Chapter 3 Assessment tools
3.1 Arterial Blood Gases (ABGs)
3.7 Breathing Pattern (See under 3.54 Respiratory Pattern – Page 148)
3.8 Breathlessness (Dyspnoea) Scales
3.10 (Invasive) Cardiac Monitoring
3.11 Central Venous Pressure (CVP)
3.12 Cerebral Perfusion Pressure (CPP)
3.14 Chest Imaging (Including Chest X-rays)
3.15 Chest X-ray (See under 3.14 Chest Imaging – Page 68)
3.23 Early Warning Scores (EWS)
3.24 Electrocardiogram (ECG) (See under 3.35 Heart Rhythms – Page 109)
3.25 Electrolytes (See under 3.6 Blood Results – page 49)
3.26 End-Tidal Carbon Dioxide (ETCO2) 92
3.27 Exercise (aerobic fitness) Testing
3.29 FEV1/FVC (See under 3.40 Lung Volumes and Lung Function Tests – Page 120)
3.30 Flow Volume Loops (See under 3.40 Lung Volumes and Lung Function Tests – Page 120)
3.31 Fluid Balance (Including Urine Output)
3.32 General Observation (See Chapter 1)
3.36 Inspiratory Muscle Testing (See under 3.40 Lung Volumes and Lung Function Tests – Page 120)
3.37 Intracranial Pressure (ICP)
3.38 ITU (critical care) Charts
3.40 Lung Volumes and Lung Function Tests (Pulmonary Function Tests)
3.41 Muscle Charting (Oxford Grading)
3.46 Peak Flow (See under 3.40 Lung Volumes and Lung Function Tests – Page 120)
3.50 Quality of Life Questionnaires
3.51 Rating of Perceived Exertion (RPE)
3.53 Renal Function (See under 3.6 Blood Results and 3.31 Fluid Balance – Pages 49 and 102)
3.61 TPR (Temperature, Pulse and Respiration) Chart
3.62 Ventilation–Perfusion (V/Q) Matching
This chapter contains assessment procedures that may be used with respiratory patients. For each assessment performed, you need to select those that are most appropriate for each patient. If you are unsure which are appropriate, refer back to the assessment checklists in Chapter 2, which relate the tools to the assessment process.
Each technique has distinct sections:
• Definition: explains what the tool or measurement is about in simple terms.
• Purpose: suggests why the test/measurement is done and why this is important for physiotherapists.
• Procedure: gives step-by-step instructions on how the technique should be undertaken.
• Findings: looks at the findings and how this information may be of use to you, linking theoretical concepts to practical application.
• Documentation: demonstrates how this information should be recorded in your notes.
3.1 Arterial blood gases (ABGs)
Procedure
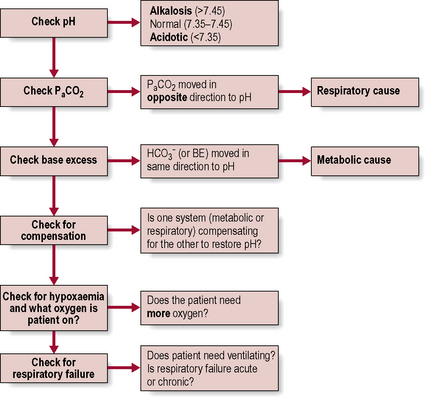
Physiotherapists need to be able to analyse the results (Fig. 3.1.1). The procedure itself involves taking an arterial blood sample and is normally carried out only by medical or nursing staff and some extended scope physiotherapists with specialized training.
Findings (Fig. 3.1.2, Table 3.1.1)
You should also consider haemoglobin (Hb) levels when interpreting ABG results (see 3.48 Pulse oximetry). Fig 3.1.2 summarizes the process of interpreting ABG’s in flowchart format.
Table 3.1.1 Blood gas measurements
| pH | |
| PaCO2 | |
| PaO2 | |
| SaO2 | |
 | |
| BE (base excess) |
NB. Partial pressure refers to the pressure exerted by one specific gas (e.g. oxygen), which forms part of the total pressure exerted by the mixture of gases (e.g. oxygen, carbon dioxide and nitrogen) in the blood.
 levels and make the blood more alkaline, thereby restoring the pH.
levels and make the blood more alkaline, thereby restoring the pH. are outside the normal range and the pH is within the normal range.
are outside the normal range and the pH is within the normal range. are both out of range but the pH is not quite within normal limits.
are both out of range but the pH is not quite within normal limits.6. Check for respiratory failure
Type One failure is when One gas (i.e. Oxygen) is affected – remember they both begin with O!
Type Two is when Two gases (i.e. oxygen and carbon dioxide) are affected.
 levels because it takes time (e.g. days) for adequate compensation to occur. Therefore, the pH is likely to be low (respiratory acidosis).
levels because it takes time (e.g. days) for adequate compensation to occur. Therefore, the pH is likely to be low (respiratory acidosis). levels. Therefore, the pH may be normal, or only slightly lower than normal (compensated respiratory acidosis). Check any current ABG results against any previous or usual results as this will also help to confirm the diagnosis of acute or chronic failure.
levels. Therefore, the pH may be normal, or only slightly lower than normal (compensated respiratory acidosis). Check any current ABG results against any previous or usual results as this will also help to confirm the diagnosis of acute or chronic failure.3.2 Attachments
Definition
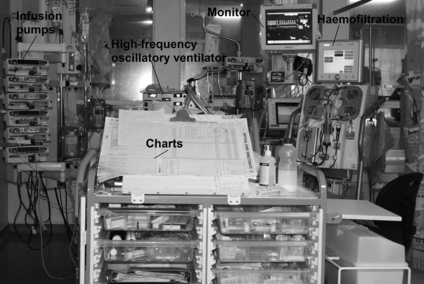
These may be any piece of equipment that is attached to the patient, e.g. intravenous (i.v.) lines, central venous line, ECG lines, surgical drains, ventilator tubing, saturations monitor and catheter (Figs 3.2.1 and 3.2.2).
Procedure
Be aware of all attachments and take care not to displace any equipment during your assessment.
3.3 Auscultation
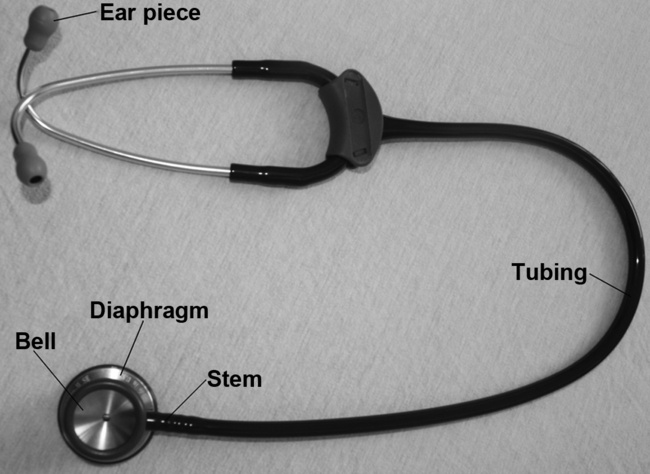
Procedure
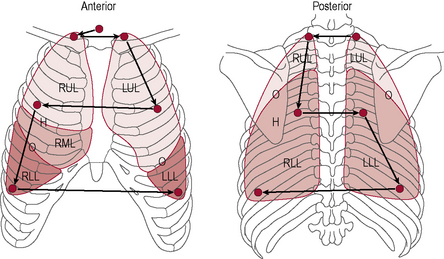
Fig 3.3.2 Auscultation points.
Reproduced and modified with kind permission from Pryor JA, Prasad SA. 2008 Physiotherapy for Respiratory and Cardiac Problems, 4th Edn. Edinburgh, UK: Churchill Livingstone.
Table 3.3.1 Auscultation zones
| Anterior | ||
| Mid-axillary | Left and right | |
| Posterior |
Findings
Breath sounds (Table 3.3.2) arise in the trachea and bronchi and are caused by the turbulence of the air as it flows in and out of these large airways. If you listen over the trachea (just below the cricoid cartilage or Adam’s apple) you will hear what they sound like at the source.You will notice that they are very loud here and also quite harsh sounding. Inspiration and expiration are heard clearly (both are loud) and there is a very slight pause between them. These sounds are known as bronchial breath sounds because they are generated in the bronchi (and trachea).
• Normal breath sounds. If you listen anywhere over the lung fields (including all of the zones shown in Fig. 3.3.2) the sounds are much quieter because you are over lung parenchyma and the air in the lungs has absorbed a lot of the sound. This attenuates the sound, making it smoother, gentler and more continuous, so it is harder to tell when inspiration changes to expiration. Since we expect to hear these sounds when auscultating over the lungs we call them ‘normal breath sounds’.
• Bronchial breathing (bronchial breath sounds heard over lung fields). If you are listening over the lungs and what you hear sounds loud, harsh and discontinuous (i.e. like bronchial breath sounds), it is not ‘normal’ and suggests that these sounds have not been dampened down by the air in the lungs – usually because in that area of lung the air has been replaced by something solid (consolidated). A solid area transmits sound very well because it vibrates more than air (ask the patient to say ‘99’ while auscultating and the sound will be very clear over consolidated lung tissue). These sounds may occur over an area of lobar pneumonia where the alveoli fill with clotted inflammatory exudate, or over collapsed lung tissue (occurring without a sputum plug), or at the lip of a pleural effusion.
• Breath sounds quieter than normal. If the breath sounds are very quiet it might be because the patient is very large and therefore the sounds have been dampened down by excess soft tissue. Make sure you press the stethoscope firmly to the chest wall and press through the adipose tissue to get the best sound transmission. It might, however, be because the breaths were quite small and not generating much turbulence. Perhaps the patient is not breathing very deeply? Does this fit with your observation and palpation? Is one side of the chest moving more than the other side?
| Turbulence in the large airways | |
Expiration louder and longer with pause between inspiration and expiration (sounds like Darth Vader) | If heard over lung fields, suggests: |
| May be due to: • Sounds filtered by pleura, chest wall (obese or muscular patients, pleural effusion, pneumothorax, haemothorax) |
• Absent breath sounds. A pleural effusion, sputum plugging or pneumothorax could prevent sounds from being heard by absorbing the sound completely before it can be transmitted to the chest wall.
• Breath sounds louder than normal. Loud breath sounds suggest more turbulence in the large airways. This is usually due to obstruction or narrowing of these airways, e.g. due to COPD. Narrower airways are harder to breathe through, so the patient may be working harder in order to breathe.
Table 3.3.3 Added sounds: crackles
| Crackles | Short, non-musical, popping sounds, fine or coarse | |
| Fine crackles | Atelectasis | |
| Intra-alveolar oedema | ||
| Secretions small airways | ||
| Coarse crackles | Obstruction more proximal and larger airways with sputum. May be inspiratory as well as expiratory | |
Table 3.3.4 Added sounds: wheezes
| Wheezes | Musical sounds due to vibration of wall of narrowed airway | |
| High pitched | Bronchospasm | |
| Low pitched | Sputum | |
| Localized | TumourForeign body | |
| Sounds like | Cause | |
|---|---|---|
| Pleural rub | ||
| Stridor | ! Alert medical staff as the patient’s airway is at great risk of compromise |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 ) levels and base excess (BE). Blood gases can also be taken from a venous or capillary sample.
) levels and base excess (BE). Blood gases can also be taken from a venous or capillary sample.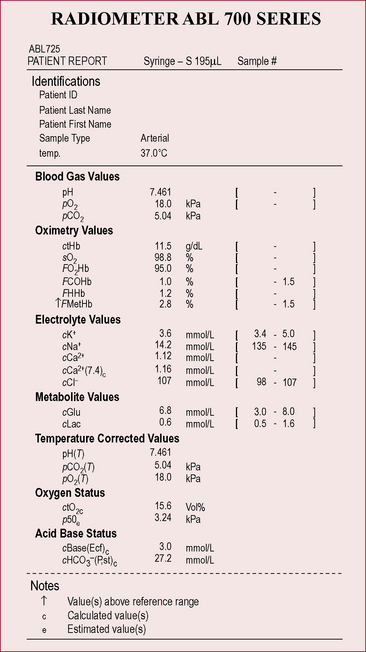
 above or below the average value of 24 mmol l−1
above or below the average value of 24 mmol l−1 (or BE)
(or BE) 14 mmol l−1
14 mmol l−1 30 mmol l−1
30 mmol l−1 move in the same direction as if in an elevator (e.g. if the pH is high the
move in the same direction as if in an elevator (e.g. if the pH is high the  will also be high).
will also be high). have moved in the opposite direction, this suggests that the metabolic system is compensating and the problem is respiratory.
have moved in the opposite direction, this suggests that the metabolic system is compensating and the problem is respiratory. 28
28 16
16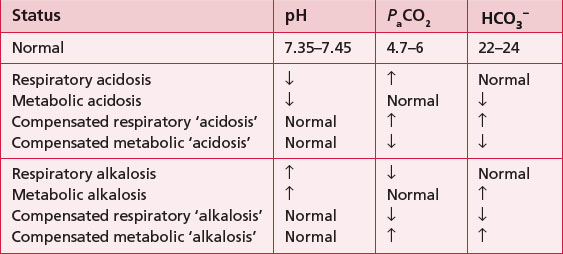
 24
24 22
22 32
32 3.5
3.5 to increase and his pH is within the normal range, despite his high PaCO2 (remember he is an ex-miner; therefore, respiratory disease would not be uncommon).
to increase and his pH is within the normal range, despite his high PaCO2 (remember he is an ex-miner; therefore, respiratory disease would not be uncommon). and therefore a fall in pH. There is some compensation because the PaCO2 has gone down, suggesting that he is breathing more in order to try and raise the pH. This is only partially successful because his pH is still below the normal range. Physiotherapy is not going to help his breathing at this point as he needs medical attention to stabilize his diabetes.
and therefore a fall in pH. There is some compensation because the PaCO2 has gone down, suggesting that he is breathing more in order to try and raise the pH. This is only partially successful because his pH is still below the normal range. Physiotherapy is not going to help his breathing at this point as he needs medical attention to stabilize his diabetes.