Chapter 5
Blunt and Penetrating Injuries
Written by H. van Aswegen, B.M. Morrow and E. van Aswegen
Trauma in the form of motor vehicle and pedestrian vehicle crashes, falls from a height, gunshot or stab wounds or physical abuse often result in blunt (non-penetrating) or penetrating injuries to the thoracic cage and/or abdominal organs.
In this chapter information is shared about:
•The causes and mechanisms of blunt or penetrating abdominal or thoracic injuries.
•The complications associated with abdominal or thoracic injuries.
•The medical and surgical management of patients with blunt or penetrating abdominal or thoracic injuries.
•The physiotherapy aims for the management of patients with such injuries in the intensive care unit and surgical or trauma ward.
•The contraindications and precautions related to the physiotherapy management of patients with blunt or penetrating abdominal or thoracic injuries.
•The physiotherapy interventions for patients who have suffered blunt or penetrating trauma.
•Adult and paediatric clinical case scenar ios.
5.1. Causes and Mechanisms of Injury
Injuries may be classified according to the site(s) and mechanism(s) of injury. Abdominal and thoracic trauma can be classified according to site as skeletal, pulmonary, heart and great vessels, visceral or diaphragmatic injury; and the mechanisms may be blunt or penetrating injury types. Blunt injuries result from forces distributed over a relatively large area and include deceleration or compression injuries. With penetrating injuries, forces are generally distributed over a small area and the organs injured are usually those that lie along the path of the penetrating object.
Abdominal or thoracic injuries, in the form of blunt or penetrating trauma, are often caused by falls from a height, motor vehicle and motor cycle crashes, pedestrian vehicle crashes, violence or attempted suicide. The epidemiology of thoracic and abdominal trauma varies according to social, economic, cultural and geographical characteristics (Herrera and Langer, 2008). A positive blood alcohol level and the use of drugs remain the highest risk factors for motor cycle, motor vehicle and pedestrian vehicle crashes, as well as for intentional injury caused to others or oneself (Carrasco et al., 2012; Brady and Li, 2013). Children are particularly vulnerable to trauma due to their physical size (smaller bodies result in a greater distribution of force), improper restraining in motor vehicles and issues of neglect or overt violence or abuse (Van As, 2010).
5.1.1. Penetrating injuries
Damage caused to the trunk by a penetrating object depends on the shape, size and velocity of the object, as well as the distance between the object and the person. The severity of a bullet injury is directly proportional to the amount of kinetic energy that is delivered to the tissues. The mortality associated with gunshot wounds is eight times higher than that of stab wounds (De Groot and Van Oppell, 2003).
5.1.1.1. Low-velocity injuries
Low-velocity penetrating injuries from civilian gunshot wounds or stab wounds damage only those tissues with which they come into direct contact. Axe or machete wounds cause extensive superficial damage without a great deal of internal injury (De Groot and Van Oppell, 2003). Disintegrating bullets are designed to break into small pieces upon contact with a surface harder than the bullet itself. Non-disintegrating bullets do not deliver significant kinetic energy to the tissues and cause less damage than disintegrating bullets. The path that handgun bullets follow through the body is unpredictable due to their low velocity and deflection may occur through bone or parenchymal organs such as the liver (Clarke, 2003; Livingstone and Hauser, 2004).
5.1.1.2. High-velocity injuries
High-velocity wounds can be caused by fragments of explosive devices such as grenades, bombs or high-velocity bullets from machine guns or rifles. High-velocity bullets cause damage to tissues in the path of the bullet, but also to remote organs. Shock waves radiate from the missile tract through the tissues, forcing them to accelerate violently forwards and outwards. A large cavity is formed that is larger than the diameter of the missile (Maiden, 2009; Hauer et al., 2011). This creates a vacuum that sucks debris, air and bacteria from the external environment into the primary missile tract and the cavity collapses over a period of a few milliseconds. Blood vessel and nerve damage, as well as shattering of bones, may result without these structures being directly hit by the bullet (Feliciano, 2004; Maiden, 2009; Hauer et al., 2011).
Penetrating abdominal and thoracic trauma is much less common than blunt trauma in the paediatric age group (Kadish, 2006; Saladina and Lund, 2006). However, the incidence of gunshot and stab injuries in children and adolescents is increasing at alarming rates in the US and South Africa (Prinsloo et al., 2012; Schecter et al., 2012), with unchanged rates of injury reported from the United Kingdom (Melling et al., 2012).
5.1.2. Abdominal injury
5.1.2.1. Abdominal injury in adults
Blunt abdominal trauma can result from direct injury, such as the rim of a steering wheel forced into the abdomen during a head-on motor vehicle collision or a tightly drawn seatbelt. These mechanisms can result in a crushing injury, in which the bowel is forced against the vertebral column, or a bursting injury, in which there is a sudden increase in pressure in the bowel. Indirect blunt injury to the abdomen can result from abrupt deceleration injury (fall from a height), with shearing forces causing injury next to sites of fixation of the bowel or solid viscera (Thomson, 2003).
The size of an abdominal organ and its contact with the anterior abdominal wall determine the frequency with which the organ is wounded. The most commonly injured organs are the abdomen, liver, small bowel (most commonly) and the colon (Feliciano, 2003; Thomson, 2003). Abdominal vascular injuries are common following penetrating trunk trauma. Abdominal injuries may accompany chest wounds or vice versa (Feliciano, 2003; Thomson, 2003).
Penetrating abdominal injuries are not immediately life threatening unless a major blood vessel is damaged. Stab wounds to the abdomen are easier to manage than those to the chest and involve injury to the major abdominal vasculature only 10% of the time (Feliciano, 2003). Stab wounds to the back are often accompanied by abdominal injuries. A gunshot wound that penetrates a major artery or vein and the colon is potentially lethal, initially due to haemorrhage and subsequently due to sepsis through the possible contamination of either the vascular wound repair site or the peritoneum (Feliciano, 2004).
5.1.2.2. Abdominal injury in paediatrics
Abdominal injuries affect 10–15% of injured children, with the spleen being the most affected organ (Gaines, 2009). Abdominal injuries are a marker of severe trauma in children (Coppola and Gilbert, 2011).
Children are at greater risk of abdominal injury following blunt trauma than adults because of their immature musculoskeletal system (Saladina and Lund, 2006). Children have less soft tissue to absorb the energy transmitted by a traumatic impact; incomplete ossification of the bony skeleton provides less protection to underlying viscera; and the pelvis is small and immature (Gaines, 2009). Another predisposing factor to severe paediatric abdominal injury is the smaller size of children, which results in abdominal organs being closely packed together. A force applied to the abdomen is distributed over a small surface area overlying a number of organs, increasing the risk of injury to multiple structures (Saladina and Lund, 2006; Zamakhshary and Wales, 2008). The spleen and liver are the most commonly injured abdominal organs in children, as they are more anterior and less protected by musculature than in adults, as well as the kidneys, which are more mobile and therefore less protected (Saladina and Lund, 2006; Klein, 2011). The presence of a seat belt sign (bruising of the abdominal wall by the lap belt) correlates with bowel injury in children following motor vehicle accidents, but its absence does not exclude abdominal injury (Chidester et al., 2009; Klein, 2011).
5.1.3. Thoracic injury
5.1.3.1. Thoracic injury in adults
The severity of injury resulting from thoracic trauma relates to the fundamental importance of the organs and physiological systems situated within the thoracic cavity.
Blunt thoracic trauma involves injuries such as fractured ribs, haemothorax, pneumothorax and pulmonary contusion. High-speed deceleration trauma may lead to cardiac, aortic, diaphragmatic and bronchial injuries. Myocardial contusion may accompany up to 76% of blunt thoracic injuries and, if diagnosed quickly, has a low mortality rate (Bansal et al., 2005). Diaphragmatic rupture occurs in less than 10% of victims of motor vehicle accidents. The left hemi-diaphragm ruptures more frequently than the right hemi-diaphragm, which is protected by the liver (Chughtai et al., 2009).
Penetrating injuries of the chest are the most lethal of injuries. The site and size of the wound to the chest wall determines the condition of the patient. The patient’s capacity to ventilate depends on the subsequent ability to sustain a negative intrapleural pressure (due to air leak from the lung into the pleural space), the extent of the parenchymal injury and oxygen delivery to the tissues (ventilation/perfusion (V/Q) ratio) (De Groot and Van Oppell, 2003). Pneumothoraces, lung collapse, diaphragmatic rupture and cardiovascular injury may all contribute to severe respiratory distress, which can be life threatening if left unattended (Livingstone and Hauser, 2004).
5.1.3.2. Thoracic injury in paediatrics
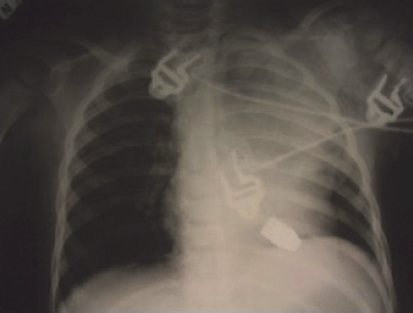
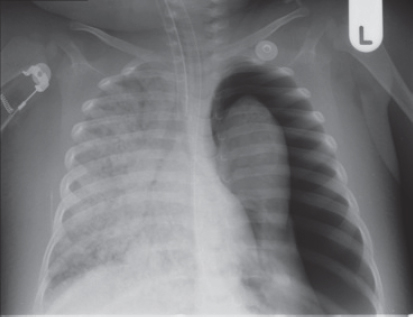
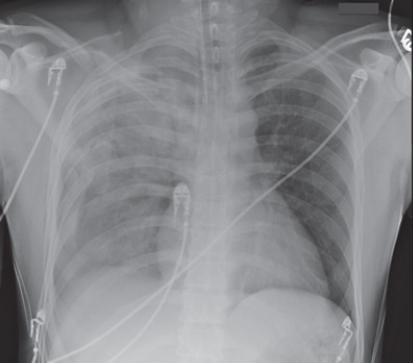
Paediatric thoracic trauma differs from adult thoracic trauma in terms of the mechanism and type of injury and the frequency of other organ system involvement (Kadish, 2006). Blunt trauma accounts for the vast majority (about 80%) of thoracic injuries in children (Herrera and Langer, 2008), although, unfortunately, penetrating trauma also occurs (Figs 5.1 and 5.2). The most common thoracic injuries in children are pulmonary contusions, pneumothorax (Fig. 5.3) or haemothorax and fractures. Lacerations of the heart, great vessels and lungs are relatively uncommon (Kadish, 2006). Commotio cordis is a rare occurence unique to paediatric thoracic trauma, in which sudden death follows discrete blunt chest trauma. It is postulated that an abrupt strike to the chest will, in some children, results in dysrhythmia followed by rapid cardiovascular collapse (heart- and vessel-related factors that lead to sudden reduction in effective blood flow) (Bliss and Silen, 2002).
Although the pliable cartilaginous rib cage in children makes rib fractures less common than in adults, it also results in the thorax being more vulnerable to serious injury (Kadish, 2006; Klein, 2011). The anterior ribs can actually be compressed to meet the posterior ribs on impact, resulting in severe pulmonary contusions, even without any rib fractures or other external evidence of trauma such as bruising (Bliss and Silen, 2002; Kadish, 2006; Tovar, 2008). Air and/or fluid in the pleural space more easily displaces the mobile mediastinum in children than adults, predisposing to tension situations with compromised venous return and cardiac output (Kadish, 2006). In children, thoracic trauma is frequently associated with abdominal trauma because of the close proximity of the chest and abdominal cavities (Kadish, 2006). Up to 12% of children will have abdominal injuries following blunt trauma (Zamakhshary and Wales, 2008).
Fig. 5.1:One-year-old child hit by a stray bullet to the chest, whilst asleep at home. Photo courtesy of Prof. A.B. van As, with permission.
Fig. 5.2:Chest x-ray showing a bullet close to the heart of a young child. Courtesy of Prof. A.B. van As, with permission.
5.2. Causes of Fatality after Abdominal or Thoracic Injuries
On-scene fatality due to traumatic injuries is high in the adult population. Death at the scene is greater with high-energy injuries (motor cycle, motor vehicle or pedestrian vehicle accidents; falls from a height; gunshot or stab injuries) than low-energy injuries (falls from low height), and mostly occurs due to traumatic brain injuries, high-level spinal cord injuries or severe blood loss from injury to the great vessels. In-hospital deaths in adults after trauma-related injuries are usually as a result of hypotension, respiratory distress or low admission Glasgow coma score (GCS) (less than eight) (Søreide et al., 2007; Evans et al., 2010).
In-hospital complications of thoracic and abdominal injuries may arise from impairment of cardiac output or gaseous exchange. Impaired cardiac output occurs due to blood loss, increased intrapleural pressures, blood in the pericardial sac, myocardial valve damage or vascular disruption. Impaired gaseous exchange develops due to atelectasis, contused lung tissue or disruption of the respiratory tract. Thoracic trauma contributes to mortality in a quarter of trauma-related deaths (Zargar et al., 2007; Oikonomou and Prassopoulos, 2011). The mortality rate increases in proportion to the time between injury and surgery (Adesanya et al., 2000). Multiple organ failure is a common cause of late-hospital fatality (Søreide et al., 2007; Evans et al., 2010).
In children, most fatalities at the scene result from lacerations of the heart, lung, blood vessels and bronchi, whilst in-hospital fatalities are mostly caused by cardiac tamponade, injuries to the great vessels and tension haemo- or pneumothoraces (Kadish, 2006). Prompt recognition of these conditions is therefore essential to reduce mortality. Although abdominal injuries are more common than thoracic injuries, they are 40% less fatal in children (Zamakhshary and Wales, 2008). Thoracic injury accounts for up to 12% of traumatic injuries and carries 5% mortality (Bliss and Silen, 2002). In multi-injured children, thoracic trauma increases mortality 20 times (Herrera and Langer, 2008).
5.3. Medical and Surgical Management of Survivors of Abdominal or Thoracic Trauma
The medical and surgical management of any patient with traumatic injury is divided into:
•primary survey and resuscitation of vital functions;
•detailed secondary survey as adjunct to the primary survey; and
•definitive care.
The specific management of patients with abdominal or thoracic injuries is outlined below in relation to the abovementioned three phases of care.
5.3.1. Primary survey and resuscitation of vital functions
On admission to the emergency department, initial assessment and management of the adult and paediatric patient focuses on identifying and reversing hypoxia, which is the most serious problem. Assessment for injuries that are life threatening is also done during the primary survey. Internationally, the ‘airways, breathing, circulation, disability, exposure’ (ABCDE) approach to basic life support is used for all adult and paediatric patients with trauma-related injuries admitted to casualty (Thim et al., 2012).
During the primary survey, ABCDE are all assessed, regardless of the organ system damaged. The ABCDE approach consists of assessment for (Thim et al., 2012) the following.
•Airway patency (with protection of the cervical spine), including the presence of oropharyngeal foreign body obstruction.
•Presence or absence of breathing. Respiratory movements and the quality of respirations are assessed using the ‘look (observe), feel (palpate) and listen (auscultate)’ approach. Shallow respirations are an early indicator of distress, whilst cyanosis is a late indicator. Pulse oximetry forms part of this assessment.
•Circulation by feeling the pulse for quality, rate and regularity. The skin is observed and palpated for colour, temperature and capillary refill. The neck veins are observed to assess whether they are flat or distended. Any active bleeding is stopped with compression over the wound. Penetrating objects are left in situ (Herrera and Langer, 2008). Electrocardiography (ECG) monitoring is done and blood pressure is measured.
•Disability by determining level of consciousness. This is done through assessing whether the patient is alert, voice responsive, pain responsive or unresponsive (AVPU approach). Pupil shape, size and reactivity to light are assessed as well as quality of limb movements. Blood glucose testing usually forms part of this assessment.
•Injuries by exposing the patient through the removal of clothes in order to visualise the skin and identify injuries. The patient’s clothes are removed but the patient is kept warm in order to prevent the onset of hypothermia.
Children with thoracic or abdominal injuries may present in respiratory or circulatory failure, but respiratory failure is more common with signs of tachypnoea, chest wall recessions or retractions and agitation secondary to hypoxia (Kadish, 2006).
Radiological investigations such as ultrasound technology, chest x-rays and computed tomography (CT) scans form part of the primary survey in order to identify life-threatening injuries that are not visible. Particularly in paediatric populations, ultrasound is extensively used in the diagnosis of thoracic and abdominal dysfunction and has the advantages of non-invasiveness and lack of radiation (Gaines, 2009). Diagnostic peritoneal lavage (DPL) may also be performed, if indicated, to diagnose intra-peritoneal haemorrhage.
Care provided to the patient in the emergency department during the primary survey includes oxygen therapy, placement of an endotracheal tube (ETT) if indicated, nasogastric tube placement to decompress the stomach if necessary, placement of peripheral intravenous (IV) lines for medication administration and fluid replacement therapy and, lastly, insertion of a urinary catheter. Analgesia is provided for pain relief.
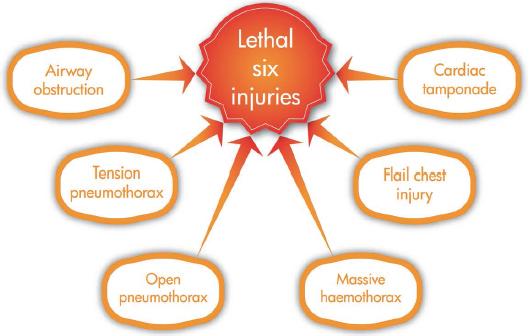
5.3.1.1. The lethal six injuries as a result of thoracic trauma
Figure 5.4 illustrates injuries that may result from thoracic trauma which constitute immediate life threats and are often termed ‘the lethal six’. Identification of ‘the lethal six’ injuries forms an important component of the primary survey. These injuries require immediate attention and can often be treated quickly and simply with a tube or needle (Tai and Boffard, 2003; Yamamoto et al., 2005). In the presence of commotio cordis in children, defibrillation may be life-saving (Herrera and Langer, 2008).
A description of each of these injuries follows below.
5.3.1.1.1. Airway obstruction
This is managed by positioning the patient’s head and neck to open the airway (with protection of the cervical spine) and suctioning to remove obstructions such as blood or vomit. Foreign bodies causing obstruction should be removed if possible. The insertion of an artificial airway may be indicated for an unconscious patient (Thim et al., 2012).
5.3.1.1.2. Tension pneumothorax
Tension pneumothoraces occur following an injury to the lung, which results in an air leak with a one-way valve effect. This leads to the accumulation of air in the pleural space with a progressive build-up of pressure resulting in mediastinal shift and lung compression (Fig. 5.3). If not resolved it can lead to reduced venous return, decreased cardiac output, diaphragmatic inversion, subcutaneous emphysema and ultimately cardiorespiratory arrest. The presence of a simple pneumothorax can be assessed through the use of ultrasound technology such as extended focussed assessment with sonography for trauma (FAST). This non-invasive assessment tool is also useful in identifying the presence of blood in the pericardium (Rippey and Royse, 2009). In the absence of ultrasound technology, chest x-ray or CT scan can be used for confirmation of diagnosis. Emergency treatment is needle decompression via the second intercostal space in the mid-clavicular line, followed by insertion of an intercostal drain (ICD).
5.3.1.1.3. Open pneumothorax (‘sucking chest wound’)
Normal ventilation requires a negative intra-thoracic pressure. A large open chest wall defect leads to the equilibration of intra-thoracic and atmospheric pressures, and if the hole is more than two-thirds of the tracheal diameter, the air preferentially flows through the chest defect, leading to severe hypoxia. Emergency treatment requires the defect to be sealed and secured with a dressing on three sides (total occlusion may lead to tension pneumothorax) and placement of an ICD at a site remote from the open chest wound, followed by definitive surgical repair (Smith, 2013; Trauma.Org, 2013b).
5.3.1.1.4. Massive haemothorax
This refers to a rapid accumulation of a large volume of blood in the chest cavity, leading to hypovolaemia and hypoxaemia. On examination the neck veins may be either flat from hypovolaemia or, on rare occasions, distended as a result of the intrathoracic blood. Breath sounds are absent and the thorax is dull to percussion. Extended FAST can be used for diagnosis of a haemothorax (Rippey and Royse, 2009). But again, in the absence of ultrasound technology, chest x-ray or CT scan can be used for confirmation of diagnosis. Emergency management is the insertion of a large-bore (adult 32–36 French gauge (FG); child 16–24 FG; infant 12–16 FG; newborn 8–12 FG) tube to drain the blood, followed by either closed drainage or open thoracotomy.
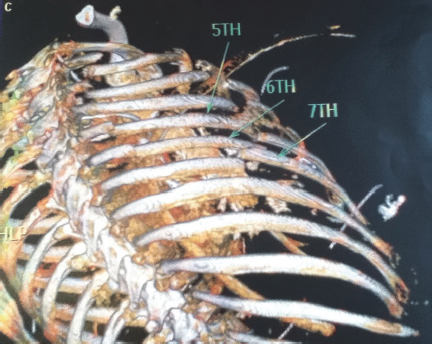
5.3.1.1.5. Flail chest
Flail chest is usually a result of direct impact to the chest wall. Two or more adjacent ribs are fractured in two or more places, producing a ‘free-floating’ segment of chest wall which moves paradoxically (opposite to normal chest wall motion) with respiration (Fig. 5.5). This leads to pain and restricted chest wall movement, and the underlying pulmonary contusion results in reduced lung compliance and atelectasis. Chest x-ray or CT are used for confirmation of diagnosis. Emergency management involves ensuring adequate ventilation, providing humidified oxygen, fluid resuscitation, pain management and stabilising of the chest. Flail rib segments are rare in children due to the marked pliability of the chest wall, but if present are likely to lead to severe respiratory decompensation (Bliss and Silen, 2002; Kadish, 2006).
5.3.1.1.6. Cardiac tamponade
Blood in the pericardial sac, usually resulting from penetrating injuries, prevents cardiac activity. The patient may present with ‘Beck’s triad’ which constitutes:
•elevated venous pressure;
•decreased arterial pressure; and
•muffled heart sounds.
Furthermore, there may be ‘pulsus paradoxus’: a decrease of 10 millimetres of mercury (mmHg) or greater in systolic blood pressure (BP) during inspiration. A systolic to diastolic gradient of greater than 30 mmHg is also suggestive of cardiac tamponade. Diagnosis is confirmed through the use of extended FAST (Rippey and Royse, 2009). Emergency treatment is the removal of a small amount of blood from the pericardial sac.
5.3.1.2. Abdominal trauma
In the case of abdominal injury, a thorough clinical examination is done to identify signs of internal bleeding, such as stomach distension, rectal bleeding and blood in gastric aspirate or in the urine. Radiological examination includes chest and pelvis x-rays for patients with multiple injuries due to blunt trauma. Those who have penetrating trauma to the abdomen and who are haemodynamically stable also undergo abdominal x-ray (American College of Surgeons Committee on Trauma, 2008). FAST has been shown to be as specific in the diagnosis of the presence of blood in the peritoneum as DPL and abdominal CT scan (American College of Surgeons Committee on Trauma, 2008; Rippey and Royse, 2009; Quinn and Sinert, 2011). Diagnostic peritoneal lavage may be performed in patients with blunt trauma to the abdomen in the presence of haemodynamic instability to identify haemorrhage if FAST is negative or if a CT scan is not available. It is an invasive procedure but is deemed to be 98% accurate in the diagnosis of intraperitoneal bleeding (American College of Surgeons Committee on Trauma, 2008; Quinn and Sinert, 2011).
5.3.2. Secondary survey as adjunct to primary survey
The secondary survey also takes place in the emergency department. It begins after the completion of the primary survey, when resuscitation has been carried out and vital functions normalised. The secondary survey is a ‘head-to-toe’ evaluation of the patient, which involves taking a detailed history of the patient as well as a complete neurological and physical examination.
Care provided to the patient during the primary survey continues in the secondary survey. If the patient’s condition is stable, placement of arterial and central venous pressure (CVP) lines are performed. If the patient’s condition is unstable, placement of these lines is done in theatre or in the intensive care unit (ICU) as part of definitive care.
The secondary survey is guided by suspicion for injuries missed during the primary survey, especially in patients who are unconscious or unstable. The presence of possible abdominal injury should be confirmed, as serious complications can occur in both adults and children if diagnosis is delayed.
•Computed tomography is used to rule out any undiagnosed injuries to the heart and major thoracic vasculature, injuries to the diaphragm, intra-abdominal haemorrhage and intestinal perforation, as well as injuries to other parts of the body, especially in the case of multiple blunt trauma (American College of Surgeons Committee on Trauma, 2008; Chidester et al., 2009; Van Vugt et al., 2011).
•Computed tomography with contrast may be needed to identify isolated injuries to the duodenum, ascending or descending colon, rectum, biliary tract and pancreas which were not identified through DPL (American College of Surgeons Committee on Trauma, 2008).
•Multi-detector CT scan may be used, if available in the trauma centre, to identify internal bleeding in haemodynamically stable patients with blunt abdominal organ injury (Van der Vlies et al., 2011).
•Diagnostic laparoscopy may be needed if uncertainty remains following non-invasive diagnostic measures (Gaines, 2009).
5.3.2.1. The hidden six injuries that result from thoracic trauma
Figure 5.6 illustrates thoracic injuries that are considered to be potential life threats and are often referred to as ‘the hidden six’ (Tai and Boffard, 2003; Yamamoto et al., 2005; Nayak, 2008). Suspicion of these injuries guides the secondary survey.
The ‘hidden six’ injuries follow below.
5.3.2.1.1. Pulmonary contusion
Pulmonary contusion refers to injury of the lung parenchyma without laceration. It is a potentially life-threatening condition with an insidious onset, and is particularly common in children (Kadish, 2006). Interstitial haemorrhage and oedema fluid that result from the contusion leak into the alveoli and cause reduced pulmonary compliance, atelectasis (exacerbated by decreased surfactant production by injured alveolar cells) and hypoventilation. Bronchospasm may result from bleeding into lung segments that were not affected at the time of injury and this leads to further pulmonary dysfunction. Pulmonary dysfunction may also be compromised by increased mucus production and decreased clearance of mucus (Cohn and DuBose, 2010). More than 50% of adults and 20% of children will develop pneumonia, even with treatment (Bliss and Silen, 2002; Tovar, 2008).
The risk of pulmonary oedema must be considered when managing such patients. In children, it may be difficult to differentiate aspiration from contusion. Aspiration may occur at the time of injury, during intubation or following vomiting whilst in the supine position (Bliss and Silen, 2002). Usually, the right lower lobe is affected due to the structure of the tracheobronchial tree, but diffuse infiltrates may be seen on a chest x-ray. Pulmonary contusion usually resolves by day seven after injury (Cohn and DuBose, 2010). See Fig. 5.7 for a chest x-ray example of pulmonary contusion.
Fig. 5.7:Blunt chest trauma resulting in rib and clavicle fractures, haemothorax and pulmonary contusion on the right.
5.3.2.1.2. Myocardial contusion
Myocardial or cardiac contusions occur as a result of blunt precordial chest trauma and are often difficult to diagnose. There is a risk of dysrhythmias, tamponade, pericarditis and sudden death. Myocardial contusion is diagnosed by ECG and elevated cardiac-specific enzyme levels. Blunt cardiac injury is rare in children, occurring in less than 5% of paediatric trauma patients (Taio et al., 2000; Kadish, 2006).
5.3.2.1.3. Traumatic disruption of the aorta
This type of injury is associated with rapid deceleration-type accidents. It is associated with high mortality at the accident scene, and for those who survive to hospital, mortality increases significantly with each undiagnosed day. Disruption occurs at the ligamentum arteriosum (ductus arteriosus) and results in a contained haematoma of 500–1000 ml of blood. Specific radiographic signs include a widened mediastinum, tracheal and oesophageal deviation to the right, and first and second rib fractures. Definitive surgical repair is required (O’Connor et al., 2009).
Great vessel and cardiac injuries are much less common in children than in adults (Bliss and Silen, 2002; Kadish, 2006). However, more than 80% of children who sustain an aortic tear will also have significant injuries to the lung, heart, abdominal viscera and nervous system, and there is a high associated mortality (Bliss and Silen, 2002; Kadish, 2006).
5.3.2.1.4. Traumatic diaphragmatic rupture
Diaphragmatic tears lead to immediate or delayed visceral herniation and lung compression. Left-sided hemi-diaphragm rupture is more common than right-sided hemi-diaphragm rupture in adults due to the protection provided by the liver (Chughtai et al., 2009; Vilallonga et al., 2011).
In children, diaphragmatic rupture occurs in up to 5% of cases following major chest trauma, particularly blunt trauma. The site of rupture is usually posterolateral (Chughtai et al., 2009; Moore et al., 2009). Surgical repair is the definitive treatment.
5.3.2.1.5. Tracheobronchial injury
Tracheobronchial injury refers to injury involving the larynx, trachea or bronchus. Injury to the larynx is rare. Suspicion is raised if the patient presents with hoarseness of the voice or subcutaneous emphysema and intubation proves to be difficult. Tracheal injury may be accompanied by oesophageal injury. Bronchial injury, usually due to blunt trauma, is rare and may be lethal. Injuries to the tracheobronchial tree are rare in children, but may occur following both penetrating and blunt trauma and are associated with up to 30% mortality (Bliss and Silen, 2002; Tovar, 2008). Up to 80% of all paediatric airway injuries occur in the distal trachea or bronchi. Most injuries show mediastinal air, although more distal injuries may present with pneumothoraces (Bliss and Silen, 2002; Kadish, 2006).
5.3.2.1.6. Oesophageal trauma
This is commonly caused by penetrating injury and may be lethal if not recognised. A high suspicion of oesophageal trauma is raised if the patient has a left pneumothorax and haemothorax without rib fractures. Another cause for concern is the presence of shock out of proportion to apparent blunt chest trauma, and there may be particulate matter in the ICD tube (Bliss and Silen, 2002). Oesophageal injuries are rare in children and are difficult to diagnose. Oesophageal perforation in children is mostly caused by iatrogenic injury followed by penetrating trauma and may have devastating consequences, such as mediastinal sepsis and death (Kadish, 2006).
5.3.3. Definitive care
Definitive care is initiated after completion of the primary and secondary surveys. At this point the patient is transferred out of the emergency department either to theatre for surgical intervention or to the ICU for close monitoring and care.
The types of definitive care provided for patients who have suffered blunt or penetrating injuries to the abdomen or thorax are discussed below.
5.3.3.1. Abdominal injury
Several adult patients with blunt abdominal organ injury who are haemodynamically stable are successfully managed non-operatively (Van der Vlies et al., 2011). In children, most injuries to the abdominal organs are managed non-operatively with very high success rates (Zamakhshary and Wales, 2008; Gaines, 2009). These patients are admitted to the ICU for monitoring and therapy.
An adult or paediatric patient with blunt abdominal trauma who presents with shock due to intra-abdominal bleeding is immediately taken to theatre for surgical intervention in the form of an exploratory laparotomy. A laparotomy is also performed if a patient with penetrating trauma presents with multiple organ injuries, haemodynamic instability, prolonged hypoxia, significant intra-abdominal blood loss or evidence of hollow visceral injury (Adesanya et al., 2000; Thomson, 2003; Gaines, 2009). The vertical abdominal incision gives the surgeon sufficient exposure to the intra-abdominal organs to identify injuries, control bleeding and contain contamination. Where possible all dead and contaminated tissue is excised to leave healthy tissue behind (Vikram, 2011).
After surgery the patient is transferred to the ICU for further care and monitoring. Special attention is paid to the detection of the development of abdominal compartment syndrome (increased pressure in the abdomen). Abdominal compartment syndrome develops due to increased pressure in the intra-abdominal compartment from large-volume fluid resuscitation after major abdominal surgery and also tight abdominal wall closure after emergency laparotomy procedures. This increase in intraabdominal pressure leads to symptomatic organ dysfunction such as acute renal failure (Subramanian et al., 2008). Like adults, children can develop abdominal compartment syndrome, with a high associated mortality if not treated timely (Gaines, 2009).
5.3.3.1.1. Damage control surgery
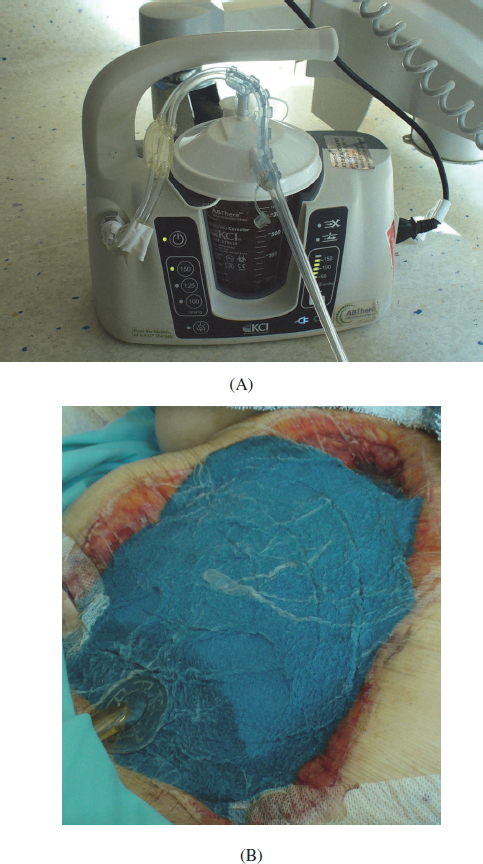
Damage control is a concept that is being used more frequently internationally (Kirkpatrick et al., 2006). Damage control involves a staged approach to the repair of damaged abdominal organs. Initially the surgeon repairs only major organ tears to stop internal bleeding and control contamination. The visceral cavity is packed with dressings to control capillary oozing, the abdominal wall is left open and the patient is taken to the ICU to be stabilised (Fig. 5.8). Repair to smaller organ tears is done in theatre once the patient is in a more stable condition (24–48 hours after initial operation). Definitive repair is completed with closure of the abdominal wall, provided that intra-abdominal swelling had subsided (Cirocchi et al., 2010, 2013).
The administration of large volumes of IV fluid during surgery may result in excessive swelling of the intestines and mesentery and retroperitoneal tissues in patients with severe abdominal trauma. The abdominal walls become less compliant due to oedema and closure of the abdominal fascia may lead to increased intraperitoneal pressure. This may result in decreased blood flow to the hepatic, renal and intestinal organs due to intra-abdominal hypertension or compartment syndrome, as discussed above (Subramanian et al., 2008).
Unplanned relook laparotomy becomes necessary in the presence of intra-abdominal sepsis, intra-abdominal bleeding, missed injuries, small bowel obstruction and fluid leaks at anastomosis sites. Between surgical interventions, patients are monitored and managed in the ICU until they have stabilised. Patients who undergo unplanned relook laparotomy have a higher mortality rate than those patients who do not. Negative pressure wound therapy may be used as part of wound care for such patients (Figs 5.9A and B) (Roberts et al., 2012). This involves the delivery of negative pressure to the wound site through the placement of patented sponge material inside the wound, together with a drainage tube that is attached to a suction machine at the bedside. This negative pressure assists in removing infectious material from the wound site, promotes the formation of granulation tissue and helps to draw the wound edges closer together (Roberts et al., 2012). The abdominal wound is closed surgically when sepsis is resolved.
Fig. 5.8:Damage control surgery. Open abdominal wound packed with sterile sponge material and covered with transparent adhesive film.
5.3.3.2. Thoracic injury
The definitive management of blunt and penetrating chest injuries is very similar.
Fig. 5.9:Negative pressure wound therapy. (A) KCI vacuum device; (B) Wound drainage tube exiting inferior to the sponge material.
5.3.3.2.1. Pneumothorax or haemothorax
Pneumo- or haemothoraces are managed with the placement of an ICD, as mentioned previously, to release pressure from the pleural space, as part of standard care. Low-pressure, high-volume suction may be necessary to encourage re-expansion of collapsed lung regions (Paramasivan and Bodenham, 2007). Prompt drainage of blood from the pleural space is essential in adults and children with haemothoraces because as the haematoma organises, it may be replaced by fibrous scar tissue, causing lung entrapment, which predisposes the patient to chronic atelectasis, V/Q mismatch, pneumonia or empyema (Bliss and Silen, 2002). Drainage also provides a method to measure and monitor the volume and rate of blood loss. A thoracotomy may be indicated for direct closure of the wound if low-pressure, high-volume suction is unsuccessful (Keilin et al., 2003; Paramasivan and Bodenham, 2007).
5.3.3.2.2. Posttraumatic empyema
Posttraumatic empyema may result from either blunt or penetrating chest injuries in 10–27% of adult cases and contributes to morbidity and mortality (Hoth et al., 2002; DuBose et al., 2012). A retained haemothorax is primarily associated with the development of posttraumatic empyema and is often caused by rib fractures. Blood trapped in the pleural space impairs its own absorption and forms an ideal environment for bacterial growth. The placement of an ICD may lead to contamination of a retained haemothorax and the development of empyema.
The diagnosis of posttraumatic empyema is made through chest CT and the presence of clinical findings such as increased leukocyte count, fever and worsening respiratory function.
The management of posttraumatic empyema includes thoracotomy for decortication and re-expansion of the involved lung, less invasive video-assisted thoracoscopy or intrapleural administration of fibrinolytic agents such as streptokinase or urokinase (Hoth et al., 2002; Paramasivan and Bodenham, 2007; DuBose et al., 2012).
5.3.3.2.3. Cardiac, airway or great vessel injuries
These injuries may be managed conservatively initially with close patient monitoring. The unstable hypotensive patient is managed surgically with a median sternotomy incision or high antero-lateral thoracotomy incision to gain access to the great vessels, trachea or bronchi, oesophagus and the heart to repair damage. Repair of the thoracic aorta requires single lung ventilation and a thoracotomy incision at the fourth intercostal space on the left side of the chest wall (Keilin et al., 2003; O’Connor et al., 2009).
5.3.3.2.4. Soft tissue injuries of the chest wall
Entrance and exit wounds of gunshot injuries are debrided thoroughly. Necrotic tissue and debris create an ideal focus area for infection. Gas gangrene may develop in neglected wounds or those that have undergone inadequate debridement. Reconstructive surgery may be indicated for wounds with large loss of chest wall integrity (Clarke, 2003; De Groot and Van Oppell, 2003; Mauffrey, 2005).
5.3.3.2.5. Pulmonary contusion
Control of pain originating from the chest wall, accurate fluid management and aggressive bronchial hygiene are important components of the treatment of all patients with pulmonary contusion. Patients with severe pulmonary contusion should be monitored closely to ensure adequate oxygenation and organ perfusion. Intermittent positioning in prone can be used to optimise oxygenation (Cohn and DuBose, 2010).
The use of epidural analgesia has been shown to decrease the duration of mechanical ventilation (MV) and the rate of development of nosocomial pneumonia more so than the use of IV opioids in patients with multiple rib fractures and pulmonary contusion. Regional analgesia is also recommended for pain control in patients with rib fractures and pulmonary contusion (Cohn and DuBose, 2010). The survival rate of adults with pulmonary contusion and rib fractures is reported to change from 60–93.5% when pain is adequately controlled, allowing for early chest physiotherapy intervention and mobilisation (Cohn and DuBose, 2010).
Neutrophil-induced lung injury may be restricted with the early administration of hypertonic saline (Bastos et al., 2008; Cohn and DuBose, 2010), but large clinical trials are needed to confirm this finding. Restricted crystalloid IV fluids are given to prevent the development of pulmonary oedema. Intravenous red packed cells and plasma are given to restore blood volume. Diuretics may be used to treat pulmonary oedema (Bastos et al., 2008). Steroid use for patients with pulmonary contusion is not recommended as it may increase the risk for the development of pneumonia (Cohn and DuBose, 2010).
The use of non-invasive positive pressure ventilation may prevent the need for intubation and MV (Cohn and DuBose, 2010). Patients with pre-existing conditions, such as emphysema or renal failure, may need early intubation. In patients with pulmonary contusion who require MV, the use of alveolar recruitment manoeuvres or high-frequency oscillatory ventilation have been reported to improve oxygenation. It is important that any MV strategy that is decided upon should minimise the risk of induced barotraumas (Cohn and DuBose, 2010).
Between 20 and 35% of children with pulmonary contusion will require MV, fewer than in adults (Bliss and Silen, 2002; Norton et al., 2008). Ancillary measures in paediatrics include fluid restriction, supplemental oxygen, pulmonary toilet and pain control.
5.3.3.2.6. Diaphragmatic injury
Diaphragmatic ruptures are managed through surgical intervention, with laparotomy incision being the golden standard. In some instances thoracotomy is performed for a right-sided hemi-diaphragm rupture (Chughtai et al., 2009; Vilallonga et al., 2011).
5.3.3.2.7. Skeletal injuries of the chest wall
Unless rib fractures are causing instability, the main aim of management is pain reduction and prevention of pulmonary complications such as atelectasis and infection. This can be achieved by using the following methods.
•Non-invasive positive pressure ventilation (NIPPV) through a fitted face mask together with adequate analgesic support. This is used to improve chest wall stabilisation for patients with multiple rib fractures or flail chest injuries. Oxygen therapy should be humidified so as not to compromise the function of the mucociliary escalator. Mechanical ventilation through an artificial airway is avoided for as long as possible due to its associated risk of complications (Bastos et al., 2008). Gunduz et al. (2005) reported that patients with flail chest injuries who were managed with NIPPV had lower mortality and incidence of nosocomial infection than those with flail chest injuries who were intubated and mechanically ventilated.
Operative stabilisation of flail rib fractures can be performed if a patient continues to suffer with poor oxygenation despite optimal MV support (Fitzpatrick et al., 2010).
Circumferential strapping of the chest wall in the presence of rib fractures is contraindicated for pain relief, as it leads to the development of respiratory complications by restricting chest wall expansion (Clarke, 2003; Trauma.Org, 2013a).
5.3.3.2.7.4. Sternal fracture. Sternal fractures occur more commonly in adults than children due to reasons previously mentioned. Sternal fractures are managed with analgesia and oxygen therapy. Open reduction and internal fixation is indicated for overlapping sternal fractures (Kadish, 2006; Panté et al., 2010).
5.3.4. Prolonged intensive care unit stay
The severity of injury following blunt or penetrating trauma and increasing patient morbidity due to the development of infection or sepsis can lead to prolonged duration of MV, resulting in longer ICU stay. Under these circumstances the inter-professional team may consider replacing the patient’s endotracheal tube with a tracheostomy tube to make the process of weaning from MV easier for the patient. The care of the patient’s tracheostomy should be a priority for each member of the interdisciplinary ICU team, as poor standards of care directly influence the patient’s mortality (Mitchell et al., 2013).
5.3.4.1. Tracheostomy care
5.3.4.1.1. Indications for tracheostomy
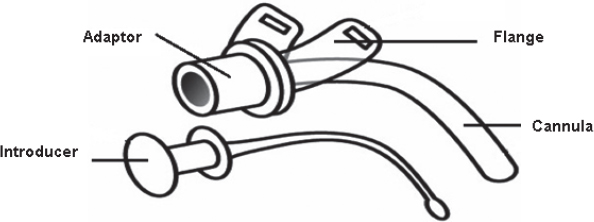
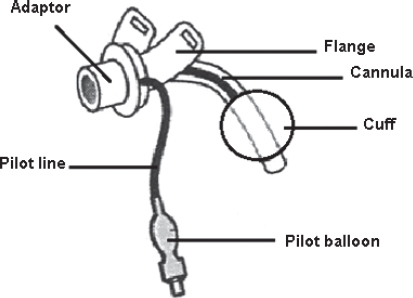
A tracheostomy involves the creation of an opening (stoma) on the neck, through which a tracheostomy tube is inserted into the trachea. The main components of adult and paediatric tracheostomy tubes are displayed in Figs 5.10A and B.
Permanent tracheostomy may be used for patients with cancer of the upper airways (adults) or other forms of upper airway obstruction (e.g. Pierre Robin sequence, laryngeal webs etc.) to assist with the maintenance of an intact airway. This is beyond the scope of this text and will not be discussed further. Temporary tracheostomy can be used in a variety of patients, but is performed in the trauma population under the following circumstances.
•To protect the airways from swelling and compression after traumatic injury or surgical procedures performed to the head or neck.
•Prolonged duration of MV (> 10 days in adults; variable in young children) (Fig. 5.11).
•To facilitate weaning from MV, as tracheostomy reduces the need for sedation and reduces dead space and the resistance to airflow created by the ventilator circuit.
A tracheostomy is performed either through a traditional surgical approach or percutaneous dilatational techniques (Mitchell et al., 2013). The reader is referred to Section 5.8 for additional sources that discuss the types of tracheostomy tubes, sizes of tracheostomy tubes and the emergency equipment that should be kept by the patient’s bedside in the case of unforeseen circumstances.
5.3.4.1.2. Positioning of the tracheostomy tube
On chest x-ray assessment the tracheostomy tube tip should extend more than half the distance between the stoma and the carina. The tracheostomy should be positioned parallel to the long axis of the trachea and should be two-thirds the diameter of the trachea in size (Kacmarek et al., 2013).
The tracheostomy tube should be securely fastened to the patient’s neck with tracheostomy tape. Tracheal injury and accidental decannulation (removal) can occur if the ventilator tubing pulls excessively on the tracheostomy tube. Good clinical practice involves reducing the leverage of the ventilator tubing on the tracheostomy by securing the tubing to drip stands above or next to the patient’s bedside.
5.3.4.1.3. Tracheostomy chart
Care of the patient with a tracheostomy can be enhanced by placing a clearly visible tracheostomy chart above the patient’s bed in the ICU or on the ward. Information that should be communicated through this chart includes the following:
•the type of procedure used for insertion of the tracheostomy (surgical or percutaneous);
•the date on which the tracheostomy was performed;
•the tracheostomy tube size; and
•people to contact in case of an emergency, e.g. anaesthesia department, ICU, ear-nose-throat specialist, maxilla-facial surgeon or the hospital emergency department.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree