1 Basics of Percutaneous Coronary Interventions
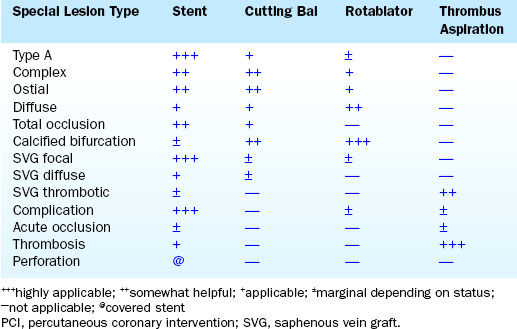
This chapter is the extension of the PCI chapter from The Cardiac Catheterization Handbook, fifth edition, and presents the basic method and mechanisms of balloon angioplasty and stenting as an introduction to the practice of interventional cardiology. The various techniques of PCI can be placed into niche applications for specific devices (Table 1-1).
Overview of the Basic PCI Method
Steps in the PCI Procedure
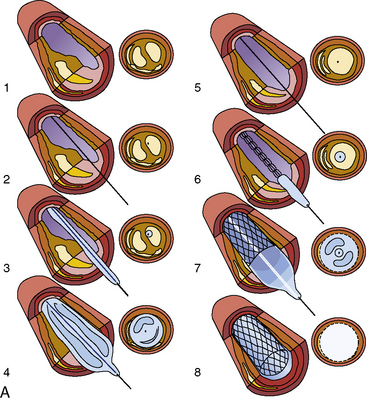
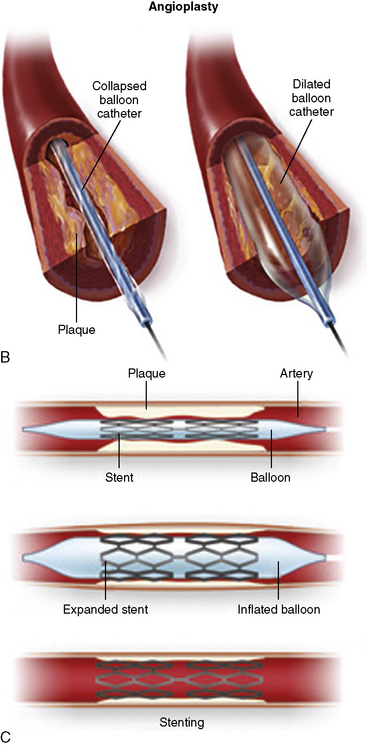
The steps in the PCI procedure are shown in Figure 1-1. First, a guiding catheter is seated in the coronary ostium. A thin, steerable guidewire is introduced into the guide catheter and then into the coronary artery and positioned across the stenosis into the distal aspect of the artery. A very small angioplasty balloon catheter is placed on the guidewire, inserted through the guiding catheter, and is positioned in the artery across the stenotic area by tracking it over the guidewire. Once correctly placed within the narrowed area to be treated, the balloon on the PCI catheter is inflated several times for brief periods (10–60 seconds). The inflation and deflation of the balloon expand the stenosis and restore blood flow to an area of the heart previously deprived by the stenosed artery.
After the stent struts have been expanded and implanted into the artery wall, the balloon is deflated, and the delivery catheter and guidewire are removed. Intravascular ultrasound (IVUS) imaging is often used to confirm appropriate vessel-stent matching and full stent strut apposition (contact without space against the wall). After IVUS and final angiography have been performed, the guide catheter is removed. The femoral or radial arterial sheath is removed, and hemostasis is obtained in the laboratory. The patient is then transferred to a recovery area and then to the patient’s room. If no complications occur, the patient is discharged the next morning. The patient usually returns to work shortly (<2 days) thereafter. The definitions of a successful PCI procedure are summarized in Table 1-2.
Table 1-2 Definitions of PCI Success
Mechanisms of Angioplasty and Stenting
Indications for PCI
In general, PCI is indicted for patients with the following:
• Stable angina pectoris unrelieved by optimal medical therapy with objective evidence of ischemia (abnormal stress test or abnormal stress thallium) and a coronary lesion in a vessel supplying a large area of myocardium
• Angina pectoris after CABG surgery
• Symptomatic restenosis after previous PCI
• Relative contraindications to PCI
• Unsuitable coronary anatomy (e.g., multiple severe complex lesions or diffuse distal disease)
• High-risk coronary anatomy in which closure of vessel would result in death
Contraindications to PCI
• Bleeding diathesis (low platelet count, peptic ulcer disease, coagulopathy, etc.)
• Patient noncompliance with procedure and post-PCI instructions and inability to take dual antiplatelet therapy (acetylsalicylic acid [ASA], Plavix, etc.)
PCI Equipment
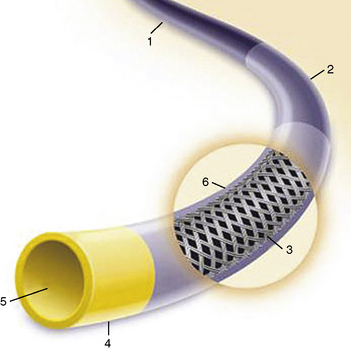
The most commonly used PCI equipment consists of four basic elements: a guiding catheter, a balloon catheter, a coronary guidewire, and a stent (Fig. 1-2 and Table 1-3 list approximate costs of such equipment).

Figure 1-2 Diagram of components of percutaneous coronary intervention equipment.
(Adapted from Safian RD, Freed MS, eds. The manual of interventional cardiology, 3rd ed. Birmingham, MI: Physicians’ Press, 2001.)
Table 1-3 Approximate Costs of Coronary Angioplasty Equipment
| Equipment | Cost ($US) |
|---|---|
| Balloon dilatation catheter | 300 OTW/250 Rx |
| Guiding catheter | 65 |
| Guidewire | 80 |
| Exchange guidewire (300 cm) | 120 |
| Indeflator | 55 |
| Y connector | 31 |
| Sheath introducer | 8 |
| Torque tool | 18 |
| Nonballoon devices | |
| Stent (noncoated) | 1300 |
| Stent (drug-eluting) | 2300 |
| Rotablator | 1330 |
| IABP | 840 |
IABP, intra-aortic balloon pump; OTW, over-the-wire; Rx, rapid exchange.
Guiding Catheter
A special large-lumen catheter is used to deliver the coronary balloon catheter and other interventional devices to the vessel that contains the lesion to be dilated. The features of the guide catheter noted in Figure 1-3 differentiate it from diagnostic catheters.
Functions
A guiding catheter serves three major functions during angioplasty:
Backup Support for Balloon Catheter and Stent Advancement
The improved quality and size of currently used stents have reduced the need for robust backup support in most situations. For more complex and technically difficult lesions, the choice of an appropriate guiding catheter for extra support and lesion visualization remains essential (see Chapter 3). When there is insufficient backup in crossing a very tight stenosis, the guiding catheter will disengage from the coronary ostium and back out into the aortic root. When pressure is applied to the stent catheter during attempts to cross the lesion, repositioning the guide catheter in a stepwise fashion while the stent is advanced may overcome this loss of support. However, aggressive intubation of the coronary ostium may damage the vessel, stopping the procedure prematurely, or may require additional stenting for an ostial dissection.
Characteristics
Compared with the diagnostic catheters, the guiding catheters have thinner walls, larger lumens, and stiffer shafts (Fig. 1-3). A large catheter lumen is achieved at the expense of catheter wall thickness and thus may result in decreased catheter wall strength, less torque control, or catheter kinking. The guiding catheters are generally stiffer to provide backup support during the PCI catheter advancement into the coronary artery and, therefore, respond differently to manipulation than diagnostic catheters. The guiding catheter tip is not tapered. Pressure-wave damping upon engaging the coronary ostium is seen more often than with similar-sized diagnostic angiographic catheters. Some guide catheters have relatively shorter and more flexible tips to decrease catheter-induced trauma.
Balloon Dilatation Catheter Systems
Types
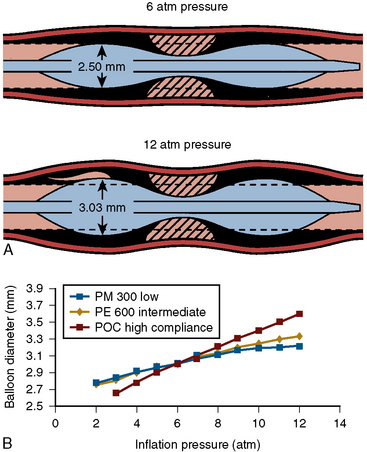
There are three types of PCI balloon catheters (Fig. 1-4):
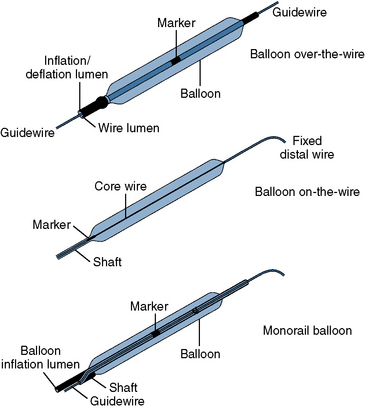
Figure 1-4 Three common types of coronary balloon angioplasty catheter design.
(Adapted from Freed MS, Grines C, eds. New manual of interventional cardiology. Birmingham, MI: Physicians’ Press, 1992: 29.)
The OTW and monorail balloons, but not fixed-wire balloons, are also used to deliver stents that are mounted by the manufacturer on a specific balloon. The advantages and limitations are summarized in Table 1-4.
Table 1-4 Advantages and Limitations of Angioplasty Balloon Types
| Advantages | Limitations |
|---|---|
| Over the wire | |
| Distal wire position | Two experienced personnel required |
| Distal port available for pressure measurement or contrast media injection | Larger profile |
| Accepts multiple guidewires | |
| Rapid exchange | |
| Distal wire position Enhanced visualization Low-profile balloons Single-operator system | Exchanging balloons at hemostatic valve may be technically demanding |
| Fixed wire | |
| Enhanced visualization | Lack of through lumen |
| Single-operator system | Inability to recross lesion without removing |
| Use with small guiding catheters system | |
| Low-profile balloons | |
Modified from Kern MJ, ed. The cardiac catheterization handbook, 2nd ed. St Louis, MO: Mosby, 1995.
OTW Angioplasty Balloon Catheters
Historically, the OTW balloon was the first introduced and has remained popular in a few centers. A standard OTW angioplasty balloon catheter has a central lumen throughout the length of the catheter for the guidewire and another, separate lumen for balloon inflation (Fig. 1-5). These balloons are approximately 145 to 155 cm long and are designed to be used with guidewires of various dimensions (0.010–0.014 inches). The major OTW advantage is the ability to maintain distal artery access with the balloon beyond the lesion while one guidewire is exchanged for another. The OTW system tracks very well because the whole balloon length has a wire lumen. It permits long guidewire exchanges, and because of the through lumen, it allows for delivery contrast and drugs distally in an artery. To exchange PCI catheters, the balloon is advanced over the wire to a distal position. The standard short (145-cm) wire is then removed from the balloon. A longer guidewire (300 cm) is then inserted to maintain distal wire position while the balloon catheter is completely withdrawn over the guidewire and another balloon catheter is introduced over the same long guidewire for additional dilatations. OTW catheters can accept multiple guidewires, which allows for exchanging additional devices that may require stronger, stiffer, or specialized guidewires.

Figure 1-5 Typical over-the-wire balloon (OTW) catheter. Quantum Maverick OTW. OTW “Quantum” Maverick Balloon.
(Courtesy SciMed-Boston Scientific, Boston, MA.)
Rapid-Exchange (Monorail) Balloon Catheters
“Rapid-exchange” or monorail catheters were developed to permit the exchange of angioplasty balloon catheters by a single operator. Rapid-exchange catheters have only a short (30–40 cm) length of the catheter shaft containing two lumens (Fig. 1-6). One lumen, in the distal 30-cm portion of the catheter shaft, houses the guidewire. The remaining lumen runs the entire length of the catheter and is used for balloon inflation. Because only a limited portion of the balloon requires dual lumens, rapid-exchange catheters are smaller in diameter than are OTW balloon catheters.

Figure 1-6 Typical rapid-exchange or monorail balloon catheter. Maverick 2 Monorail. Monorail balloon catheter.
(Courtesy SciMed-Boston Scientific, Boston, MA.)
Characteristics
The mechanical aspects of balloon inflations apply the following fundamental principles: