1990).
Foreign body aspiration may manifest as a sudden dyspnea and in some cases results in acute respiratory failure. In adults, clinical manifestations often do not develop directly after choking. Therefore, patients often cannot recall any choking episode (Sentürk and Sen 2011; Ngoo et al. 2008). In some cases, the delay in establishing the correct diagnosis and initiating the appropriate treatment after aspiration can be long. Cough and wheezing are the most commonly reported long-standing manifestations which are suggestive of an airway foreign body (Ngoo et al. 2008; Sharma et al. 2006). In some patients, hemoptysis is also present (Mishra et al. 2014; Sentürk and Sen 2011).
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


