Atrial Fibrillation and Shortness of Breath
A 42-year-old woman had her first episode of atrial fibrillation 3 years ago. Over the last year, she developed symptoms of fatigue and shortness of breath.
Physical examination showed no signs of cardiac decompensation. On auscultation, a split second heart sound was noted.
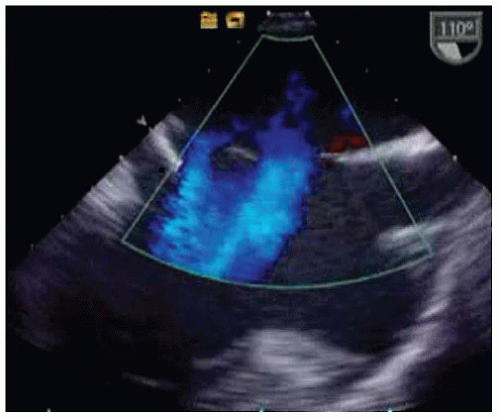
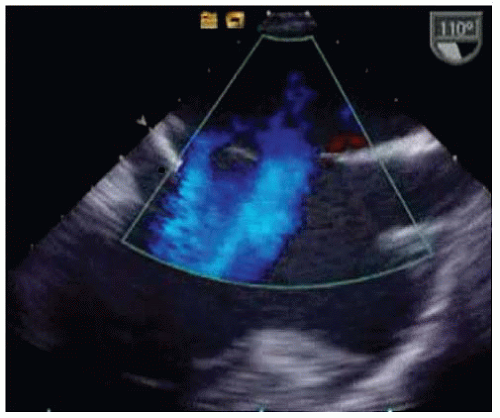
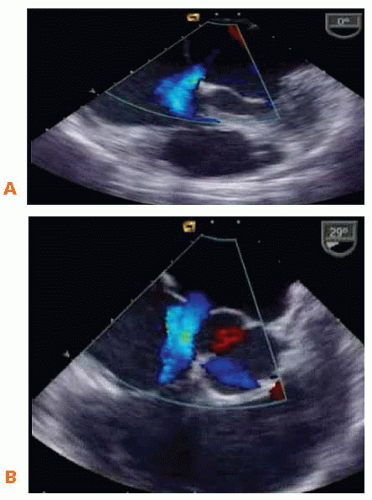 Figure 24-2. A. Conventional 2D transesophageal echocardiogram (TEE) with color Doppler in different planes at 0°. B. Conventional 2D TEE with color Doppler at 30°. |
QUESTION 1. What is the diagnosis?
A. Ventricular septal defect
B. Secundum atrial septal defect
C. Atrioventricular (AV) canal defect
D. Left-to-right shunting through a stretched patent foramen ovale
View Answer
ANSWER 1: B. The short-axis view (Fig. 24-2 and Video 24-1) at 30° shows that the patient had no aortic rim, and the long-axis view (Fig. 24-3 and Video 24-2) at 110° documents two atrial septal defects in the secundum portion of the atrial septum.
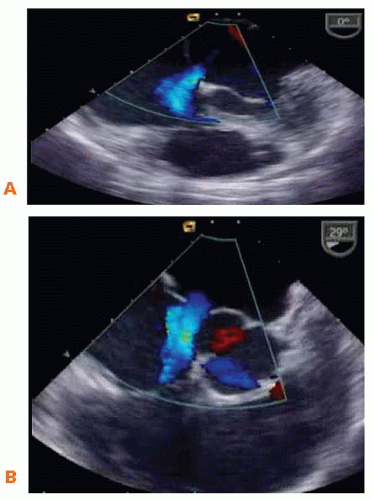 Figure 24-2. A. Conventional 2D transesophageal echocardiogram (TEE) with color Doppler in different planes at 0°. B. Conventional 2D TEE with color Doppler at 30°. |
QUESTION 2. How would you proceed?
A. The patient has only mild symptoms; a routine follow-up in 6 months is sufficient
B. Closure of the atrial septal defects (surgery or transcatheter closure)
View Answer




ANSWER 2: B. Indications for atrial septal defect closure include symptoms and/or right ventricular/right atrial enlargement and/or a pulmonic blood flow: Systemic blood flow > 1.5 and/or paradoxical embolism.1
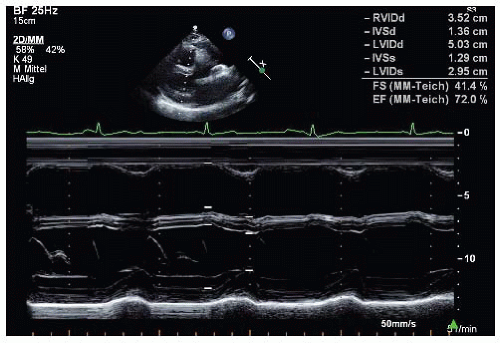
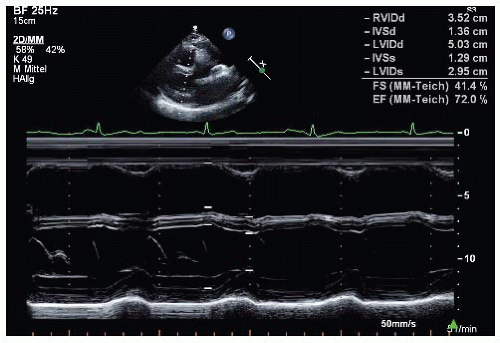
The patient has symptoms, and the M-mode (Fig. 24-1) shows right ventricular enlargement.
Therefore, treatment is indicated, and it was decided to close the defect with percutaneous closure devices.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree