Premature atrial complex
Blocked premature atrial complex (PAC) (again!)
DESCRIPTION
The first part of this is easy: if the beat is early it’s premature! The harder part (there always is a harder part) is what kind of a premature beat it is. Other than being able to correctly identify the beat when asked by the Chief Resident, it is clinically important to distinguish the various types of premature beats, as there may be different triggers involved, as well as different interventions (if any).
A premature ventricular complex (PVC, no, not the pipe) originates in the ventricle, and at times will send a P wave retrograde into the atrium where it can be seen, inverted, closely following the PVC itself. A PVC tends to be wide and look nothing like the normal beats, and most importantly, it is NOT preceded by a P wave.
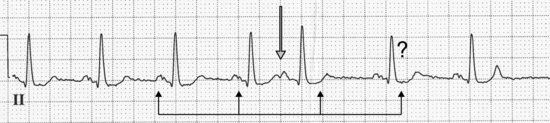
Probably the best way to help decide if a beat is a PVC or not is based on the fact that since PVCs arise in the ventricle, the sinus node usually doesn’t know an extrasystole occurred, so it keeps firing P waves right on time. That means that if you took your calipers or other measuring equipment (see page 18) you could march the P wave rhythm right through the PVC (see arrows) and the following P waves would be right on time (see above). Note I didn’t use the universally decried phrase “compensatory pause” even once, and I’m not going to! If you can show the underlying rhythm marches right through a premature beat that’s wide, you have pretty much proven it’s a PVC.
One last word of advice: if it looks like a PVC most of the time it is one, so don’t try to outsmart yourself.
What about premature atrial complexes (PACs)? If the beat is early, preceded by a P wave (open arrow), and looks like all the regular sinus beats, then it’s probably a PAC. A PAC arises somewhere within the atrium, not always near the sinus node, so the P wave of a PAC may not look like a sinus P wave. The P wave of a PAC may be hard to spot so you will need to look closely for them as they may be buried in the T waves of preceding beats. There are senior cardiologists who amuse themselves by pointing out 1–2 micron deflections on T waves and noting smugly “there’s the P wave”: if they are responsible for paying your salary or giving you a grade, nod politely and smile. Note that a PAC will usually “reset” the sinus node; that means the sinus node will be depolarized by the PAC and will resume its P to P interval from the PAC onward, so the previous P rhythm will usually NOT march through (see how the subsequent sinus beat is nowhere near where one would expect it to be if the sinus node kept firing unaffected by the premature beat, marked by the question mark).
Note that these ectopy rules are usually preceded by the qualifier “usually.” At this stage in your life you should know what that means!
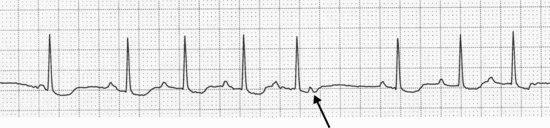
Although we already mentioned blocked PACs in the “Heart Block” section, their discussion really belongs here. A blocked PAC should be considered as exactly the same thing as a non-blocked PAC, with the same potential triggers. The most important thing about a blocked PAC is not to confuse it with a spontaneous sinus pause, as that might trick you into reducing or stopping medications which might otherwise be important. The key point here is that if you see a pause, look closely at the T wave of the preceding beat. If you actually find a P wave there that isn’t conducted the staff will look at you as if you were a hero.
Well, maybe not a hero, but they will be impressed.
HABITAT
These early beats can be found anywhere! If you attached a 24-hour monitor to anyone it would be extremely unusual not to find premature beats – and I mean all sorts: PACs, PVCs, couplets, bigeminy … you name it, they could be there! In certain habitats, however, you may find some types of extrasystoles more commonly than others. And like animals in a forest, some may be dangerous while others may not be. If an individual has a normal heart (no important valve or heart muscle disease) most premature beats you see won’t bite and are not poisonous. In other words, in the setting of no structural heart disease, if you see ventricular or supraventricular beats, they’re probably not dangerous and they won’t kill the patient. In the poor ejection fraction jungle, however, ventricular tachycardia and ventricular fibrillation are lurking in the undergrowth: ventricular extrasystoles are bad players, especially if a few group themselves together (three or more in a row is ventricular tachycardia). In the acute coronary syndrome PVCs are ominous, especially the evil R-on-T beat, where the PVC is so early it lands on the T wave of the preceding normal beat.
In the marshes and swamps of chronic lung disease we are more likely to find PACs, possibly harbingers of more sustained supraventricular arrhythmias; we probably have right atrial stretch to thank for these beasts (or should I say, beats?).
In any setting, and no matter what the beats, if you suddenly see an increase of these creatures, you should search for a cause: abnormal electrolytes, ischemia, drug toxicity, low oxygen, too much vodka, an unexpected marriage proposal, etc.
CALL
Varied, depending on the habitat. In a Holter lab: “These #@%*! beats are taking me too long to scan this tape!”
Medical telemetry floor: “What the #@%*! are all these beats? Call the CCU!”
CCU: Either “ What the #@%*! are all these beats? Call the cardiologist!” or “Get the amiodarone!”
Cardiologist: “Hmm … these are either #@%*! ventricular or supraventricular beats, where are my calipers?”
Electrophysiology lab in patient with an ejection fraction less than 30%: “Who cares what these #@%*! beats are, get the implantable defibrillator!”1
RESEMBLANCE TO OTHER ARRHYTHMIAS
The big challenge is to decide whether the premature beats are ventricular, supraventricular, or nodal/junctional. You can refer to the points raised in the “Description” section described above, resort to calipers (making sure your tetanus vaccinations are up to date), or simply and authoritatively state that the wide beats are PVCs, the narrow beats preceded by P waves are PACs, and the narrow beats not preceded by P waves are premature junctional/nodal complexes. You’ll be right most of the time, and if you’re authoritative enough no one will dare question you.
CARE AND FEEDING
Here, as in most cases, how to feed these rhythms depend on their environment. In other words, if the premature beats are occurring in a non-dangerous setting (normal heart, normal ejection fraction, no ischemia) they’ll generally do just fine on their own. But we would suggest a search for triggers, especially if the extrasystoles are new or increasingly frequent: check potassium, magnesium, thyroid levels, oxygen levels, toxic drugs, pain, etc. – and then treat the underlying problem.
1 If you didn’t notice, mixed in with all the profanity was a footnote! Moss AJ, Zareba W, Hall WJ, et al. Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N Engl J Med 2002;346:877–83.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


