Chapter 4 Blood-pressure generation
After reading this chapter, you should:
Together with heart rate, pulsatile blood pressure is the most readily accessible measure of cardiovascular performance in humans. Blood pressure rises with sympathetic activation and this pressor response plays a vital role in optimizing blood flow to muscle and other vital organs during exercise. It is, therefore, important to spend a little time considering the factors that determine the limits of pressure pulsation and how these will be affected by increased sympathetic drive. The changes in blood pressure that occur during exercise will be examined in more detail in Chapter 7.
FACTORS AFFECTING BLOOD PRESSURE
Limits to blood pressure
Systolic pressure
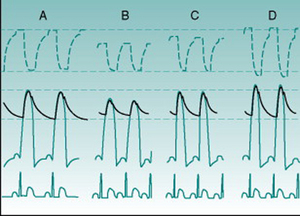
The extent to which blood pressure rises during systolic ejection reflects how much the energy of ejection is able to compress the arterial contents downstream of the left ventricle. The size of the stroke volume is, therefore, one obvious factor that will influence the level of systolic blood pressure (SBP). Anything that reduces stroke volume will reduce SBP (Fig. 4.1A,B). In normal individuals, the most usual situations in which this occurs is when cardiac filling falls because of an increase in heart rate or reduced venous return, typically during postural change.
Generalised sympathetic nervous system activation elevates SBP, due to a variety of factors. First, increased cardiac muscle contractility reduces end-systolic ventricular volume and increases stroke volume. Second, an increased action potential conduction velocity through the ventricular myocardium leads to faster compression of the contents and, therefore, to a higher velocity of ejection. In addition, the smooth muscle in the proximal aorta receives a sympathetic innervation and contraction of these muscle cells reduces aortic compliance. This stiffening allows all of the energy of ejection to be used in pressure generation. Finally, sympathetic vasoconstrictor drive to veins stiffens these and mobilizes blood normally stored in the venous reservoir back into active circulation, aiding cardiac filling and further increasing stroke volume. The additive effects of these factors are illustrated in Figures 4.1C and D.
Diastolic pressure
As diastolic blood pressure (DBP) represents the lowest value to which pressure falls in the arteries before the next systolic ejection, it must be influenced by the period over which the pressure can fall, so heart rate itself is also a major determinant of DBP, with tachycardia predictably causing a pressure rise (Fig. 4.1). Heart rate changes will also affect SBP if pulse pressure remains constant but, in practice, the consequences of heart rate alteration for ventricular filling time and, therefore, for stroke volume tends to minimize SBP changes.
The second main influence on DBP is the rate at which intra-arterial pressure falls after systolic ejection ceases; that is, how fast the pressurized blood flows out through the resistance of the peripheral blood vessels. Thus, the total peripheral resistance is a major determinant of DBP and changes in DBP can in many situations be used as an index of peripheral resistance changes. While all vascular beds and all segments of the vasculature contribute to the overall resistance of the system, most of the peripheral resistance occurs in the largest regional vascular beds, those supplying the digestive tract and associated tissues (the splanchnic circulation), the skeletal muscles, the skin and the kidneys, and almost all is localized to the arteriolar segment of the vasculature. In Chapter 5 (p. 50) we will see why the arterioles produce so much more resistance to flow than do other parts of the vascular tree.
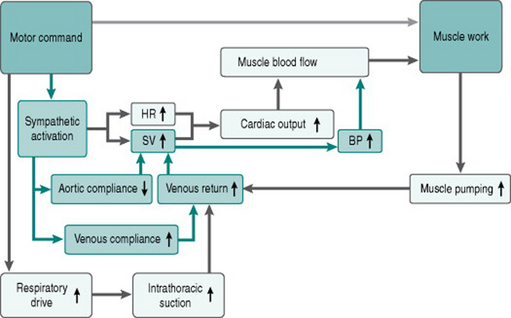
Figure 4.2 adds the effects of sympathetic activation on cardiac generation of blood pressure to our flow chart of the exercise response.
Mean versus phasic arterial pressure
As indicated above, the phasic limits of blood pressure can provide valuable information on the behaviour of specific components of the circulatory system. The pulsatile nature of pressure in large arteries is, however, irrelevant to perfusion of the peripheral tissues, since virtually all pulsatility is damped out by the time blood enters the capillaries. Also, calculation of parameters such as peripheral resistance requires an averaged value for pressure. The concept of mean arterial pressure is, therefore, essential to quantitative evaluation of circulatory function.
Does mean blood pressure change with heart rate?
or
With increasing heart rate, the shape of the BP wave changes so that the flatter late diastolic portion disappears and the waveform becomes more triangular. There is some experimental evidence suggesting that under these circumstances mean BP may be better approximated by DBP + 2/5PP (Robinson et al 1988).
Central and peripheral arterial pressures
The concept of arterial pressure generation from cardiac ejection and the factors determining systolic and diastolic limits as discussed above relate specifically to pressure just outside the semilunar valves. In the systemic circulation, however, additional factors become significant in pressure determination the further one moves away from the heart down the system of distributing arteries, with the result that absolute values recorded from, for example, arteries in the arm or leg, are no longer a precise reflection of the pressures in the aortic arch.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree