Basic Diagnostic Studies
“Absence of evidence is not evidence of absence”
Electrocardiography
Numerous excellent textbooks on electrocardiography have been written, and this section is not intended to compete with or replace those textbooks. However, those textbooks may be a bit challenging for the medical student, family practice, or general pediatric resident. This chapter includes the essentials of cardiac rhythm analysis and treatment.
For each rhythm displayed, there is a brief comment about the treatment. One must recognize that the treatment of pediatric arrhythmias has become very complex. Indeed, pediatric electrophysiology is a specialty by itself. Therefore, the comments about treatment will be tailored to immediate rather than long-term treatment.
It is essential that all clinicians have the ability to determine the cardiac rhythm from an electrocardiographic tracing. Although it may be possible to determine the rhythm from a strip chart recording obtained from an electrocardiogram (ECG) monitor, one will make fewer errors if the interpretation is based upon a 12-lead surface ECG.
Cardiac Rhythm
The rhythm is sinus if there is a P wave in front of every QRS and if the P wave is upright in leads I and aVF (see Figure 3.1).
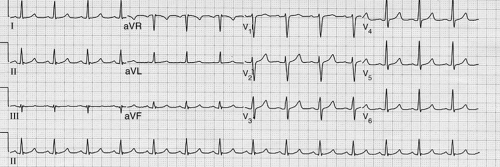
Figure 3.1 • Sinus rhythm. This rhythm is indicated when there is a P wave in front of every QRS and if the P wave is upright in leads I and aVF
The rhythm is low right atrial if there is a P wave in front of every QRS but if the P wave is upright in lead I and inverted in lead aVF (see Fig. 3-2). This is not an abnormal rhythm. It is a variant of normal and requires no special evaluation or treatment.
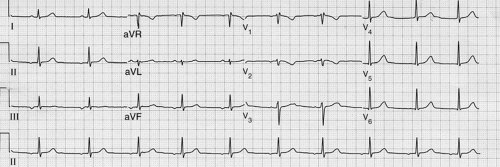
Figure 3.2 • Low right atrial rhythm. This is indicated if there is a P wave in front of every QRS but the P wave is upright in lead I and inverted in lead aVF
The rhythm is left atrial if there is a P wave in front of every QRS and the P wave is inverted in lead I (see Fig. 3-3). This rhythm can be associated with situs inversus totalis, in which the morphologic right atrium and the normal sinus node are to the left of the left atrium. In this case, the rhythm requires no treatment. A left atrial rhythm can also occur with normal situs when a left atrial electric focus supplants the normal sinus rhythm. In the absence of a left atrial ectopic focus tachycardia associated with this condition, no treatment is required.
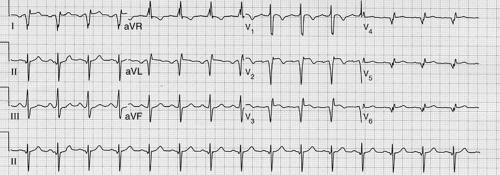
Figure 3.3 • Left atrial rhythm. This is indicated if there is a P wave in front of every QRS and the P wave is inverted in lead I.
The rhythm is junctional if there is no P wave in front of the QRS and if the QRS is narrow (<80 msecond; two small boxes) (see Fig. 3-4). Usually, junctional rhythm is slower than the expected sinus rate. Intermittent junctional rhythm can be normal, especially during sleep.
The treatment for junctional rhythm in the absence of any sinus rhythm may involves insertion of a pacemaker. However, it is difficult to identify patients who require a pacemaker.
When junctional rhythm is a complication of cardiac surgery, most experts recommend insertion of a pacemaker. If junctional rhythm is particularly slow or is associated with symptoms of lightheadedness or syncope, insertion of a pacemaker is indicated.
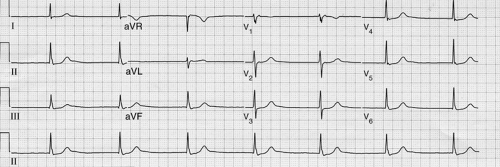
Figure 3.4 • Junctional rhythm. This is indicated if there is not a P wave in front of the QRS and the QRS is narrow (<80 msecond; two small boxes).
If there is no P wave in front of the QRS and if the QRS is wide (>120 msecond), the rhythm likely is originating distal to the His bundle (see Fig. 3-5). The rhythm most likely is ventricular in origin. Alternatively, the rhythm could be originating from the junction if there is bundle branch block.
The treatment of this condition depends upon many factors. Firstly, one must determine whether the rhythm is junctional with aberrant conduction or is ventricular or fascicular in origin. If a previous ECG is available when the patient was in sinus rhythm and if the morphology of the QRS complex in sinus rhythm is identical to that when there is no sinus rhythm, then the rhythm is junctional and treated accordingly (see preceding text).
Secondly, if the rhythm is ventricular or fascicular, its cause must be determined. The causes of ventricular or fascicular rhythms include myocarditis, electrolyte imbalance, long–QT-interval syndrome, Brugada syndrome, and myocardial ischemia, among others. The treatment will depend upon the underlying cause but might include correction of metabolic abnormalities causing the arrhythmia, drugs to suppress the rhythm, and/or an implantable cardiac defibrillator (ICD).
There is a condition of benign ventricular tachycardia (VT) of childhood that requires no treatment. However, before arriving at this diagnosis, all other causes of ventricular rhythms must be excluded.
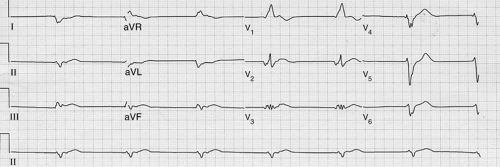
Figure 3.5 • Rhythm likely originating distal to the His bundle. This is indicated if there is no P wave in front of the QRS and the QRS is wide (>120 msecond).
Tachyarrhythmias exist if the heart rate is faster than it should be on the basis of the patient’s activity. For example, a heart rate of 180 beats per minute is normal for a 14-year-old engaged in vigorous exercise but is abnormal if the child is resting. Tachyarrhythmias can be classified into supraventricular tachycardia (SVT), junctional tachycardia (paroxysmal junctional tachycardia [PJT] or junctional ectopic tachycardia [JET]), and VT.
In SVT, the QRS is narrow, and P waves, if discernible, will be related to the QRS (see Fig. 3-6). Treatment of SVT can be divided into (i) immediate treatment to terminate the episode of SVT and (ii) treatment to prevent its recurrence.
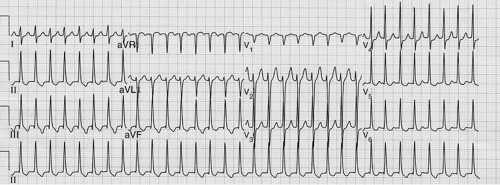
Figure 3.6 • The electrocardiogram in SVT. The QRS is narrow, and P waves, if discernible, are related to the QRS.
There are several ways to terminate SVT. Because it is rarely life threatening, one can wait an hour or two for SVT to terminate on its own. The patient may be able to terminate SVT by doing a Valsalva maneuver, such as bearing down against a closed glottis and straining as if having a bowel movement. Carotid massage can be tried. Swallowing ice water will sometimes terminate SVT. If none of these works, immersing the patient’s face in ice water may be effective but it is very uncomfortable. One of the most effective pharmacologic methods to terminate SVT is the intravenous use of adenosine. For the rare patient who is hemodynamically unstable while in SVT, electrical cardioversion is perhaps the best choice of treatment.
There are a variety of options to prevent recurrence of SVT. These include β-blockers, calcium channel blockers, amiodarone, and ablation of the atrial focus or the reentry circuit that is responsible for the arrhythmia. β-Blockers are certainly a safe choice. The use of other treatment methods should be guided by a cardiologist.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


