Answer 10: C. Answer A is a correct statement since the PRF is greatly dependent on the time to transmit and receive an ultrasound burst. Since the speed of sound is relatively fixed, the most important variable is the depth of the image.
Answer B is a correct statement since more lines of data are necessary to create and maintain an adequate image quality as the sector increases.
Answer C is the least accurate statement since 2 lines/degree are necessary to obtain high-quality images, and it would be prohibitively long to obtain 200 lines/degree.
Answer D is a correct statement. To increase the frame rate, the line density is compromised, and therefore, the image quality degrades.
Answer E is a correct statement. This concept is increasingly important as one tries to compare tissue Doppler velocities obtained from two distinct techniques. Since color coding measures mean velocities, these measures will be inherently lower than if pulsed-wave Doppler measures were obtained.
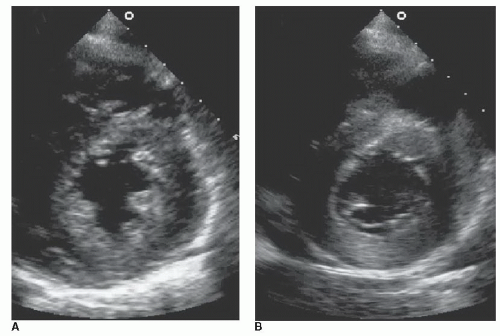
A number of variables must be considered when creating a 2D image. The depth of the examination, the pulse repetition frequency (PRF), the line density, and frame rate each conspire to result in a high-quality image. After sending in a burst of ultrasound, the returning signal must be received, and this is mostly a function of the depth of transmission. Each ultrasound pulse provides a single raster line of data, and the rate that the pulses are transmitted is the PRF. To obtain a 2D image (as opposed to a single-dimensional M-mode image), the ultrasound beam needs to sweep through an angle. The greater the line density, the higher the spatial resolution and image quality. More data lines are needed to fill larger sectors. A line density of approximately two lines per degree is usually adequate to construct a high-quality image. Line density can be increased by decreasing the sector width (same # lines per smaller region), reducing the frame rate (more time for building lines/frame), and reducing the depth (shorter lines = shorter time to build).
The total ultrasonic data recorded during one complete sweep of the ultrasound beam are termed a “field.” The sum of imaging data recorded is a frame. Two fields are interlaced (to improve line density) to produce one frame, and therefore, the frame rate is half of the sweep rate.
Color-flow Doppler (CFD) imaging is a form of pulsed-wave Doppler imaging. CFD uses multiple sample volumes along multiple raster lines to record the Doppler shift at multiple locations. This information is placed on top of a two-dimensional image display, but only the mean frequencies and frequency spreads (variance) are obtained to save processing (Fourier transform) time.