Atrial flutter has similar causes to atrial fibrillation. It is often idiopathic. Antiarrhythmic drugs are frequently ineffective and may sometimes cause an increase in ventricular rate. Cardioversion and catheter ablation are both first-line treatments. Embolic risk should be managed as for atrial fibrillation.
Common atrial flutter
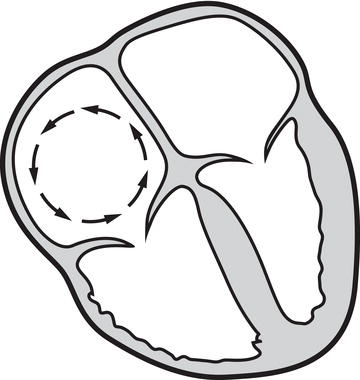
The arrhythmia is caused by repeated circulation of an impulse around the right atrium. Usually, the impulse circulates in a superior direction along the interatrial septum and returns in an inferior direction along the lateral border of the right atrium (Figure 7.1). The left atrium is activated by the impulses arising from the right atrium. Atrial flutter may be paroxysmal or sustained.
ECG characteristics
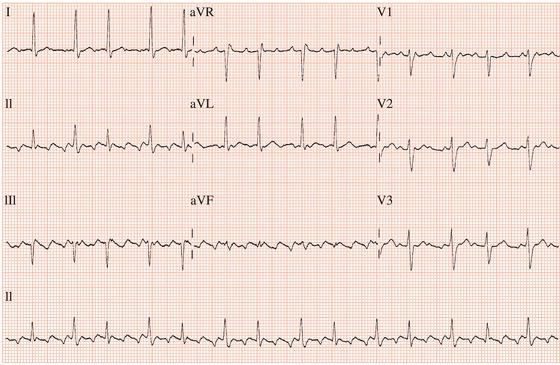
During the typical form of atrial flutter, the atria discharge regularly at a rate of approximately 300 beats/min. In many leads there will be no isoelectric line between atrial deflections, termed F waves, leading to the characteristic sawtooth appearance that is usually best seen in leads II, III and aVF. However, in some leads, especially lead V1, atrial activity will be seen in the form of discrete waves (Figure 7.2).
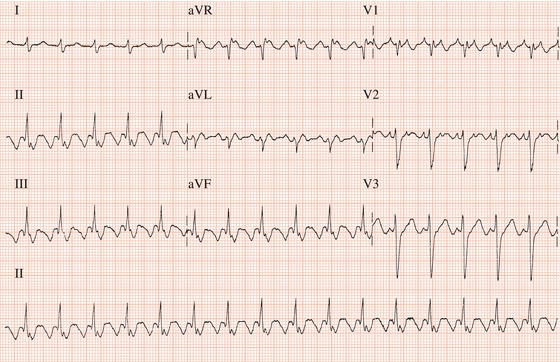
Commonly, in typical atrial flutter, the atrial impulse circulates counterclockwise within the right atrium, in which case the F waves are predominantly negative in leads II, III and aVF, of very low amplitude in lead I and positive in V1 (Figure 7.2). Uncommonly, the impulse circulates in a clockwise direction when the F waves will be positive in the inferior leads and negative in lead V1 (Figure 7.3).
Figure 7.2 Common atrial flutter: negative sawtooth pattern in the inferior leads and positive, discrete F waves in lead V1.
Atypical flutter
In atypical atrial flutter, the atrial rate is faster, ranging from 350 to 450 beats/min. It is not amenable to isthmus ablation (see below) and cannot be terminated by rapid atrial pacing.
Atrioventricular conduction
As with atrial fibrillation, the ventricular response to atrial flutter is determined by the conducting ability of the AV junction. Frequently, alternate F waves are conducted to the ventricles with a resultant ventricular rate close to 150 beats/min (Figure 7.4). AV nodal blocking drugs, impaired AV nodal function or high vagus nerve tone during the night may lead to a higher degree of AV block (Figure 7.5). High levels of sympathetic nervous system activity, as may occur during exercise, may enhance AV nodal conduction and result in 1:1 conduction and a ventricular rate of approximately 300 beats/min (Figure 7.6).
Figure 7.3 Uncommon form of typical atrial flutter due to clockwise rotation within the right atrial re-entrant circuit.
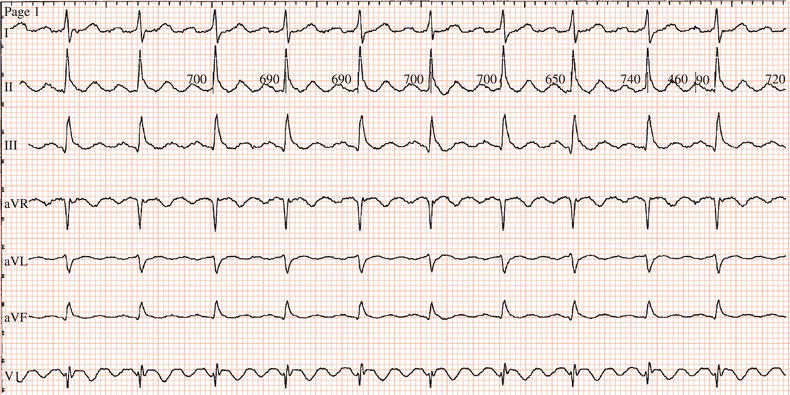
Figure 7.4 Atrial flutter with 2:1 AV block. The limb leads shows a classic sawtooth appearance while V1 shows discrete atrial waves. In V1, each QRS complex is immediately preceded by an F wave and is followed by an F wave which is superimposed on the T wave.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree