Atrial Septal Defect
Defects in the atrial septum are relatively common. They appear at various sites in the septum and can be associated with other congenital abnormalities. In addition, there is a real or potential slit-like opening, the foramen ovale, where the fossa ovalis flap disappears behind the superior septal limbus. Generally, the higher pressure in the left atrium keeps the fossa ovalis flap in apposition to the superior septal limbus, and therefore the opening remains closed. In 20% of the population, however, the foramen ovale is patent and has the potential to allow shunting under certain circumstances. When pressure in the right atrium increases, as in right-sided heart failure, the septum becomes stretched and allows the foramen ovale to enlarge with significant shunting at the atrial level.
The sinus venosus atrial septal defect occurs high in the atrial septum and extends into the orifice of the superior vena cava, which becomes malpositioned slightly toward the left. There is usually anomalous drainage from the right superior pulmonary vein associated with these defects (Fig. 19.1).
The fossa ovalis type, also known as the ostium secundum defect, is the most common variety. This defect occurs in the midseptum in the vicinity of the fossa ovalis and may be small or very large. Infrequently, the defect may occur low in the septum and extend into the orifice of the inferior vena cava, which also becomes malpositioned toward the left. This type of defect is sometimes referred to as a sinus venosus defect of the inferior vena caval type and may be associated with anomalous pulmonary venous drainage. Rarely, the whole septum may be absent, giving rise to a single common atrium.
A defect low in the interatrial septum that extends down to the level of the atrioventricular valve orifices is part of the atrioventricular septal defect complex (see Chapter 22).
SURGICAL ANATOMY OF THE RIGHT ATRIUM
Although the right atrium is morphologically molded into a single chamber, it is formed by two components: the sinus venarum and the right atrial appendage (sometimes referred to as the body of the atrium). Systemic venous return flows in from opposing directions through the superior and inferior venae cavae into the sinus venarum. This smooth-walled area is the most posterior portion of the right atrium and stretches between the orifices of the caval veins. From the viewpoint of the surgeon looking down into the right atrium, the sinus venarum is more or less horizontal with the superior vena cava entering from the left and the inferior vena cava (bounded by the eustachian valve) entering from the right (Fig. 19.2).
Just below and medial to the orifice of the superior vena cava arises a muscle bundle, the crista terminalis, which springs into prominence as it circles the orifice of the superior vena cava to the right lateral wall of the atrium and continues inferiorly toward the inferior vena cava, thereby forming the boundary between the sinus venarum and the atrial appendage. This muscle bundle is evidenced on the outside of the atrium by a groove, the sulcus terminalis. Lying subepicardially in the sulcus terminalis, just below the entrance of the superior vena cava, is the sinoatrial node, which may be vulnerable to injury from the various surgical incisions and cannulations commonly performed on the right atrium. The remainder of the right atrium is made up of atrial appendage, which begins at the crista terminalis and extends forward (upward from the surgeon’s perspective) to surround the tricuspid valve and form an expanded chamber.
In contrast with the smooth-walled sinus venarum, the lateral wall of the atrial appendage is ridged with multiple narrow bands of muscle, the musculi pectinati. These bands arise from the crista terminalis and pass upward to the most anterior part of the atrium. Functionally, they supply the right atrium with enough pumping capacity to propel the venous inflow through the tricuspid valve into the right ventricle.
Just above the sinus venarum in the center of the medial wall is the fossa ovalis, a horseshoe- or elliptically shaped depression. The true interatrial septum consists of the fossa ovalis with variable contributions from the superior, anterior, and inferior limbic muscle bundles that surround it. The aortic root is hidden behind the anteromedial atrial wall between the fossa ovalis and the termination of the heavily trabeculated right atrial appendage. Segments of
the noncoronary and right sinuses of Valsalva are in close apposition to the atrial wall in this area. Their location may be manifested by the aortic mound, which is a bulge above and slightly to the left of the fossa ovalis. The aortic valve here can be more clearly visualized if its continuity, through the central fibrous body, with the adjacent tricuspid valve annulus is taken into consideration.
the noncoronary and right sinuses of Valsalva are in close apposition to the atrial wall in this area. Their location may be manifested by the aortic mound, which is a bulge above and slightly to the left of the fossa ovalis. The aortic valve here can be more clearly visualized if its continuity, through the central fibrous body, with the adjacent tricuspid valve annulus is taken into consideration.
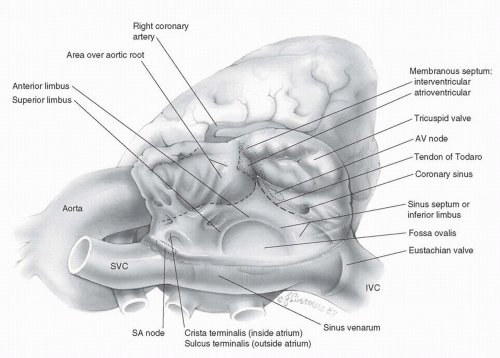 FIG. 19.2 Surgical anatomy of the right atrium. SVC, superior vena cava; SA, sinoatrial; IVC, inferior vena cava; AV, atrioventricular. |
Also, often invisible to the surgeon is the artery to the sinoatrial node, which can run through this same area. Although its origin and exact course are unpredictable, it takes a variable course toward the superior cavoatrial angle and the sinus node.
The tricuspid valve is located anteroinferiorly in the right atrium, where it opens widely into the right ventricle. The annulus of the tricuspid valve crosses over the membranous septum, dividing it into atrioventricular and interventricular segments. The membranous, or fibrous, septum is a continuation of the central fibrous body, through which the tricuspid, mitral, and aortic valves are connected. Immediately below the upper or atrioventricular section of the membranous septum lies the hidden atrioventricular node. It is situated at the apex of the triangle of Koch, the boundaries of which are the annulus of the septal leaflet of the tricuspid valve, the tendon of Todaro (running intramyocardially from the central fibrous body to the eustachian valve of the inferior vena cava), and its base, the coronary sinus. Anderson describes the tendon of Todaro as a fibrous extension of the commissure between the eustachian valve (of the inferior vena cava) and the thebesian valve (of the coronary sinus). Conduction tissue passes from the atrioventricular node as the bundle of His, below the membranous septum, and down into the muscular interventricular septum. The coronary sinus, draining the cardiac veins, is situated alongside the tendon of Todaro, between it and the tricuspid valve.
Incision
All forms of atrial septal defect can be approached through a median sternotomy. Many surgeons now use a lower ministernotomy approach or submammary right thoracotomy for simple secundum atrial septal defects. Others prefer the Brom modification of the median sternotomy incision to allow full exposure of the pericardial space with acceptable cosmetic results in female patients (see Chapter 1).
Cannulation
The ascending aorta is cannulated in the usual manner (see Chapter 2). The superior vena cava is usually cannulated directly, although it may be cannulated through the right atrial appendage. The inferior vena cava is cannulated through the atrial wall, just above the origin of the inferior vena cava. Tapes are then passed around both cavae. For those defects thought to be low in the atrial septum or for inferior sinus venosus defects, it is imperative to cannulate low on the inferior vena cava itself.
A tie is placed on the right atrial appendage. Inferior traction on the appendage allows adequate visualization of the right superior vena cava for direct cannulation in most instances. If direct cannulation is not feasible, a straight venous cannula can be passed into the superior vena cava through a purse-string suture on the right atrial appendage. 

Myocardial Preservation
Cold cardioplegic arrest of the myocardium is achieved by infusion of cold-blood cardioplegia into the aortic root (see Chapter 3).
Alternatively, closure of a simple septum secundum-type defect can be accomplished safely without clamping the aorta by inducing ventricular fibrillation (see subsequent text). This approach is used with minimally invasive incisions because aortic cross-clamping in these cases may be difficult.
SINUS VENOSUS ATRIAL SEPTAL DEFECT
Sinus venosus atrial septal defects usually occur high on the septum close to the orifice of the superior vena cava and are associated with anomalous drainage of right upper lobe pulmonary veins into the superior vena cava and right atrium (Fig. 19.3). Approximately 10% of patients with this type of atrial septal defect also have a persistent left superior vena cava, which may be suspected from a large coronary sinus on the preoperative echocardiogram.
Technique
The superior vena cava is cannulated directly high above the entry site of the highest anomalous pulmonary vein or preferably at the innominate/caval junction.
The aorta is cross-clamped, and cardioplegic solution is administered into the aortic root (see Chapter 3). The vena caval snares are then snugged down. A longitudinal atriotomy is made starting at a point 0.5 to 1 cm posterior
and parallel to the sulcus terminalis. The edges of the incision are then retracted to provide good exposure of the septal defect (Fig. 19.3). If additional exposure is required, the atriotomy is extended superiorly and posterolaterally across the superior vena caval-right atrial junction and onto the vena cava as far as necessary.
and parallel to the sulcus terminalis. The edges of the incision are then retracted to provide good exposure of the septal defect (Fig. 19.3). If additional exposure is required, the atriotomy is extended superiorly and posterolaterally across the superior vena caval-right atrial junction and onto the vena cava as far as necessary.
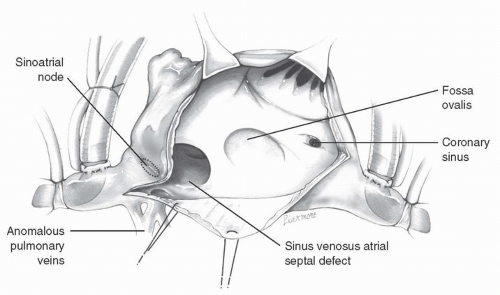 FIG. 19.3 Sinus venosus atrial septal defect and the superior extension of the atriotomy posterior to the sinoatrial node. |
The azygos vein, as it joins the superior vena cava, may at times obscure the surrounding structures. In this case, it may be ligated and divided to free up the superior vena cava and to provide better exposure of the anomalous pulmonary veins. 

A patch of glutaraldehyde-treated autologous pericardium or Gore-Tex is cut to an appropriate size and shape after examining the extent of the defect. With a continuous suture of 5-0 or 6-0 Prolene, the patch is sewn around the orifices of the anomalous veins and across to the anteromedial margin of the atrial septal defect (Fig. 19.4).
Sometimes it is necessary to place several sutures through the patch and the right atrial or superior vena caval wall around the openings of the anomalous veins before lowering the patch into position. Accurately placed sutures, well away from the anomalous vein orifices, will prevent subsequent stenosis. 

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree









