Purpose of a high-risk clinic
Address diagnostic uncertainties
Recognize and manage factors that make asthma “difficult to treat”
Persistent triggers
Suboptimal adherence and inhaler technique
Uncontrolled comorbidities
Optimize self-management skills
Prevent and manage complications from long-term oral corticosteroid exposure
Assist with pheno-endotyping
Provide access to advanced therapies
Afford opportunities for training and research
15.4.1 Address Diagnostic Uncertainties
Some Common Asthma “Masqueraders”
Condition | Presentation |
|---|---|
Overlapping symptoms | |
Paradoxical vocal fold motion | Rapid onset/offset, inspiratory wheeze, cough, dysphonia, throat tightness, common triggers – exercise and irritants |
Dysfunctional breathing | Episodic shortness of breath, general sense of distress, sighing, dizziness, paresthesia |
Excessive Dynamic Airway Collapse (EDAC)/tracheobronchomalacia | Severe harsh paroxysmal cough, sputum retention, expiratory wheeze |
Central airway obstruction (foreign body, subglottic stenosis, tumor) | Acute or subacute, constant, progressive dyspnea, hemoptysis, focal wheeze |
Airflow obstruction | |
Bronchiectasis | Productive cough, recurrent infections |
Alpha 1 anti-trypsin deficiency | Dyspnea, family history of emphysema, liver disease |
Chronic Obstructive Pulmonary Disease (COPD) | Past/current smoking or noxious exposure, cough, sputum, dyspnea |
Sarcoidosis | Cough, wheeze, dyspnea, extrapulmonary and constitutional symptoms |
Bronchiolitis | Progressive dyspnea, idiopathic or associated with autoimmune disease, toxic inhalation, posttransplant, infections, and medications |
15.4.2 Recognize and Manage Factors that Make Asthma “Difficult to Treat”
Incorrect diagnosis, suboptimal adherence, persistent exposure to unrecognized or unavoidable triggers, and uncontrolled comorbidities can all contribute to poor control of asthma. Before pursuing phenotype-based targeted therapies, it is imperative to evaluate and address these factors. A systematic approach to assessment and management of these factors results in achieving asthma control in a majority of patients with “difficult asthma” and identifies the small subgroup of patients with truly severe asthma who are most likely to benefit from these advanced and expensive therapies [20–22].
15.4.2.1 Triggers
Identification of asthma triggers and incorporation of an individualized trigger-avoidance plan are important components of a successful asthma management strategy. Environmental triggers may be allergic, irritant or infectious, indoor or outdoor, and may occur at home, school or workplace. Workplace triggers are particularly important to consider in patients with late-onset asthma [23]. Emotional stress can be an important trigger and a comorbidity [24]. In patients with severe or difficult asthma, increasing numbers of asthma triggers are associated with an increase in severity and frequency of asthma exacerbations and a decrease in asthma-related quality of life [24]. Multiple triggers can co-exist, and an integrated approach is often necessary [25–29].
15.4.2.2 Comorbidities
Sinonasal disease, gastroesophageal reflux disease (GERD), obstructive sleep apnea, psychopathologies, and vocal cord dysfunction, all have high prevalence in patients with difficult-to-treat asthma [30–33]. In a recent study, Radhakrishna and colleagues demonstrated that use of validated questionnaires in patients with difficult asthma improved detection of relevant comorbidities [12]. Comorbidities in asthma are associated with high symptom burden, worse quality of life, and increased exacerbation risk [21, 34–36]. A systematic assessment and control of these comorbidities can improve asthma-related outcomes (Chap. 4) [11].
15.4.2.3 Adherence
Poor adherence is common in difficult asthma and associated with worse outcomes (Chap. 3) [37–40]. Among patients attending a high-risk asthma clinic, only 25% were adherent with all prescribed medications [38]. Common barriers to adherence include high cost, suboptimal patient-provider communication, poor disease insight, forgetfulness, cultural beliefs, side effects, and lack of perceived benefit [41–43]. Behavioral changes are more likely to be seen if the medical advice is linked to patient’s goals and preferences. Self-report consistently overestimates adherence; objective confirmation with review of pharmacy data or use of a monitoring device is preferred [44]. Multifaceted interventions through a specialized severe asthma service can result in improved adherence to prescribed treatments and positively impact clinical outcomes [45].
15.4.2.4 Inhaler Technique
Patients with asthma now have more choices in inhaler devices than even before. Unfortunately, inhaler handling errors commonly interfere with effective drug delivery and result in poor asthma control [46]. A recent systematic review found that inhaler-use errors continue to occur frequently and have not changed significantly over 40 years [47]. Achieving adequate inhaler technique requires repeated review but majority of the patients are still unable to use their inhalers correctly [48]. Ability to actuate the inhaler device, coordination with inhalation timing, and generation of required peak inspiratory flow are all factors that need to be considered when selecting an inhaler device. This can be achieved in a specialized clinic through a multidisciplinary approach that includes an asthma educator, respiratory therapist or pharmacist.
15.4.3 Optimize Self-Management Skills
Supported self-management in asthma and patients’ active participation in their care are associated with improved asthma-related outcomes as well as patient satisfaction [49–51]. Asthma management plans should be tailored taking into account patient’s preferences. Available shared decision-making tools can be used to engage, educate, and empower patients to select treatment options better aligned with their goals and beliefs [52]. Incorporation of a patient-specific written asthma action plan is associated with reduced emergency room visits, hospitalizations, loss of productivity, and improved quality of life; however, asthma action plans are woefully underutilized in primary care and specialty practices [53, 54]. A growing body of evidence suggests that mobile technology may be more effectively used to engage patients and improve asthma outcomes [55, 56].
15.4.4 Prevent and Manage Complications from Long-Term Oral Corticosteroid Exposure
Many patients with uncontrolled asthma require treatment with maintenance oral corticosteroids (OCS). Long-term use of OCS is associated with a myriad of adverse effects including hyperglycemia, premature cataracts, glaucoma, osteoporosis, increased risk of fractures, Hypothalamus-Pituitary-Adrenal (HPA) axis suppression, and weight gain. Recent studies evaluating steroid-sparing effect of biologics have consistently demonstrated that a lower OCS dose can be achieved during optimization phase, even prior to any other therapeutic intervention, suggesting that patients often receive higher than necessary dose of OCS [57–59]. Specialist referral can help in optimizing OCS dose, introduction of steroid-sparing therapies, as well as close monitoring and management of adverse effects.
15.4.5 Assist with Phenotyping
Asthma that requires therapy at GINA steps 4/5 to maintain control, or remains uncontrolled despite high-intensity therapy, benefits from additional testing to better understand the inflammatory phenotype [1, 60]. Our understanding of the disease heterogeneity in asthma has improved with findings from several large well-characterized cohorts using unbiased cluster analysis (Chap. 7) [61–63]. This characterization can identify certain “treatable traits” that further inform selection of more advanced therapies as well as removal of medications that are ineffective. Partnering with an asthma specialist allows comprehensive evaluation and access to more sophisticated lung function testing and biomarker assays to better characterize difficult asthma.
15.4.6 Access to Advanced Therapies
There have been remarkable recent advances in asthma therapeutics (Chap. 8). Several novel therapies have been approved for use in moderate-to-severe asthma, including biologics and bronchial thermoplasty. In fact, after a 12-year hiatus, we have seen a new monoclonal antibody for asthma receive FDA approval every year since 2015. There have also been improvements in inhaler devices and inhaled drug formulations (Chap. 6). However, many barriers often prevent patients from receiving these effective interventions. General practitioners may not be familiar or comfortable with initiating advanced therapies. There are fiscal challenges associated with high cost of the medications and difficulty accessing available financial assistance programs. Administration of a biologic typically occurs in a severe asthma clinic or infusion center, and requires close monitoring for potentially serious adverse effects. Similarly, bronchial thermoplasty procedure is performed in a specialized center with appropriate expertise, only after evaluation by an asthma specialist. A high-risk asthma service can assist patients and referring providers in navigating this maze of therapeutic options.
15.4.7 Afford Opportunities for Education and Research
A comprehensive severe asthma program can provide opportunities for education and training to many learners including patients, providers, physicians-in-training, and other healthcare staff [64]. Patients can access novel therapies through clinical trials. Registries and tissue banking from patients with well-characterized difficult asthma can improve our understanding of pathobiology of the disease. Post-approval use of advanced therapies can lead to pragmatic real-world effectiveness studies [65].
15.5 The Logistics of a Specialized Severe Asthma Clinic
15.5.1 Concept and Business Plan
Severe asthma poses a disproportionately high burden on healthcare resources. A case for setting up a high-risk asthma clinic can be made by highlighting the potential cost savings from reduced emergency room visits/hospitalizations, judicious use of medications, improved control of relevant comorbidities, and gained productivity. A “needs assessment” should be performed first taking into consideration the size of population being served, prevalence of difficult asthma in that population, willingness of providers to refer patients, ease of access for the patients, and if a severe asthma program is already available to the community.
15.5.2 Facility
The physical space should have consultation/exam rooms, work area for clinicians, private phone triage area, an area to store and administer biologics, as well as a conference room for education and multidisciplinary case review. The area should house basic life support equipment as well as medications needed for immediate rescue, such as epinephrine, in case of systemic reactions to administered biologics. It should have a fully equipped and staffed pulmonary function laboratory with capability of performing spirometry, lung volume measurements, diffusing capacity, bronchodilator reversibility, bronchoprovocation testing, and fractional exhaled nitric oxide measurement. Placebo inhaler devices are needed for training patients. Additional testing facilities should be located nearby including imaging and sleep testing.
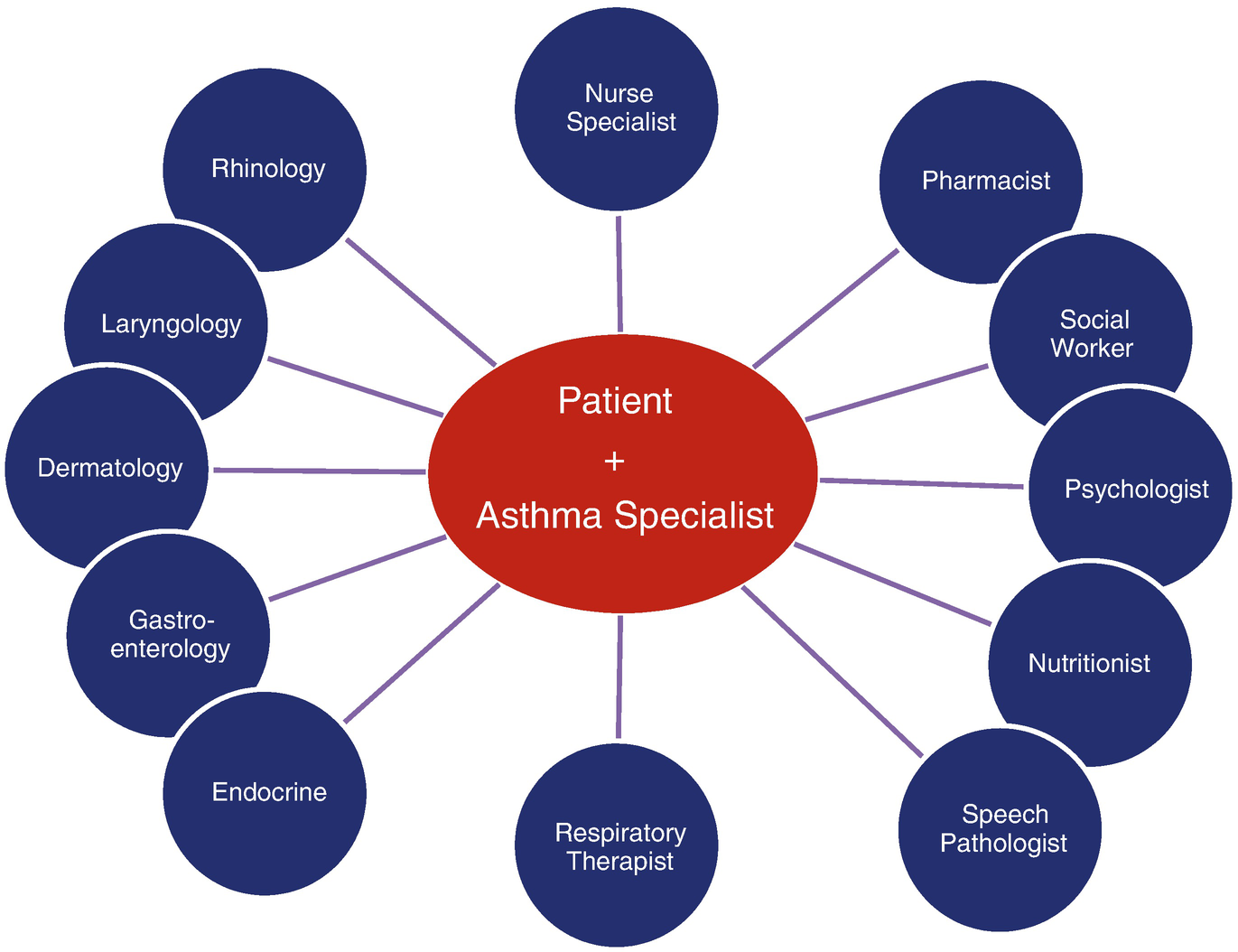
15.5.3 Core-Team Structure

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


