Home Blood Pressure Telemonitoring: conventional and mobile health-based approaches
11.2 Definitions
Telemedicine or telehealth consists in the exchange or delivery of medical information (e.g., health parameters, biological signals, diagnostic images) from one site to another via electronic communications in order to provide diagnosis and care at distance [7].
For many years, telemedicine systems were based mainly on strategies in which teletransmission was performed by means of personal computers equipped with internet connection [8]. However, the worldwide increase in the use of smartphones observed in recent years, along with the development of applications for patients’ data monitoring, has offered new perspectives for telemedicine and the potential to improve interaction between doctors and patients, an approach defined as “ mobile health ” or m-health [9–11]. BPT represents a particular application of telemedicine using either computer-tailored or m-health strategies [12]. It consists of automatic data transmission of BP values and additional parameters, from the patient’s living site (home or work place HBPT) or from a professional healthcare environment (e.g., primary care clinic or community pharmacy) to the doctor’s office or to a hospital [12] (Box 11.1).
Box 11.1: Definitions
e-health of Digital health
The use of electronic processes and information and communication technologies to provide healthcare services
Telemedicine (also referred to as telehealth )
Teletransmission of health-related data from one site to another via electronic communications
M-health or “ mobile health ”
Teletransmission of health-related data by means of mobile communication devices (i.e., smartphones)
Blood Pressure Telemonitoring (BPT)
Teletransmission of BP values by means of traditional computer-based or m-health strategies
11.3 Methodological Aspects for Application of BPT
11.3.1 Conventional (eHealth Based) BPT Systems
The wide availability and low cost of automated BP measuring devices, the current advances in communication and information technologies, and the emphasis put by healthcare systems on delivering patient-centered care have stimulated development of home BPT, i.e., a particular application of telemedicine based on either personal computer or m-health strategies (see Fig. 11.1 and Box 11.1).
Types of BP measuring devices and data collection and communication technologies used for blood pressure telemonitoring
BP measuring devices |
• Automated devices (wired or wireless) |
• Multiple parameters monitoring devices (e.g., single channel ECG, pulse oximetry, body temperature, blood glucose, medication intake) also known as “medical tricorders” |
• Wireless smartphone applications (paired with an external wireless BP monitor or turning the smartphone into a cuffless BPM device) |
• Wearable monitors for long-term surveillance (e.g., wrist tonometers or finger pletismographs) |
Data communication technologies |
Data transmission (download) from the device |
• Dedicated wireless devices based on bluetooth, wi-fi, zigbee or NFC and with built-in mobile phone-based transmission systems (e.g., home hubs or smart boxes) |
• Handheld devices (smartphones, tablets, PDAs, etc.) with wireless communication linked to private (home) or public (community) wi-fi access points or to the mobile public network |
• Desktop or laptop computers linked to the BP measuring devices via wired (USB cable) or wireless connection |
Data transmission (upload) to the telemedicine provider |
• Landline broadband wired telephone lines (via a data modem or an acoustic coupling system) |
• Broadband mobile network |
• Peer-to-peer connection or the Internet |
• Health exchange servers acting as single point forward hubs in the cloud (gateway) |
Type of data transmitted |
• Immediate or periodic automatic forward of encrypted data strings with proprietary or standard formats |
• Manual data input by text messaging (SMS, social media applications such as whatsapp, facebook messenger, etc.) |
• E-mail messaging (manual data input or list of readings sent as an attachment) |
• Website with dedicated forms allowing manual data input or manual upload of files |
Overall, home BPT systems require active involvement of patients who should self-monitor their BP levels and other related clinical variables and send these values to a healthcare provider. Current HBPT solutions allow self-BP measurements performed by patients at home to be in the device memory and the forwarded, immediately or periodically, to a remote computer host through a landline broadband or mobile network, and through the web by applying encryption transmission protocols which ensure data integrity and security [13]. Once data are received at the central telemedicine server they are stored and analyzed. Reports are automatically generated and then reviewed by a healthcare professional (usually a technician, a nurse, or a pharmacist), before they are submitted to the reporting physician, although in some instances reports are directly sent to the family doctor in charge. At the end of this process a medical report is forwarded to the patient and referring primary physician through a website, via e-mail or through dedicated smartphone apps (see Fig. 11.1). During all these processes the healthcare professional may also interact with the patient in order to obtain feedbacks on his/her health status and adjust treatment according to the indications of the managing physician (co-intervention or additional support) [14].
11.3.2 mHealth-Based BPT Strategies
Main mobile phone applications for mHealth-based BPT strategies
Type of App | Advantages | Disadvantages |
|---|---|---|
Manual insertion of BP values by user | − Flexibility − Widely available in digital stores − Not tied to specific devices − Measurement and recording of BP values can be performed at different times − May provide adaptative self-care practices via text messaging | − High risk of errors in transcription of BP values from the device to the phone |
Automated transmission from an oscillometric device to the phone | − Widely available − High accuracy of validated devices − Automated transmission of data: easy to obtain and low risk of errors | − Tied to a specific device brand or model − Cost |
Wireless cuff paired to the phone | − High portability − Automated transmission of data: easy to obtain and low risk of errors − May provide adaptative self-care practices via text messaging | − Tied to a specific device brand or model − Controversies on accuracy of BP readings − Lack of transparency and evaluation of the algorithms − Uncertainty of privacy issues and security of data storage |
Cuffless measurement through the phone | − No need for devices other than the smartphone − Always available | − Lack of standardization − Low accuracy, no validation for app-related tools |
Apps associated to automated transmission of BP values from the BP measurement devices to the phone have the advantage to be associated to either conventional or automated oscillometric BP measurement devices able to send data to smartphones, or equipped with specifically designed cuffs with an inflating system that works only when paired to a phone. Although wireless cuffs that work with a paired phone have been developed and seem appealing for the user due to their extreme portability, their accuracy has been questioned due to the high variability of BP measures compared to standard BP measurement techniques [15].
Apps that turn the smartphone into a BP measurement device (cuffless measurement) without the need for ad hoc external devices have also been developed based on measurement principles such as pulse transit time assessment or even without the need for any other device than the smartphone, by applying the subject’s finger to the phone camera. Although their extreme ease of use in any circumstance and free availability make them particularly attractive to smartphone users, a major limitation of these apps is the limited evidence from validation studies supporting their accuracy. A recent study evaluating one of these apps indeed indicated that this approach may be highly inaccurate, underestimating higher BP and overestimating lower BP values (mean, SD of the absolute values of the difference between the app and standard were 12.4, 10.5 mmHg for SBP and 10.1, 8.1 mmHg for DBP), thus strongly supporting the need of proper validation of the BP data provided by apps of this kind [16]. The low sensitivity for hypertensive measurements means that approximately four-fifths (77.5%) of individuals with hypertensive BP levels will be falsely reassured that their BP is in the non-hypertensive range. These results have raised awareness on the need to reinforce partnership of app developers, distributors, and regulatory bodies to set and follow standards for safe, validated mHealth technologies.
11.4 BPT: Effects on BP Levels and on Achievement of BP Control
11.4.1 Conventional BPT Systems
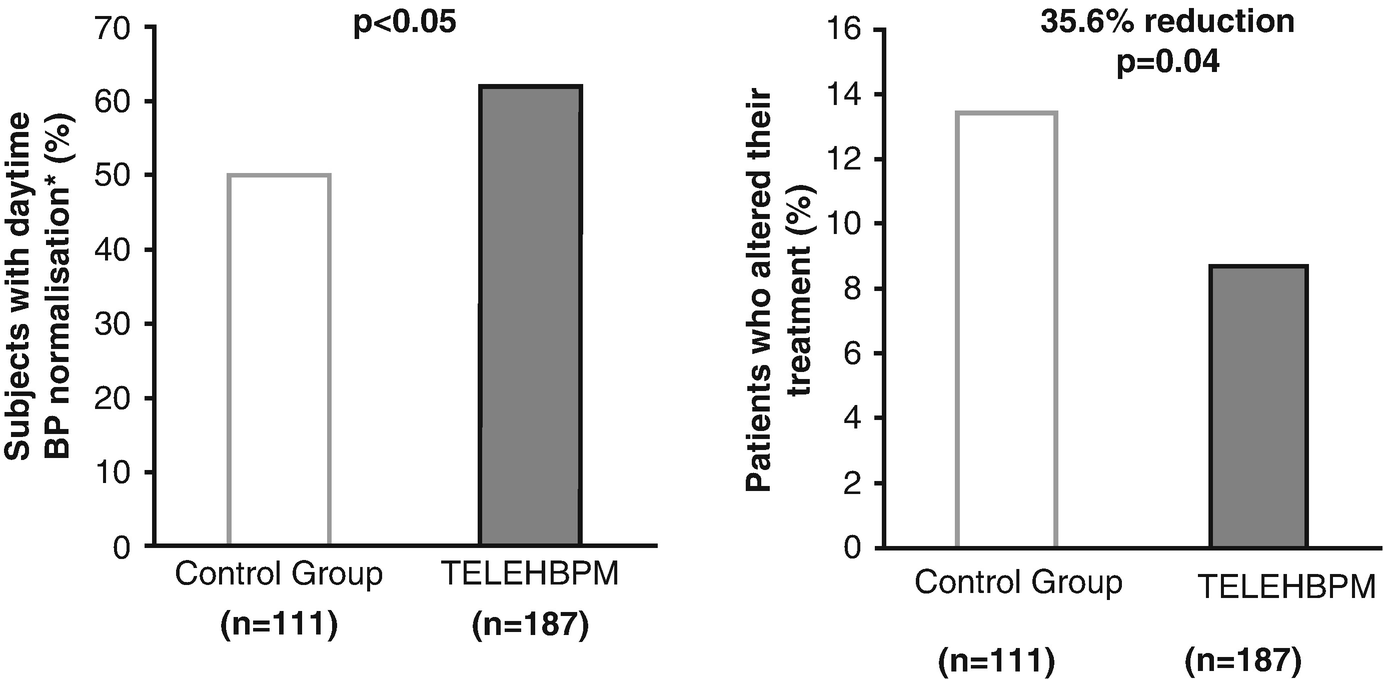
Percentage of patients with daytime ambulatory BP normalization (systolic BP <130 mmHg and diastolic BP <80 mmHg). In this study, hypertensive patients were randomized to be conventionally managed based on office BP measurement (withe bars, n = 111) or to be managed based on teletransmission of home BP values (gray bars: n = 187). Modified from Parati, et al. [4] by permission

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


