Understanding the perspective of early-career cardiologists is important to design effective responses to the challenges in modern cardiovascular (CV) training programs. We conducted a web-based survey on a total of 272 early-career cardiologists (within 10 postgraduate years) who registered for the 2011 annual Japanese Circulation Society Meeting. Main outcome measures were satisfaction with their training, confidence in their clinical skills, and professional expectations, scaled from 0 to 10. The median training time was 6 years, with 2 years for internal medicine and 4 years for CV disease. Most received their training in university hospitals at some point during their career (79.5%) and were interested in a subspecialty training, such as interventional cardiology (38.6%), electrophysiology (15.1%), and advanced heart failure (10.3%); only 9.6% showed interest in general cardiology. The respondents felt comfortable in managing common CV conditions such as coronary artery disease (average score 6.3 ± 2.4 on an 11-point Likert scale) but less so in peripheral arterial disease (3.8 ± 2.8), arrhythmias (3.7 ± 2.3), and congenital heart disease (2.9 ± 2.2). Their satisfaction rate with their CV training positively correlated with their clinical proficiency level and was associated with volume of coronary angiograms, percutaneous coronary interventions, and echocardiograms completed. In conclusion, the current young cardiologists have a positive perception of and interest in procedure-based subspecialty training, and their training satisfaction was related to volume of cardiac procedures. Additional effort is needed in enforcing the training in underappreciated subspecialty areas.
In recent years, the satisfaction of medical trainees (i.e., residents and fellows) with training and their perspective have been the subject of much research to provide reliable information for the outcome of the training system. This is of no exception in cardiovascular (CV) training, and the program faces the need to identify the imbalance in volume and composition of the training system and assess its appropriateness through the perspective of the medical trainees. The CV-training programs are facing additional challenges; advances in medical treatment, intensive care, and noninvasive diagnosis in cardiology have led to an increasing demand for a complex system that provides residents with knowledge and skills required for diverse subspecialties. However, the perspective of trainees in CV medicine and their self-assessed confidence level is unknown. There has been much research on resident perspectives and satisfaction within other specialties. Factors such as operating experience, quality of the attendant’s teaching, interaction with attendants during patient care, and substantial citing of evidence-based literature were associated with residents’ satisfaction in their training programs. Our primary goal was to analyze and understand job-satisfaction levels and their factors for early-career cardiologists.
Methods
This study is based on an analysis of data from a survey of CV trainees in Japan registered to attend the Japanese Circulation Society annual meeting scheduled in March 2011. Two hundred seventy-two trainees, who graduated all within 10 years, completed the web-based anonymous survey on registration.
The details of the survey questionnaire are provided in the online supplement . The survey included questions across a wide number of variables. Questions related to current employment included hospital information, scholarly activity, satisfaction in current job environment, current annual salary, and clinical proficiency and satisfaction level in subspecialty management and imaging studies. Questions related to education and training included past training patterns regarding hospital type and specialty (general internal medicine, clinical cardiology, basic cardiology); obtaining specialist qualifications and PhD; areas of interest in CV subspecialty; experience of cardiology procedures; and length of career since graduation from medical school.
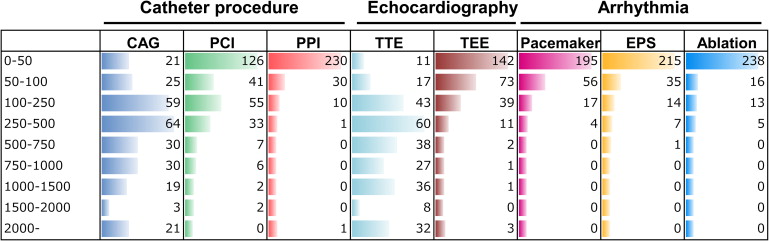
Trainees were queried regarding the number of cardiology procedures they performed as a primary operating physician. The procedures included coronary angiogram, percutaneous coronary intervention, percutaneous peripheral intervention, electrophysiological study, catheter ablation, transthoracic echocardiogram, transesophageal echocardiogram, implantation of pacemaker, implantable cardioverter defibrillator, and cardiac resynchronization therapy(-defibrillator). Each item had 9 categorical choices for procedure volume.
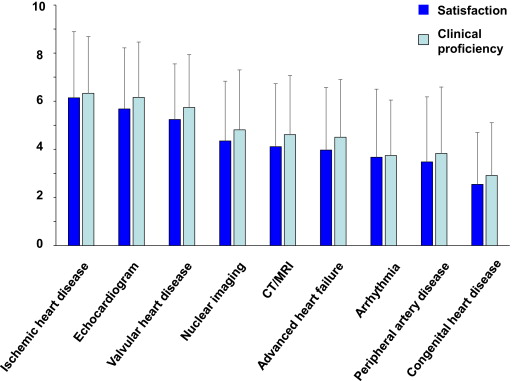
Clinical proficiency level was assessed with 9 items based on an 11-point Likert scale (i.e., 0 = “never done before” to 10 = “able to handle all by myself through the end”). Items evaluated were management of ischemic heart disease, arrhythmia, severe heart failure, peripheral artery disease, valvular heart disease, congenital heart disease, and imaging studies (echocardiogram, nuclear studies, and computed tomography/magnetic resonance imaging). Trainees were asked to rate their satisfaction level with their training in same 9 items by using an 11-point Likert scale (i.e., 0 = “dissatisfied, complete lack of experience” to 10 = “satisfied, gained enough experience”).
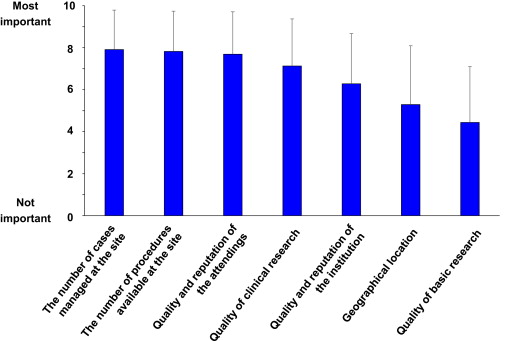
Participants were asked to rate the most important factors in their program choice. On a 0 to 10 scale (i.e., 0 = “not important at all” to 10 = “most important”), important cardiology training facility variables included hospital location, volume of patients and procedures, faculty and facility quality/reputation, and clinical and basic experimental research quality.
Continuous data were summarized as mean values ± SD and discrete data as absolute values and percentages. Data were analyzed using SPSS statistical software (SPSS Inc., Chicago, Illinois). Overall satisfaction score was calculated as the sum of satisfaction levels in each subspecialty. This reflected satisfaction with career training in the management of 6 CV fields (ischemic heart disease, valvular heart disease, advanced heart failure, arrhythmia, peripheral artery diseases, congenital heart diseases) and 3 noninvasive imaging studies (echocardiogram, nuclear studies, and computed tomography/magnetic resonance imaging). Logistic regression analysis was used to assess the association (reported as odds ratios and 95% confidence intervals) of trainee satisfaction with various factors, including clinical proficiency, procedure volume, scholarly activity, and obtaining cardiology board qualification or MD/PhD dual physician-scientist degree.
Results
Baseline characteristics of the 272 responding participants are shown in Table 1 . One hundred forty-five participants (53%) identified themselves as currently working in university hospitals and 112 (41%) in community hospitals. Most received their training in academic university hospitals at some point during their career (79.5%). The 3 most selected areas of interest in CV medicine were management of ischemic heart disease, arrhythmia, and advanced heart failure. Only 9.6% selected general cardiology as their area of interest ( Table 2 ).
| Type of current training facility | |
| University hospital | 145 (53%) |
| Community hospital | |
| <200 beds | 16 (6%) |
| 200–500 beds | 59 (22%) |
| 500–beds | 37 (14%) |
| Others | 15 (6%) |
| Total training duration (years) | 7.6 ± 2.1 |
| Training duration, type of specialty (years) | |
| General internal medicine | 2.1 ± 1.1 |
| Clinical cardiology | 3.9 ± 2.3 |
| Basic cardiovascular research | 2.7 ± 2.3 |
| Training duration, type of training facility (years) | |
| Community hospital | 3.6 ± 0.4 |
| University hospital, clinical training | 2.7 ± 2.4 |
| University hospital, basic science | 1.5 ± 1.8 |
| Cardiology board qualification | 134 (49%) |
| Presentation at scientific meeting | |
| Basic science research | 90 (33%) |
| Clinical science research | 236 (87%) |
| Publication of peer-reviewed article | |
| Basic science research | 50 (18%) |
| Clinical science research | 114 (42%) |
| Annual salary | |
| <6,000,000 JPY ∗ | 31 (11%) |
| 6,000,000–10,000,000 JPY ∗ | 130 (48%) |
| 10,000,000–JPY ∗ | 99 (36%) |
| Unanswered | 12 (4%) |
| Interest of Area | |
|---|---|
| Ischemic heart disease (including interventional cardiology) | 105 (38.6%) |
| Arrhythmia (including electrophysiological study and catheter ablation) | 41 (15.1%) |
| Advanced heart disease (including management of left ventricular assistant device and heart transplantation) | 28 (10.3%) |
| General cardiology | 26 (9.6%) |
| Imaging study; echocardiogram | 25 (9.2%) |
| Basic research | 18 (6.6%) |
| Imaging study; computed tomography/magnetic resonance imaging | 9 (3.3%) |
| Valvular heart disease | 4 (1.5%) |
| Imaging study; nuclear study | 3 (1.1%) |
| Congenital heart disease | 2 (0.7%) |
| Other | 11(4.0%) |
In terms of current job environment, 55 residents (20%) were “satisfied,” 107 (39%) were “somewhat satisfied,” and 20 (7%) were “dissatisfied.” The response of “satisfied” or “somewhat satisfied” was significantly greater among the participants in nonuniversity hospitals than those in university hospitals (73% vs 53%, p = 0.003). Notably, the participants who responded “satisfied” or “somewhat satisfied” had similar training periods compared with their counterparts (CV medicine training; 4.2 ± 2.3 vs 3.8 ± 2.2 years [p = 0.21]).
Figure 1 presents the volume of procedures performed by participants as a primary operating physician. The volume of coronary angiogram and transthoracic echocardiogram varied greatly. Nearly half of trainees had experienced less than 50 cases of percutaneous coronary intervention, and majority of the participants (more than 97%) experienced less than 50 cases in the implantation of implantable cardioverter defibrillators or cardiac resynchronization therapy/cardiac resynchronization therapy-defibrillators.
We surveyed self-assessed clinical proficiency and satisfaction levels in the management of 6 CV subspecialty areas (ischemic heart disease, valvular heart disease, advanced heart failure, arrhythmia, peripheral artery diseases, and congenital heart diseases) and 3 noninvasive imaging studies (echocardiogram, nuclear studies, and computed tomography/magnetic resonance imaging) ( Figure 2 ). Mean overall clinical proficiency level rankings ranged between 2.9 and 6.4 on an 11-point scale. Trainees at the time of the survey were comfortable in managing coronary artery disease (average score 6.3 ± 2.4) but less so in peripheral arterial disease (score 3.8 ± 2.8), arrhythmias (score 3.7 ± 2.3), and congenital heart disease (score 2.9 ± 2.2). There was strong a correlation between self-assessed clinical proficiency and satisfaction levels in each subspecialty field (ischemic heart disease, r = 0.60, p <0.0001; valvular heart disease, r = 0.69, p <0.0001; advanced heart failure, r = 0.73, p <0.0001; arrhythmia, r = 0.63, p <0.0001; peripheral artery disease, r = 0.74, p <0.0001; congenital heart disease, r = 0.65, p <0.0001; echocardiogram, r = 0.68, p <0.0001, nuclear studies; r = 0.73, p <0.0001, and computed tomography/magnetic resonance imaging; r = 0.79, p <0.0001). Consistent with their clinical proficiency level, high levels of satisfaction for management of ischemic heart disease, valvular heart diseases, and noninvasive imaging studies was reported.
The 3 CV training program variables considered most important by the participants were the number of cases managed at the site, the number of procedures available at the site, and the quality and reputation of the attendings. The quality of basic research was rated relatively low ( Figure 3 ).
Satisfaction score was calculated from the sum of satisfaction levels in each of the previously described 6 CV subspecialty areas and for 3 noninvasive imaging studies. The participants with more than first tertiles for total satisfaction score (>50 points) were defined as the satisfied group. Clinical proficiency level; years of CV or general internal medicine physician’s experience; acquisition of specialist qualifications; the volume of coronary angiograms, percutaneous coronary interventions, transthoracic echocardiograms, and implantation of pacemaker/implantable cardioverter defibrillator; and publication of clinical scientific manuscripts were significant contributors to participant’s satisfaction levels ( Table 3 )
| Variable | OR | 95% CI | p Value |
|---|---|---|---|
| Cardiologist’s experience | 1.31 ∗ | 1.15–1.48 | <0.0001 |
| General internal medicine physician’s experience | 1.39 ∗ | 1.07–1.80 | 0.01 |
| Clinical proficiency scale | 3.71 † | 2.62–5.26 | <0.001 |
| Volume of procedures | |||
| Coronary angiogram | 1.32 ‡ | 1.15–1.52 | <0.001 |
| Percutaneous coronary intervention | 1.42 ‡ | 1.18–1.72 | <0.001 |
| Percutaneous peripheral intervention | 1.23 ‡ | 0.85–1.79 | 0.27 |
| Electrophysiologic study | 1.27 ‡ | 0.89–1.83 | 0.19 |
| Catheter ablation | 1.20 ‡ | 0.78–1.85 | 0.41 |
| Pacemaker implantation | 1.56 ‡ | 1.06–2.31 | 0.03 |
| ICD implantation | 1.49 ‡ | 0.47–4.77 | <0.0001 |
| CRT/CRT-D implantation | 1.41 ‡ | 0.22–9.02 | 0.72 |
| Transthoracic echocardiogram | 1.27 ‡ | 1.11–1.45 | <0.001 |
| Transesophageal echocardiogram | 1.17 ‡ | 0.95–1.44 | 0.14 |
| Scholarly activity, clinical | |||
| Presentation at meeting | 1.49 | 0.74–2.99 | 0.26 |
| Publication of scientific articles | 1.98 | 1.11–3.53 | 0.02 |
| Scholarly activity, basic | |||
| Presentation at meetings | 1.62 | 0.90–2.92 | 0.11 |
| Publication of scientific articles | 2.49 | 0.84–7.34 | 0.10 |
| Cardiology board qualification | 0.44 | 0.24–0.79 | 0.006 |
| PhD degree obtaining | 1.30 | 0.65–2.57 | 0.45 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


