Atrioventricular re-entrant tachycardia (AVRT) is caused by an accessory pathway: a strand of myocardium, congenital in origin, which straddles the groove between atria and ventricles.
In atrioventricular nodal re-entrant tachycardia (AVNRT), the AV node and its adjacent atrial tissues are functionally dissociated into two pathways: fast and slow. Typically, during AVNRT, AV conduction is via the slow pathway and ventriculoatrial conduction is via the fast pathway.
Both AVRT and AVNRT lead to a regular and usually narrow QRS tachycardia. The tachycardias can be terminated by vagal stimulation or by intravenous adenosine. The best approach to preventing recurrence is radiofrequency catheter ablation.
These supraventricular arrhythmias are caused by an additional electrical connection between atria and ventricles so that an impulse can repeatedly and rapidly travel around a circuit consisting of the normal atrioventricular (AV) junction and the additional AV connection (Figure 9.1). This is in contrast to the atrial arrhythmias discussed in the previous three chapters, where the mechanism responsible for the tachycardia is confined to the atria and the AV node merely transmits some or all of the atrial impulses to the ventricles.
Mechanism
In most cases the heart is structurally normal. If there is valve, myocardial or coronary disease these disorders will be coincidental to but not the cause of the arrhythmia. There are two main types of additional connection between atria and ventricles:
Accessory atrioventricular pathway
In atrioventricular re-entrant tachycardia (AVRT), the additional connection is an accessory AV pathway, which is a strand of myocardium, congenital in origin, which straddles the groove between atria and ventricles and therefore bypasses the AV node.
Figure 9.1 Initiation of AV junctional re-entrant tachycardia. An atrial extrasystole arrives at the AV junction while the bypass tract is still refractory to excitation following the last cardiac cycle (left-hand panel). The extrasystole is therefore only conducted to the ventricles via the AV node. By the time the extrasystole has traversed the AV node and reached the ventricles, the bypass tract has recovered and can conduct the impulse back to the atria, thereby initiating the re-entrant mechanism (right-hand panel).
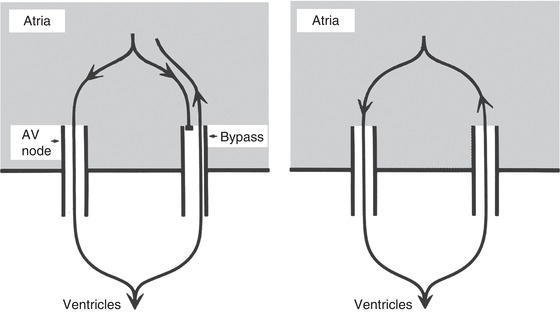
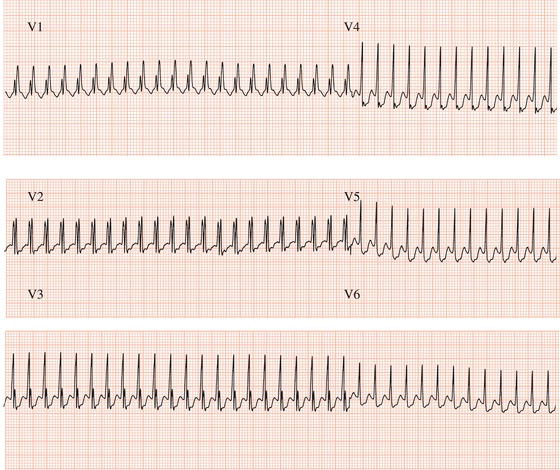
Figure 9.2 AV junctional re-entrant tachycardia. A regular tachycardia with narrow ventricular complexes.
Dual atrioventricular nodal pathways
In atrioventricular nodal re-entrant tachycardia (AVNRT), the AV node and its adjacent atrial tissues are functionally dissociated into two pathways: one that can conduct quickly, termed the fast pathway, and another which conducts relatively slowly, termed the slow pathway. The fast pathway has a relatively long recovery or refractory period whereas the slow pathway has a shorter refractory period. Typically during tachycardia, AV conduction is via the slow pathway and ventriculoatrial conduction is via the fast pathway.
ECG characteristics
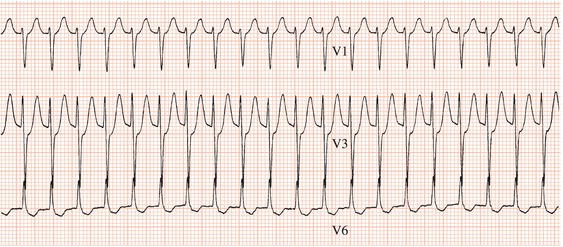
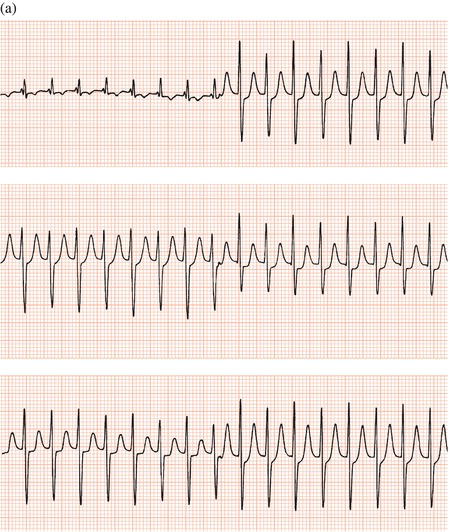
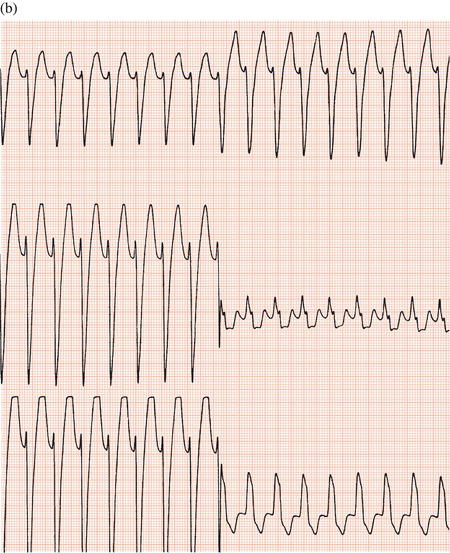
The tachycardia, whether AVRT or AVNRT, is regular. Usually the QRS complexes are normal and therefore narrow (Figure 9.2) but occasionally pre-existing bundle branch block or bundle branch block resulting from the fast heart rate will lead to broad ventricular complexes (Figures 9.3, 9.4).
Figure 9.3 AV junctional re-entrant tachycardia, leads V1–V6: (a) with narrow complexes; (b) the same patient a few minutes later, showing broad complexes that have developed due to functional left bundle branch block.
The rate during tachycardia can range from 130 to 250 beats/min, and it is influenced by the sympathetic nervous system. For example, sympathetic activity and consequently the speed of AV nodal conduction increase on standing or during exertion so the tachycardia may become faster.
Clearly, normal P waves will not occur during this arrhythmia. Since the circulating impulse re-enters the atria after ventricular activation, each QRS complex will be followed by a P wave, though this wave is not always evident (Figures 9.4–9.7). If the atrial rate exceeds the ventricular rate, whether spontaneously or due to a drug or manoeuvre which slows AV node conduction, then the rhythm is not AV re-entrant tachycardia; it is probably atrial tachycardia or flutter. (There is an exception to this important guideline: very rarely, 2:1 AV block can occur during AVNRT.)
ST segment and T wave changes can be caused by the tachycardia and persist for some time after its cessation: they are of no diagnostic significance. The ECG during sinus rhythm is usually normal unless the accessory pathway can also conduct from atria to ventricles, in which case the ECG will show the Wolff– Parkinson–White syndrome (Chapter 10).
Regular
Rate 130–250 beats/min
Usually narrow
Inverted, inscribed during or after each QRS complex
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree