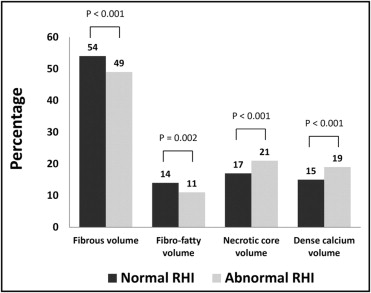
Although reactive hyperemia index (RHI) predicts future coronary events, associations with intravascular ultrasound (IVUS)-assessed coronary plaque structure have not been reported. This study therefore investigated associations between RHI and IVUS-assessed coronary plaques. In 362 patients RHI was measured by noninvasive peripheral arterial tonometry and coronary plaque components (fibrous, fibrofatty, necrotic core, and dense calcium) were identified by IVUS in 594 vessel segments of the left anterior descending, circumflex, and/or right coronary arteries. RHI values <1.67 were considered abnormal. Analysis of variance was used to detect independent associations between RHI and plaque composition. Patients with an abnormal RHI had greater plaque burden (41% vs 39% in patients with normal RHI, p = 0.047). Compared to patients with normal RHI, plaque of patients with abnormal RHI had more necrotic core (21% vs 17%, p <0.001) and dense calcium (19% vs 15%, p <0.001) and less fibrous (49% vs 54%, p <0.001) and fibrofatty (11% vs 14%, p = 0.002) tissue. After adjustment for age, gender, cardiovascular risk factors, and drug therapy, abnormal RHI remained significantly associated with fibrous (F ratio 14.79, p <0.001), fibrofatty (F ratio 5.66, p = 0.018), necrotic core (F ratio 14.47, p <0.001), and dense calcium (F ratio 10.80, p = 0.001) volumes. In conclusion, coronary artery plaques of patients with abnormal RHI had a larger proportion of necrotic core and dense calcium. The association of an abnormal RHI with a plaque structure that is more prone to rupture may explain why these patients exhibit a greater risk of coronary events.
Endothelial dysfunction (ED) promotes coronary artery disease (CAD) and has been shown to precede angiographic evidence of atherosclerosis. Reactive hyperemia index (RHI) measured by noninvasive peripheral arterial tonometry (PAT) may be used to noninvasively measure ED. Previous studies have shown that RHI correlates with presence of cardiovascular risk factors, biomarkers of atherosclerosis, presence of CAD, and occurrence of cardiovascular events. However, to the best of the authors’ knowledge, no previous study has assessed the associations of RHI with intravascular ultrasound (IVUS)-assessed plaque structure. Because plaque structure is a major determinant of future coronary events, the question arises whether RHI correlates with atherosclerotic plaque structure in coronary arteries. The present study therefore investigated associations between RHI and IVUS-assessed coronary plaque structure.
Methods
Consecutive patients referred to a single center (Luzerner Kantonsspital, Lucerne, Switzerland) for elective or rescue coronary angiography from May 2007 through January 2011 were evaluated for this prospective study. The decision to perform coronary angiography was taken based on clinical grounds and at the discretion of the cardiologist in charge. IVUS was performed during angiography, if the anatomy was suitable for the IVUS procedure. A priori anatomic criteria precluding safe IVUS examination included total or subtotal stenosis of the left main, proximal left anterior descending, or circumflex coronary artery with potential for hemodynamic instability during the procedure. Hemodynamically unstable patients were also excluded. In patients who presented with acute coronary syndrome, IVUS was not performed if the main vessel contained the culprit lesion. Three hundred sixty-two patients qualified for inclusion in the study and were willing to participate. All patients provided written informed consent. The institutional ethical committee approved the study, which was conducted in compliance with the Declaration of Helsinki.
IVUS was acquired using an Eagle Eye gold Catheter (20 MHz) and an automatic continuous speed pullback device (Volcano Corp., Rancho Cordova, California). Pullback velocity was 1 mm/s. Frames were acquired electrocardiographic triggering. In all 362 patients, IVUS was performed in the proximal 4 cm of the left anterior descending, left circumflex, and/or right coronary artery. IVUS data were analyzed by a specially trained investigator who was blinded to clinical and angiographic data. Contours of the lumen and media–adventitia interface were detected semiautomatically. For every cross-sectional area, vessel diameters and areas for different plaque components were calculated using pcVH2.2 software (Volcano Corp.). Spectral analysis of IVUS radiofrequency signals provided a histology of the plaque, identifying 4 major plaque components (fibrous, fibrofatty, necrotic core, and dense calcium). The software calculated the absolute volumes of each of the 4 plaque components and their relative amounts expressed as percentages of the total volume of the 4 components within the 4-cm segment. Total plaque volume was calculated as the sum of volumes of all 4 plaque components and of the media–adventitia. Plaque burden was defined as the ratio between plaque volume and the sum of plaque and lumen volumes.
RHI was measured 1 day after coronary angiography using PAT (Itamar Medical, Ltd., Caesarea, Israel). Drugs were continued. The principle of PAT has been previously described. The peripheral arterial tonometric finger probe was placed on each index finger, and after a baseline period of 5 minutes, total occlusion was performed with a blood pressure cuff on the right arm for 5 minutes. The cuff was inflated to suprasystolic pressures to obtain complete occlusion. Thereafter, the cuff was deflated and the hyperemic response of the occluded right arm was recorded and compared to the nonoccluded left arm (control arm) to obtain the RHI. RHI values <1.67 have been shown to indicate ED and were therefore considered abnormal.
In all 362 patients, clinical characteristics (age, gender, cardiovascular risk factors, medical history, and clinical presentation) were assessed at baseline. Hypertension was defined as increased blood pressure >140/90 mm Hg according to current guidelines. Dyslipidemia was defined as total cholesterol >234 mg/dl (6.0 mmol/L) or low-density lipoprotein cholesterol >117 mg/dl (3.0 mmol/L). Diagnosis of diabetes mellitus was made if fasting plasma glucose was ≥7 mmol/L on ≥2 different days or if postprandial plasma glucose was ≥11.1 mmol/L. Patients were considered smokers if they currently smoked ≥1 cigarette per week. Patients who previously stopped smoking were considered nonsmokers. A positive family history of CAD was defined as evidence of CAD in a parent or sibling <60 years old.
Data were analyzed using STATA 11.2 (STATA Corp. LP, College Station, Texas). Student’s t test was used for continuous variables with normal distribution and Mann–Whitney test for variables with non-normal distribution. For categorical variables chi-square and Fisher’s exact tests were used. Analysis of variance was used to verify the independent association of RHI with plaque composition. Analysis of variance was performed as a multivariable model including the following independent factor variables: age and gender, variables that showed differences in baseline characteristics (smoking status, presence of diabetes, systolic and diastolic blood pressures, presence of CAD and previous stroke), and variables that were deemed clinically relevant (use of angiotensin-converting enzyme inhibitor and/or statin). Continuous variables age and blood pressure were dichotomized at their median values for analysis of variance. For reporting of analysis of variance, the F ratio and p value are provided. For all statistical comparisons, a p value <0.05 was considered statistically significant.
Results
Baseline characteristic are listed in Table 1 . Mean age was 59.6 ± 10.7 years (range 20.5 to 83.7). One-, 2-, or 3-vessel CAD was found during coronary angiography in 73.8% of patients. Mean RHI was 1.82 ± 0.48 (range 1.00 to 3.97). Dichotomization of the RHI at 1.67 resulted in a group of 199 study participants with normal RHI and 163 study participants with abnormal RHI. Patients with abnormal RHI had higher systolic and diastolic blood pressures than patients with normal RHI ( Table 1 ). Patients with abnormal RHI were more often current smokers, were more likely to have diabetes, and more frequently had CAD at angiography or a previous stroke. For other baseline characteristics, no significant differences in patients with normal versus abnormal RHI were found.
| Characteristic | All (n = 362) | RHI | p Value ⁎ | |
|---|---|---|---|---|
| Normal (n = 199) | Abnormal (n = 163) | |||
| Age (years), mean ± SD | 59.6 ± 10.7 | 59.2 ± 10.2 | 60.1 ± 11.2 | 0.415 |
| Women | 99 (27.4%) | 61 (30.7%) | 38 (23.3%) | 0.119 |
| Body mass index (kg/m 2 ), mean ± SD | 27.4 ± 4.4 | 27.4 ± 4.7 | 27.4 ± 4.1 | 0.890 |
| Obesity † | 84 (23.2%) | 45 (22.6%) | 39 (23.9%) | 0.768 |
| Systolic blood pressure (mm Hg), mean ± SD | 131 ± 20 | 130 ± 19 | 134 ± 20 | 0.039 |
| Diastolic blood pressure (mm Hg), mean ± SD | 76 ± 12 | 74 ± 12 | 78 ± 11 | 0.005 |
| Hypertension † | 222 (61.3%) | 122 (61.3%) | 100 (61.3%) | 0.993 |
| Dyslipidemia † | 249 (68.8%) | 138 (69.3%) | 111 (68.1%) | 0.799 |
| Current smoker | 86 (23.8%) | 39 (19.6%) | 47 (28.8%) | 0.040 |
| Diabetes mellitus | 58 (16.0%) | 25 (12.6%) | 33 (20.2%) | 0.047 |
| Positive family history | 138 (38.1%) | 71 (35.7%) | 67 (41.1%) | 0.290 |
| Previously known coronary artery disease | 62 (17.1%) | 29 (14.6%) | 33 (20.2%) | 0.154 |
| Previous stroke | 13 (3.6%) | 3 (1.5%) | 10 (6.1%) | 0.023 |
| Previous peripheral artery disease | 17 (4.7%) | 8 (4.0%) | 9 (5.5%) | 0.502 |
| Clinical presentation at date of angiography | ||||
| Angina pectoris | 0.642 | |||
| Canadian Cardiovascular Society 0 | 79 (21.8%) | 40 (20.1%) | 39 (23.9%) | |
| Canadian Cardiovascular Society 1 or 2 | 190 (52.5%) | 111 (55.8%) | 79 (48.5%) | |
| Canadian Cardiovascular Society 3 or 4 | 93 (25.7%) | 48 (24.1%) | 45 (27.6%) | |
| Acute coronary syndrome ‡ | 45 (12.4%) | 25 (12.6%) | 20 (12.3%) | 0.933 |
| Medication § | ||||
| Angiotensin-converting enzyme inhibitor | 118 (32.6%) | 65 (32.7%) | 53 (32.5%) | 0.976 |
| β Blocker | 164 (45.3%) | 94 (47.2%) | 70 (42.9%) | 0.414 |
| Statin | 146 (40.3%) | 76 (38.2%) | 70 (42.9%) | 0.359 |
| Findings during coronary angiography | ||||
| Number of coronary arteries narrowed ¶ | 0.035 | |||
| 1 | 92 (25.4%) | 49 (24.6%) | 43 (26.4%) | |
| 2 | 90 (24.9%) | 47 (23.6%) | 43 (26.4%) | |
| 3 | 85 (23.5%) | 42 (21.1%) | 43 (26.4%) | |
| Left ventricular ejection fraction (%), mean ± SD | 69 ± 12 | 70 ± 11 | 69 ± 13 | 0.352 |
| Low-density lipoprotein cholesterol (mg/dl), mean ± SD | 104.4 ± 38.7 | 104.4 ± 42.5 | 104.4 ± 38.7 | 0.381 |
⁎ Comparisons of participants with normal versus abnormal reactive hyperemia index.
† Obesity was defined as body mass index ≥30 kg/m 2 . Hypertension was defined as a repeatedly increased blood pressure >140/90 mm Hg. Dyslipidemia was defined as total cholesterol >234 mg/dl (6.0 mmol/L) or low-density lipoprotein cholesterol >117 mg/dl (3.0 mmol/L).
‡ Defined as acute presentation with increased troponin.
§ Long-term medication within 2 weeks before intravascular ultrasound.
¶ Number of coronary arteries with ≥1 coronary luminal stenosis of ≥50%.
In the 362 study participants, 594 proximal vessel segments were assessed by IVUS. Plaque structure was assessed in the left anterior descending coronary artery in 269 participants, left circumflex coronary artery in 193 participants, and right coronary artery in 132 participants. Plaque composition in the left anterior descending, left circumflex, right coronary arteries and all vessel segments pooled significantly differed in patients with normal versus abnormal RHI ( Table 2 ). Patients with abnormal RHI had significantly larger relative amounts of necrotic core and dense calcium volumes and significantly smaller relative amounts of fibrous and fibrofatty tissue ( Figures 1 and 2 ) . Compared to patients with normal RHI, patients with abnormal RHI had 21% more necrotic core volume and 25% more dense calcium volume in the pooled vessel segments. There were also tendencies toward larger plaque volumes and greater plaque burden in the left anterior descending, left circumflex, and right coronary arteries of patients with abnormal RHI, but these differences achieved statistical significance only when all vessel segments were pooled.
| Plaque Component | LAD | LCx | RCA | All Vessel Segments Pooled | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Normal RHI (n = 147) | Abnormal RHI (n = 122) | p Value | Normal RHI (n = 103) | Abnormal RHI (n = 90) | p Value | Normal RHI (n = 75) | Abnormal RHI (n = 57) | p Value | Normal RHI (n = 325) | Abnormal RHI (n = 269) | p Value | |
| Plaque volume (ml) | 224 ± 101 | 253 ± 108 | 0.023 | 193 ± 90 | 195 ± 80 | 0.827 | 249 ± 124 | 286 ± 118 | 0.092 | 220 ± 105 | 241 ± 107 | 0.018 |
| Lumen volume (ml) | 333 ± 159 | 335 ± 144 | 0.942 | 331 ± 129 | 320 ± 120 | 0.526 | 393 ± 165 | 406 ± 140 | 0.635 | 346 ± 153 | 345 ± 139 | 0.892 |
| Plaque burden (%) | 41 ± 13 | 43 ± 12 | 0.093 | 37 ± 11 | 38 ± 10 | 0.414 | 39 ± 14 | 41 ± 11 | 0.366 | 39 ± 13 | 41 ± 11 | 0.047 |
| Fibrous volume (%) | 54 ± 12 | 50 ± 12 | 0.011 | 52 ± 13 | 48 ± 14 | 0.040 | 55 ± 13 | 49 ± 13 | 0.018 | 54 ± 13 | 49 ± 13 | <0.001 |
| Fibrofatty volume (%) | 15 ± 12 | 12 ± 10 | 0.076 | 12 ± 12 | 9 ± 9 | 0.053 | 15 ± 14 | 12 ± 11 | 0.121 | 14 ± 12 | 11 ± 10 | 0.002 |
| Necrotic core volume (%) | 16 ± 8 | 20 ± 9 | <0.001 | 19 ± 8 | 22 ± 8 | 0.023 | 17 ± 9 | 22 ± 9 | 0.001 | 17 ± 9 | 21 ± 9 | <0.001 |
| Dense calcium volume (%) | 14 ± 12 | 17 ± 13 | 0.019 | 17 ± 14 | 21 ± 15 | 0.014 | 13 ± 13 | 17 ± 13 | 0.017 | 15 ± 13 | 19 ± 14 | <0.001 |

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


