Chapter 39
Basic Life Support and Advanced Cardiac Life Support
Vissia S. Pinili, MSN, RN, CPAN, CCRN, Nicole R. Keller, PharmD, BCNSP and Glenn N. Levine, MD, FACC, FAHA
1. Why was the A-B-C (airway, breathing, compression) sequence of cardiopulmonary resuscitation (CPR) changed to C-A-B (compression, airway, breathing)?
2. What factors constitute “high-quality CPR”?
Components of high-quality CPR include:
 Chest compressions at least 100 times per minute
Chest compressions at least 100 times per minute
 Depth of chest compressions for adults of at least 2 inches (5 cm), for children compressions of 2 inches, and for infants compressions of 1.5 inches (4 cm)
Depth of chest compressions for adults of at least 2 inches (5 cm), for children compressions of 2 inches, and for infants compressions of 1.5 inches (4 cm)
 Allowing for complete chest recoil after each compression
Allowing for complete chest recoil after each compression
 Minimizing interruptions in chest compressions
Minimizing interruptions in chest compressions
3. What is your first step if you are alone and come across an unresponsive adult victim with no signs of breathing?
Figure 39-1 is an algorithm for adult basic life support (BLS) decisions and actions. A summary of key BLS components for treating adults, children, and infants is given in Table 39-1.
TABLE 39-1
SUMMARY OF KEY BASIC LIFE SUPPORT COMPONENTS FOR ADULTS, CHILDREN, AND INFANTS
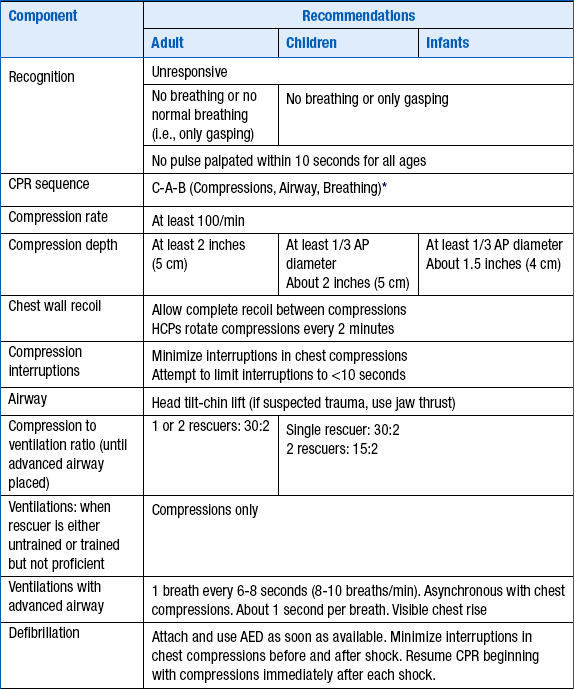
∗Excluding the newly born, in whom the etiology of an arrest is nearly always asphyxia.
From American Heart Association: Highlights of the 2010 American Heart Association Guidelines for CPR and ECC. Available at : http://www.heart.org/idc/groups/heart-public/@wcm/@ecc/documents/downloadable/ucm_317350.pdf. Accessed March 26, 2013.

Figure 39-1 Adult basic life support (BLS) algorithm. AED, Automated external defibrillator; CPR, cardiopulmonary resuscitation.
4. For patients with respiratory arrest (but with a perfusing heart rhythm), how often should breaths be delivered?
5. What is the most common cause of airway obstruction in the unconscious adult patient?
6. How many joules of energy are indicated for the treatment of ventricular fibrillation (VF) or pulseless ventricular tachycardia (VT) when using a biphasic defibrillator?
Biphasic defibrillators are now used at many institutions, replacing the older monophasic defibrillators. The amount of energy will often be device specific, ranging from 120 to 200 J. If the appropriate setting is unknown, use 200 J. Additional shocks should be equivalent or higher energy. This contrasts to the older monophasic defibrillators, for which a setting of 360 J is recommended.
7. In order, what are the preferred routes of drug administration?
 Intravenous (IV) is the preferred route of drug administration. The guidelines emphasize that resuscitation attempts should not be delayed by trying to achieve central IV access when peripheral IV access can be easily achieved.
Intravenous (IV) is the preferred route of drug administration. The guidelines emphasize that resuscitation attempts should not be delayed by trying to achieve central IV access when peripheral IV access can be easily achieved.
 When IV access is not possible, intraosseous (IO) is preferred over endotracheal (ET). The IO route can be used in both children and adults.
When IV access is not possible, intraosseous (IO) is preferred over endotracheal (ET). The IO route can be used in both children and adults.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



