Fig. 7.1
Granular cell tumor with polygonal cells, granular eosinophilic cytoplasm, and uniform small nuclei is usually located under the bronchial mucosa within the endobronchial wall
Parenchymatous Tumors
While most of these tumors occur within the peripheral parenchyma of the lung, they are not restricted to these areas. Most of them are silent and only discovered incidentally during work-up for other diseases or screening for lung cancer. Some of them, like hamartoma, have characteristic radiologic features to make the diagnosis very accurate; others require tissue sampling to rule out malignancy, especially in cases with concurrent malignancies. Whenever there is limited material to make the diagnosis, the use of adjunct information from clinical and radiologic findings becomes paramount to avoid making the wrong diagnosis in these cases.
Pulmonary Hamartoma
This is a benign neoplasm composed of a mixture of mesenchymal elements such as cartilage, fat, connective tissue, and smooth muscle with entrapped epithelium. They present as incidental finding on imaging studies in older patients in the sixth decade. They are more common in males than females. They can be identified as such on imaging where they can be recognized as coin lesions with a “soap bubble” or “popcorn” appearance and with occasional calcification. They can be in the endobronchial wall producing symptoms of obstruction and rarely hemoptysis due to the tumor impinging on the endobronchial wall vessels [6].
Histologically, they are represented by lobules of cartilage and intervening fat and entrapped epithelium. In cytologic preparations, the material is usually represented by fragments of cartilage with scant other elements (Fig. 7.2). The aspirator will usually report that the lesion is hard and is well circumscribed. On modified Giemsa stain, the cartilaginous material can be appreciated with its magenta color.
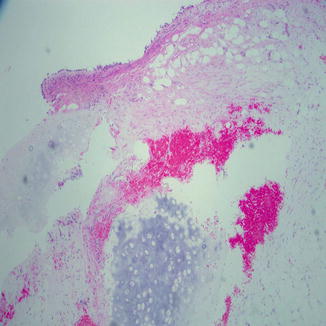
Fig. 7.2
Low-magnification view of a small biopsy illustrating the mixture of fat, connective tissue, and cartilage in a pulmonary hamartoma
On small biopsies, the presence of two mesenchymal elements helps in establishing the diagnosis. The presence of fat in close proximity to the cartilage in small biopsy should be enough to make the diagnosis. The lack of cytologic atypia and pleomorphism, along with the radiologic findings, should aid in establishing the benign nature of the lesion.
Alveolar Adenoma
Alveolar adenoma (AA) is a well-circumscribed lesion within the lung parenchyma. They are comprised of uniform cells of alveolar derivation. The size can be large (up to 6.0 cm), but the circumscription and slow rate of growth if interval radiologic evaluation is applied should reveal the benign nature of the lesion [7]. When the lesion is completely removed, the microscopic examination reveals cystic spaces lined with what would appear as type II pneumocytes. On a small biopsy specimen, the differential diagnosis would include adenocarcinoma in situ, adenocarcinoma with lepidic pattern, and pneumocytoma (sclerosing hemangioma). Immunoreactivity to TTF-1 and napsin A does not help in discerning the malignant or benign nature of the lesion [8]. Awareness of the radiologic findings and bland natures of the cells is important in working up these cases. Cystic spaces could be interpreted as emphysematous changes on a small-needle core biopsy. Again reviewing the radiologic findings is very helpful.
Papillary Adenoma
This is another tumor with a well-circumscribed outline and is an incidental finding in most cases. Radiologic imaging reveals a mass within the lung that could be in the differential diagnosis with malignant tumors.
On microscopic examination, the presence of papillary fronds is alarming for papillary carcinoma on cytologic material or needle core biopsies. It is important to pay close attention to the bland cytologic features, which contrasts with those of true papillary carcinoma of the lung where the nuclei have much more malignant features with vesicular nuclei having an irregular nuclear membrane and very prominent nucleoli [9] (Fig. 7.3). Papillary carcinoma of the lung is one of the most aggressive tumors among the adenocarcinoma subtypes. The papillary frond usually has an appreciable fibrovascular core, and there is no tertiary structure where the cells are piling up without a fibrovascular core (Fig. 7.4a, b).
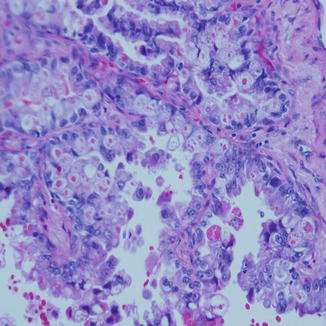
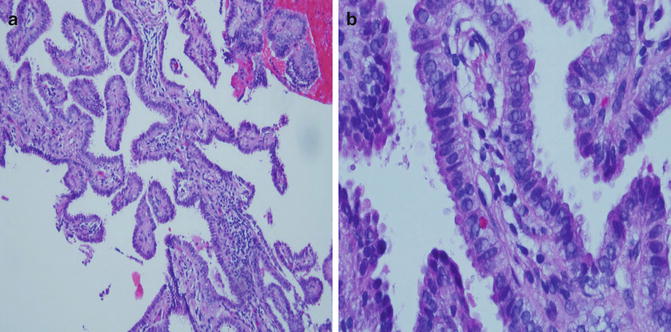
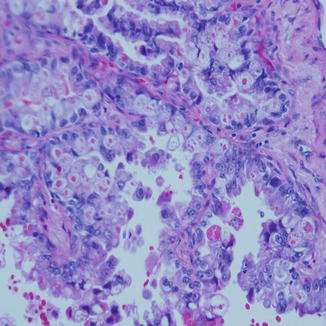
Fig. 7.3
Papillary carcinoma of the lung showing the delicate fibrovascular cores within the tumors and high-grade nuclear features. Large pleomorphic nuclei with prominent nucleoli are seen in a disordered pattern lining the fronds in contrast to Fig. 7.4
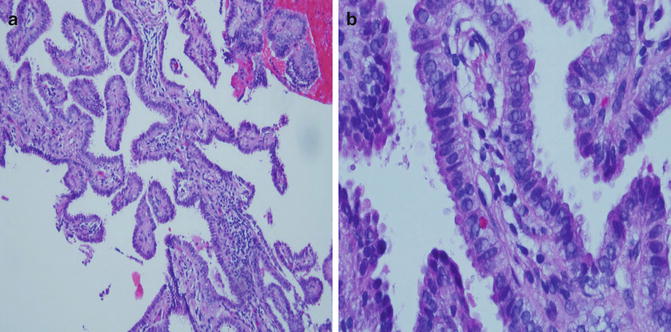
Fig. 7.4
(a, b) The fibrovascular cores of papillary adenoma are larger, and the lining cells have low-grade nuclear features with a streaming pattern. In (b) under higher magnification, the cells show apical snouts and frequent pseudoinclusions
Pneumocytoma “Sclerosing Hemangioma”
This is a tumor that was first described as an analog to a skin lesion because of the presence of blood lakes and hemosiderin within the tumor [12]. Later on, the histogenetic origin was proved to be from alveolar cells. The name has been controversial for decades, and recently Shimosato suggested the name pneumocytoma to correctly represent the cell of origin of this tumor as an uncommitted cell of the alveolar lining [13]. The tumor can occur at any age but it has a predilection to women with male to female ratio of 1:5. It can occur anywhere in the lung but usually it is in the periphery. It appears as a coin or oval lesion and it could be surrounded by a crescent or a rim of air around the lesion. It seldom shows any clinical symptoms and is discovered incidentally.
On microscopic examination when the tumor is completely resected, the circumscription is appreciated and there are two types of cells: one is similar to type II pneumocytes lining the alveolar spaces and the papillary fronds within the tumor (Fig. 7.5a, b). The others are a group of cuboidal cells representing the stroma or the interstitium within the lesion. Both types are polygonal or cuboidal in shape with uniform nuclei and a fair amount of cytoplasm. Clusters of foamy histiocytes or calcifications could be seen within the solid areas or within the papillary fronds. Hemosiderin could be seen deposited within the tumor or the area immediately next to it [14].
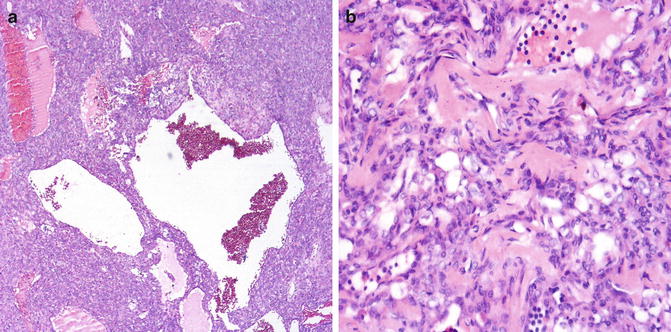
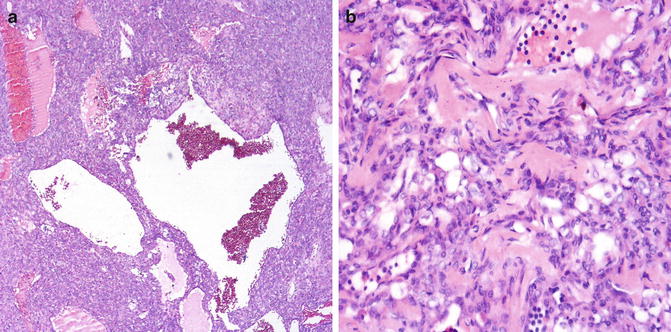
Fig. 7.5
(a, b) Pneumocytoma or the so-called sclerosing hemangioma shows a combination of lining cells and solid areas between cystic spaces (a). Blood lakes are noted in the spaces. Sclerotic areas are also present in (b), and in all instances the cells are similar in morphology and histogenesis
The problem is usually encountered either on frozen section or small biopsies and fine-needle aspiration biopsies. In these examples the differential diagnosis with adenocarcinoma in situ can be problematic. Correlation with history of smoking and imaging studies can avoid the overcall. It is also important to pay close attention to the cytologic morphology. The nuclei are rounded and the N/C ratio is low to moderate. The presence of nuclear pseudoinclusions should not be interpreted as a sign of malignancy because it is frequently encountered even in benign reactive type II pneumocytes.
The cells follow the same pattern of those derived from alveolar lining, being positive for TTF-1 and napsin A, CK7, and EMA. The tumor is negative for mesothelial markers WT-1, calretinin, and CK5/6. It is also negative for the neuroendocrine markers, synaptophysin, chromogranin, and CD56 [15].
Rarely, these tumors could metastasize to draining lymph nodes. However, even when they do, the course is indolent and the patient has been reported not to die from the disease.
Solitary Fibrous Tumor
Solitary fibrous tumors of the lung and pleura have been confused with mesothelioma because of the old name of “localized fibrous mesothelioma.” Later work proved these tumors to be of multipotent fibrous derivation from the subpleural fibrous tissue. They are considered of low malignant potential due to the fact that they can attain some features associated with malignancy like hypercellularity, increased mitotic activity (>4/10 HPF) with associated hemorrhage, and necrosis. In addition they can be locally aggressive and recur after excision.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


